[1]
Thein SL. Molecular basis of β thalassemia and potential therapeutic targets. Blood cells, molecules & diseases. 2018 May:70():54-65. doi: 10.1016/j.bcmd.2017.06.001. Epub 2017 Jun 20
[PubMed PMID: 28651846]
[2]
Thein SL. The molecular basis of β-thalassemia. Cold Spring Harbor perspectives in medicine. 2013 May 1:3(5):a011700. doi: 10.1101/cshperspect.a011700. Epub 2013 May 1
[PubMed PMID: 23637309]
Level 3 (low-level) evidence
[5]
Weatherall DJ. The Evolving Spectrum of the Epidemiology of Thalassemia. Hematology/oncology clinics of North America. 2018 Apr:32(2):165-175. doi: 10.1016/j.hoc.2017.11.008. Epub
[PubMed PMID: 29458724]
[6]
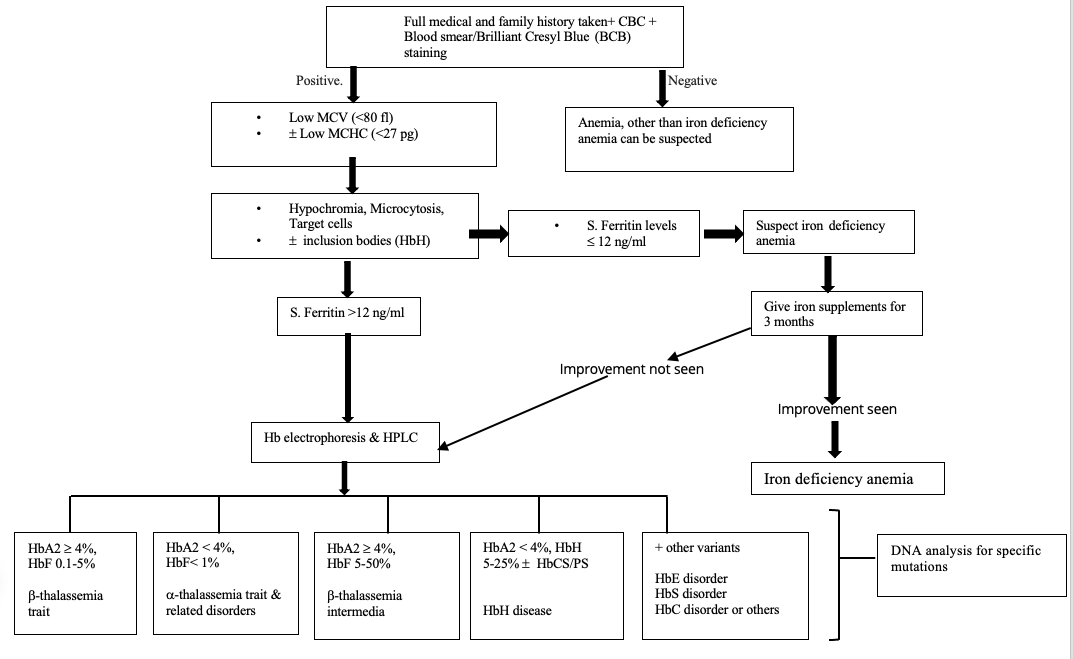
Munkongdee T, Chen P, Winichagoon P, Fucharoen S, Paiboonsukwong K. Update in Laboratory Diagnosis of Thalassemia. Frontiers in molecular biosciences. 2020:7():74. doi: 10.3389/fmolb.2020.00074. Epub 2020 May 27
[PubMed PMID: 32671092]
[7]
Rund D. Thalassemia 2016: Modern medicine battles an ancient disease. American journal of hematology. 2016 Jan:91(1):15-21. doi: 10.1002/ajh.24231. Epub
[PubMed PMID: 26537527]
[8]
Musallam KM, Rivella S, Vichinsky E, Rachmilewitz EA. Non-transfusion-dependent thalassemias. Haematologica. 2013 Jun:98(6):833-44. doi: 10.3324/haematol.2012.066845. Epub
[PubMed PMID: 23729725]
[9]
Piel FB, Weatherall DJ. The α-thalassemias. The New England journal of medicine. 2014 Nov 13:371(20):1908-16. doi: 10.1056/NEJMra1404415. Epub
[PubMed PMID: 25390741]
[10]
Poyart C, Wajcman H. Hemolytic anemias due to hemoglobinopathies. Molecular aspects of medicine. 1996 Apr:17(2):129-42
[PubMed PMID: 8813715]
[11]
He S, Li J, Huang P, Zhang S, Lin L, Zuo Y, Tian X, Zheng C, Qiu X, Chen B. Characterization of Hb Bart's Hydrops Fetalis Caused by - -(SEA) and a Large Novel α(0)-Thalassemia Deletion. Hemoglobin. 2018 Jan:42(1):61-64. doi: 10.1080/03630269.2018.1434198. Epub 2018 Mar 1
[PubMed PMID: 29493331]
Level 2 (mid-level) evidence
[12]
Pang W, Long J, Weng X, Fan Q, Sun L, Pan Z, Fan Z. Identification of Three Types of α-Thalassemia Deletion, -α(21.9), -α(2.4), and - -(THAI), and Their Frequencies, in One Family in the Population of Southern Guangxi Zhuang Autonomous Region, People's Republic of China. Hemoglobin. 2018 Jan:42(1):37-42. doi: 10.1080/03630269.2018.1428618. Epub 2018 Feb 15
[PubMed PMID: 29447013]
[13]
Williams TN, Weatherall DJ. World distribution, population genetics, and health burden of the hemoglobinopathies. Cold Spring Harbor perspectives in medicine. 2012 Sep 1:2(9):a011692. doi: 10.1101/cshperspect.a011692. Epub 2012 Sep 1
[PubMed PMID: 22951448]
Level 3 (low-level) evidence
[14]
Kalfa TA. Diagnosis and clinical management of red cell membrane disorders. Hematology. American Society of Hematology. Education Program. 2021 Dec 10:2021(1):331-340. doi: 10.1182/hematology.2021000265. Epub
[PubMed PMID: 34889366]
[15]
