Continuing Education Activity
Corneal topography is an integral diagnostic tool in the armamentarium of the cornea, cataract, and refractive surgeons. This activity highlights the evolution of corneal topographic mapping and the methods of evaluating the anterior and posterior surfaces of the cornea. The radius of curvature of the central part of the anterior surface of the cornea is measured by the size of the reflection of an image projected by the keratometer. The differences between topography and tomography, the indications, techniques, and topography machines are described. The roles of topography in the diagnosis, as well as the progression of corneal ectasias and pre and post-operative evaluation in refractive procedures, are summarized.
Objectives:
- Describe the different techniques of corneal topography, including Placido disc, slit scanning, and Schiempflug imaging.
- Review the indications and the importance of corneal topography in pre-refractive surgery screening.
- Summarize the clinical significance of corneal topography in diagnosing various corneal disorders.
- Outline the role of corneal topography in clinical practice and discuss the role of interprofessional collaboration in delivering optimal care to patients to improve visual outcomes.
Introduction
The healthy central cornea is aspheric and prolate (the central curvature is steeper than the periphery).[1] Attempts to measure the cornea were made as early as the 1600s by Scheiner, who compared reflections produced by glass spheres whose diameters were known to the reflections from the anterior surface of the cornea.[2] The central keratometric values vary between 40 D to 47 D (mean 43D).[1] The standard keratometry device measures two points at a 2.25-4 mm zone in the central cornea.[3][4]
The radius of curvature of the central part of the anterior surface of the cornea is measured by the size of the reflection of an image projected by the keratometer using the formula r=2uI/o or the radius of curvature= 2 x distance between the reflective surface and the object x image size /object size (r=radius of curvature, u=distance between the reflective surface and the object, I=image size, and o= object size).[3][5]
The different keratometers, such as the Javal Schiotz and the Bausch and Lomb keratometer, were adequate to calculate the dioptric power of the cornea for intraocular lens power calculation and contact lens fitting. However, with increased keratorefractive procedures, the evaluation of paracentral and peripheral cornea is of increased significance. The Placido ring was the first instrument used to analyze the anterior surface of the cornea.[1][6] Then, computerized videokeratography (CVK) was developed to map the corneal power and shape.
Principles of topography - A luminous object is projected onto the cornea, and its reflection is analyzed. The methods of topography include
- Placido method,
- Slit scanning technique, and
- Schiempflug method.
The Placido method analyzes only the anterior surface of the cornea, whereas the other two methods also map the posterior corneal surface and measure the corneal thickness. The Placido method involves projecting a series of concentric black and white rings onto the cornea and capturing their reflection by a camera placed in the center of the rings. This is the first Purkinje reflex. The power of the central 3 mm of the cornea is extrapolated, resulting in the Sim (simulated) K (keratometry) values. The rings are centered on the visual axis and not the pupil. The distance between the visual axis and the center of the pupil is the angle kappa (K). Algorithms calculate the power of the cornea at each point depending on the deformation of the mires. The Placido-based topography measures the refractive status of the cornea accurately but does not, however, reflect the true shape of the cornea.
Corneoscope and corneopter: This Placido-based device projects black and white mires on the cornea. Then a black and white or a color polaroid photograph is taken at 4.8 X magnification.[7] The dioptric power, and the radius of curvature at a particular point, are read by comparing the amount of magnification needed to match the photographed rings to a standard set of rings on the comparator screen. The steeper the cornea, the closer the rings. Variations between the normal cornea, pseudocones, suture-induced astigmatism, and true keratoconus can be recognized.[7]
The commonest causes of pseudocones are pellucid marginal degeneration, contact lens-induced irregular astigmatism, and corneal or limbal trauma. The corneal power is inversely related to the area which can be examined. A larger area of a flatter cornea can be examined compared to a steep cornea.
The slit scanning technology is based on measuring the dimensions of a slit scanning beam projected on the cornea.[2] Orbscan initially was only a slit scanning technology to measure corneal thickness as well as curvature of the anterior and posterior surfaces of the cornea. Elevation information was acquired directly, and curvature information was derived from this. Orbscan II incorporated a Placido disc attachment to get curvature measurements directly. The Orbscan IIz is a further improvement because it incorporates the Shack-Hartmann aberrometer in the Zyoptix workstation.[8]
The reflection of the illuminated Placido disc onto the cornea is stored, followed by the projection of 40 slits, 20 from the right and the left (each slit 12.5 mm high x 0.30 mm wide) at an angle of 45 degrees to the instrument axis. The backscattered images are captured by the device's video camera. Acquisition of images is followed by assessment of images and compensation for eye movements by a proprietary technique. Processing of the data is done by the machine to construct the anterior and posterior elevation maps and the curvature maps.