Bhat VS, Dewan KK, Krishnaswamy PR. The Diagnosis of α-Thalassaemia: A Case of Hemoglobin H -α Deletion. Indian journal of clinical biochemistry : IJCB. 2010 Oct:25(4):435-40. doi: 10.1007/s12291-010-0053-7. Epub 2010 Sep 14
[PubMed PMID: 21966120]
Level 3 (low-level) evidence
[16]
Viprakasit V, Limwongse C, Sukpanichnant S, Ruangvutilert P, Kanjanakorn C, Glomglao W, Sirikong M, Utto W, Tanphaichitr VS. Problems in determining thalassemia carrier status in a program for prevention and control of severe thalassemia syndromes: a lesson from Thailand. Clinical chemistry and laboratory medicine. 2013 Aug:51(8):1605-14. doi: 10.1515/cclm-2013-0098. Epub
[PubMed PMID: 23525874]
[17]
King AJ, Higgs DR. Potential new approaches to the management of the Hb Bart's hydrops fetalis syndrome: the most severe form of α-thalassemia. Hematology. American Society of Hematology. Education Program. 2018 Nov 30:2018(1):353-360. doi: 10.1182/asheducation-2018.1.353. Epub
[PubMed PMID: 30504332]
[18]
Giordano PC. Strategies for basic laboratory diagnostics of the hemoglobinopathies in multi-ethnic societies: interpretation of results and pitfalls. International journal of laboratory hematology. 2013 Oct:35(5):465-79. doi: 10.1111/ijlh.12037. Epub 2012 Dec 7
[PubMed PMID: 23217050]
[19]
Brancaleoni V, Di Pierro E, Motta I, Cappellini MD. Laboratory diagnosis of thalassemia. International journal of laboratory hematology. 2016 May:38 Suppl 1():32-40. doi: 10.1111/ijlh.12527. Epub 2016 May 16
[PubMed PMID: 27183541]
[20]
Hansson K, Schuring-Blom GH, Leschot NJ. The preserving of chorionic villi before establishing long-term cell cultures for cytogenetic analysis. Prenatal diagnosis. 1995 Nov:15(11):1067-9
[PubMed PMID: 8606886]
[21]
Old J, Henderson S. Molecular diagnostics for haemoglobinopathies. Expert opinion on medical diagnostics. 2010 May:4(3):225-40. doi: 10.1517/17530051003709729. Epub 2010 Mar 15
[PubMed PMID: 23488532]
Level 3 (low-level) evidence
[22]
Galanello R, Origa R. Beta-thalassemia. Orphanet journal of rare diseases. 2010 May 21:5():11. doi: 10.1186/1750-1172-5-11. Epub 2010 May 21
[PubMed PMID: 20492708]
[23]
Oyaert M, Van Laer C, Claerhout H, Vermeersch P, Desmet K, Pauwels S, Kieffer D. Evaluation of the Sebia Minicap Flex Piercing capillary electrophoresis for hemoglobinopathy testing. International journal of laboratory hematology. 2015 Jun:37(3):420-5. doi: 10.1111/ijlh.12305. Epub 2014 Oct 16
[PubMed PMID: 25324031]
[24]
Chong SS, Boehm CD, Higgs DR, Cutting GR. Single-tube multiplex-PCR screen for common deletional determinants of alpha-thalassemia. Blood. 2000 Jan 1:95(1):360-2
[PubMed PMID: 10607725]
[25]
Liu YT, Old JM, Miles K, Fisher CA, Weatherall DJ, Clegg JB. Rapid detection of alpha-thalassaemia deletions and alpha-globin gene triplication by multiplex polymerase chain reactions. British journal of haematology. 2000 Feb:108(2):295-9
[PubMed PMID: 10691858]
[26]
Rao S, Kar R, Gupta SK, Chopra A, Saxena R. Spectrum of haemoglobinopathies diagnosed by cation exchange-HPLC & modulating effects of nutritional deficiency anaemias from north India. The Indian journal of medical research. 2010 Nov:132(5):513-9
[PubMed PMID: 21150000]
[27]
Kunwandee J, Srivorakun H, Fucharoen G, Sanchaisuriya K, Fucharoen S. ARKRAY ADAMS A1c HA-8180T Analyzer for Diagnosis of Thalassemia and Hemoglobinopathies Common in Southeast Asia. Laboratory medicine. 2014 Summer:45(3):e112-21. doi: 10.1309/LMMH649POETQREXL. Epub
[PubMed PMID: 25217515]
[28]
Khera R, Singh T, Khuana N, Gupta N, Dubey AP. HPLC in characterization of hemoglobin profile in thalassemia syndromes and hemoglobinopathies: a clinicohematological correlation. Indian journal of hematology & blood transfusion : an official journal of Indian Society of Hematology and Blood Transfusion. 2015 Mar:31(1):110-5. doi: 10.1007/s12288-014-0409-x. Epub 2014 Jun 5
[PubMed PMID: 25548455]
[29]
Borbely N, Phelan L, Szydlo R, Bain B. Capillary zone electrophoresis for haemoglobinopathy diagnosis. Journal of clinical pathology. 2013 Jan:66(1):29-39. doi: 10.1136/jclinpath-2012-200946. Epub 2012 Oct 26
[PubMed PMID: 23105123]
[30]
Khongthai K, Ruengdit C, Panyasai S, Pornprasert S. Analysis of Deletional Hb H Diseases in Samples with Hb A(2)-Hb H and Hb A(2)-Hb Bart's on Capillary Electrophoresis. Hemoglobin. 2019 Jul-Sep:43(4-5):245-248. doi: 10.1080/03630269.2019.1683573. Epub 2019 Nov 5
[PubMed PMID: 31687860]
[31]
Suwannakhon N, Pangeson T, Seeratanachot T, Mahingsa K, Pingyod A, Bumrungpakdee W, Sanguansermsri T. Noninvasive prenatal screening test for compound heterozygous beta thalassemia using an amplification refractory mutation system real-time polymerase chain reaction technique. Hematology reports. 2019 Sep 18:11(3):8124. doi: 10.4081/hr.2019.8124. Epub 2019 Sep 18
[PubMed PMID: 31579144]
[32]
Qin J, He J, Li Y, Liu N, Tao F, Zhang P, Guo W, Qin Q, Zhou W. One-step genotyping of α-thalassaemia by multiplex symmetric PCR melting curve. Journal of clinical pathology. 2023 Sep:76(9):632-636. doi: 10.1136/jclinpath-2022-208363. Epub 2022 Jun 14
[PubMed PMID: 35701141]
Level 2 (mid-level) evidence
[33]
Green RC, Berg JS, Grody WW, Kalia SS, Korf BR, Martin CL, McGuire AL, Nussbaum RL, O'Daniel JM, Ormond KE, Rehm HL, Watson MS, Williams MS, Biesecker LG, American College of Medical Genetics and Genomics. ACMG recommendations for reporting of incidental findings in clinical exome and genome sequencing. Genetics in medicine : official journal of the American College of Medical Genetics. 2013 Jul:15(7):565-74. doi: 10.1038/gim.2013.73. Epub 2013 Jun 20
[PubMed PMID: 23788249]
[34]
Zhou YQ, Xiao GF, Li LY, Li WD, Liu ZY, Zhu LF, Mo QH, Qu XJ, Xu XM. Evaluation of clinical application of gap-PCR as a routine method for alpha-thalassemia carrier detection. Di 1 jun yi da xue xue bao = Academic journal of the first medical college of PLA. 2002 May:22(5):434-6
[PubMed PMID: 12390707]
[35]
Schouten JP, McElgunn CJ, Waaijer R, Zwijnenburg D, Diepvens F, Pals G. Relative quantification of 40 nucleic acid sequences by multiplex ligation-dependent probe amplification. Nucleic acids research. 2002 Jun 15:30(12):e57
[PubMed PMID: 12060695]
[36]
Slatko BE, Gardner AF, Ausubel FM. Overview of Next-Generation Sequencing Technologies. Current protocols in molecular biology. 2018 Apr:122(1):e59. doi: 10.1002/cpmb.59. Epub
[PubMed PMID: 29851291]
Level 3 (low-level) evidence
[37]
Emms A, Castleman J, Allen S, Williams D, Kinning E, Kilby M. Next Generation Sequencing after Invasive Prenatal Testing in Fetuses with Congenital Malformations: Prenatal or Neonatal Investigation. Genes. 2022 Aug 24:13(9):. doi: 10.3390/genes13091517. Epub 2022 Aug 24
[PubMed PMID: 36140685]
[38]
Kingchaiyaphum B, Sanchaisuriya K, Fucharoen G, Chaibunruang A, Hess SY, Hinnouho GM, Barffour MA, Wessells KR, Kounnavong S, Fucharoen S. Hemoglobins F, A(2) , and E levels in Laotian children aged 6-23 months with Hb E disorders: Effect of age, sex, and thalassemia types. International journal of laboratory hematology. 2020 Jun:42(3):277-283. doi: 10.1111/ijlh.13164. Epub 2020 Feb 12
[PubMed PMID: 32048804]
[39]
Todd D, Lai MC, Beaven GH, Huehns ER. The abnormal haemoglobins in homozygous alpha-thalassaemia. British journal of haematology. 1970 Jul:19(1):27-31
[PubMed PMID: 5465779]
[40]
Harteveld CL, Higgs DR. Alpha-thalassaemia. Orphanet journal of rare diseases. 2010 May 28:5():13. doi: 10.1186/1750-1172-5-13. Epub 2010 May 28
[PubMed PMID: 20507641]
[41]
Curran M, Mikhael M, Sun WD, Lim J, Leung A, Morchi G, Chmait RH. Perinatal Management of Bart's Hemoglobinopathy: Paradoxical Effects of Intrauterine, Transplacental, and Partial Exchange Transfusions. AJP reports. 2020 Jan:10(1):e11-e14. doi: 10.1055/s-0039-3401799. Epub 2020 Jan 27
[PubMed PMID: 31993246]
[42]
Songdej D, Babbs C, Higgs DR, BHFS International Consortium. An international registry of survivors with Hb Bart's hydrops fetalis syndrome. Blood. 2017 Mar 9:129(10):1251-1259. doi: 10.1182/blood-2016-08-697110. Epub 2017 Jan 5
[PubMed PMID: 28057638]
[43]
Ghosh K, Colah R, Manglani M, Choudhry VP, Verma I, Madan N, Saxena R, Jain D, Marwaha N, Das R, Mohanty D, Choudhary R, Agarwal S, Ghosh M, Ross C. Guidelines for screening, diagnosis and management of hemoglobinopathies. Indian journal of human genetics. 2014 Apr:20(2):101-19. doi: 10.4103/0971-6866.142841. Epub
[PubMed PMID: 25400338]
[44]
Torcharus K, Sriphaisal T, Krutvecho T, Ketupanya A, Vuthiwong C, Suwanasophon C, Noonai A. Prenatal diagnosis of Hb Bart's hydrops fetalis by PCR technique: Pramongkutklao experience. The Southeast Asian journal of tropical medicine and public health. 1995:26 Suppl 1():287-90
[PubMed PMID: 8629126]
[45]
Dame C, Albers N, Hasan C, Bode U, Eigel A, Hansmann M, Brenner R, Bartmann P. Homozygous alpha-thalassaemia and hypospadias--common aetiology or incidental association? Long-term survival of Hb Bart's hydrops syndrome leads to new aspects for counselling of alpha-thalassaemic traits. European journal of pediatrics. 1999 Mar:158(3):217-20
[PubMed PMID: 10094442]
[46]
Fenta DA, Ali MM. Factors Affecting Quality of Laboratory Result During Ordering, Handling, and Testing of the Patient's Specimen at Hawassa University College of Medicine and Health Science Comprehensive Specialized Hospital. Journal of multidisciplinary healthcare. 2020:13():809-821. doi: 10.2147/JMDH.S264671. Epub 2020 Aug 18
[PubMed PMID: 32922023]
Level 2 (mid-level) evidence
[47]
Kinns H, Pitkin S, Housley D, Freedman DB. Internal quality control: best practice. Journal of clinical pathology. 2013 Dec:66(12):1027-32. doi: 10.1136/jclinpath-2013-201661. Epub 2013 Sep 26
[PubMed PMID: 24072731]
Level 2 (mid-level) evidence
[48]
Laudus N, Nijs L, Nauwelaers I, Dequeker EMC. The Significance of External Quality Assessment Schemes for Molecular Testing in Clinical Laboratories. Cancers. 2022 Jul 28:14(15):. doi: 10.3390/cancers14153686. Epub 2022 Jul 28
[PubMed PMID: 35954349]
Level 2 (mid-level) evidence
[49]
Skitek M, Martinello F, Jerin A. How to Really Understand and Improve the System of Internal Quality Control and External Quality Assessment in the Accreditation Process of the Medical Laboratory? EJIFCC. 2022 Apr:33(1):23-27
[PubMed PMID: 35645692]
Level 2 (mid-level) evidence
[50]
Lock RJ. My approach to internal quality control in a clinical immunology laboratory. Journal of clinical pathology. 2006 Jul:59(7):681-4
[PubMed PMID: 16803947]
Level 2 (mid-level) evidence
[51]
Petersen PH, Ricós C, Stöckl D, Libeer JC, Baadenhuijsen H, Fraser C, Thienpont L. Proposed guidelines for the internal quality control of analytical results in the medical laboratory. European journal of clinical chemistry and clinical biochemistry : journal of the Forum of European Clinical Chemistry Societies. 1996 Dec:34(12):983-99
[PubMed PMID: 8986407]
Level 2 (mid-level) evidence
[52]
Abu-Siniyeh A, Al-Shehri SS. Safety in Medical Laboratories: Perception and Practice of University Students and Laboratory Workers. Applied biosafety : journal of the American Biological Safety Association. 2021 Sep:26(Suppl 1):S34-S42. doi: 10.1089/apb.20.0050. Epub 2021 Sep 13
[PubMed PMID: 36032652]
[54]
Cornish NE, Anderson NL, Arambula DG, Arduino MJ, Bryan A, Burton NC, Chen B, Dickson BA, Giri JG, Griffith NK, Pentella MA, Salerno RM, Sandhu P, Snyder JW, Tormey CA, Wagar EA, Weirich EG, Campbell S. Clinical Laboratory Biosafety Gaps: Lessons Learned from Past Outbreaks Reveal a Path to a Safer Future. Clinical microbiology reviews. 2021 Jun 16:34(3):e0012618. doi: 10.1128/CMR.00126-18. Epub 2021 Jun 9
[PubMed PMID: 34105993]