The Schiempflug technology uses a rotating camera to capture the reflection of a bright slit beam that sweeps across the cornea.[1] A 3-D reconstruction of the anterior and posterior elevation is done, and the pachymetry is calculated. The Schiempflug principle is credited to Theodore Schiempflug, who devised a method to correct distortion in aerial photography.[1][9][10][11][12] A single rotating camera and static camera are present in the Pentacam device.[12][9]
The Schiempflug and the Placido-based technologies are combined in machines like the Sirius, TMS 5, and Galilei.[13] The Galilei machine uses two rotating cameras (dual Schiempflug analyzer), whereas the pentacam has a single rotating camera.
Tomography vs. Topography
A topographer analyzes only the front surface of the cornea. Tomography is derived from the word "Tomos " (Greek for cut or section) and "graphein" (to write). A 3-dimensional image of the anterior and posterior surface of the cornea and corneal thickness is measured as opposed to topography, where only the anterior surface of the cornea is mapped.[9][10]
Tear film analysis is possible with the Placido-based systems. Non-invasive tear film break-up time (NITBUT) can be measured for various purposes by Placido-based topographers or by Placido disc alone.[14] Projecting rings on the corneal surface and measuring the time to break or distortion of the mires can effectively measure the tear film break-up time.
Procedures
Corneal topography, whether Placido based or slit scanning, or a combination of the two techniques, involves placing the patient's chin on the chin rest of the machine, asking the patient to focus on a fixation light, and capturing the image of the Placido mires and /or the slit beam by means of a camera and the machine automatically calculates the dioptric power across the corneal surface.[6] The Placido-based devices calculate the radius of curvature and, thereby, the dioptric power of the central and paracentral cornea and extrapolate the data in the peripheral cornea.
Different indices are incorporated in the various devices to enable the prediction of ectasias, such as the Rabinowitz indices or the Klyce Maeda indices.[15]
The slit scanning devices such as Orbscan and the Schiempflug-based devices such as the Oculus pentacam have faster acquisition times which means lesser problems with the eye movement of patients during acquisition. The tear film has a major role to play in corneal topography maps. It is preferred to remove soft lenses a week before and rigid gas permeable lenses two weeks before doing corneal topography to avoid contact lens-induced warpage.[16][17][18]
Indications
Corneal topography and tomography maps display the size, shape, and power of the cornea's anterior and posterior surface and the cornea's thickness in various locations. Topography maps are essential for the following:
Screening for refractive surgery: Normative data have been established for various topographers. Placido-based topographers give data only for the anterior corneal surface.
An example is a TMS-4N topographer (Tomey) which has 25 rings with 256 measurement points on a ring, and it can measure a maximum of 6400 measurement points. The Sim K values reflect the values derived by keratometric devices.[19]
Color maps make it easier to identify steeper and flatter areas of the cornea. Warmer colors indicate steeper and cooler colors indicate flatter keratometry.[20] Various maps are used by topographers to identify different patterns. Axial maps using a mid-dioptric green value show certain patterns such as circular, symmetric bowtie, asymmetric bowtie, and irregular patterns.[19]
Topographic indices have been established in Placido-based topographers and Slit scanning and Schiempflug-based tomography machines to identify candidates who are fit for laser refractive procedures. Artificial intelligence-based systems have recently been used to detect the early onset of keratoconus.[21]
Detection of corneal ectasia: Pentacam-based systems provide the indices, including the following:
- Index of surface variance (ISV)
- Keratoconus index (KI)
- Central keratoconus index (CKI)
- Index of height decentration (IHD)
- The minimum radius of curvature (R min)
- Index of vertical asymmetry (IVA)
- Index of height asymmetry (IHA)
These indices have high sensitivity and specificity for distinguishing keratoconus from normal corneas.[22][23][24]
Concept of "enhanced reference surface": A reference is devised which resembles a normal portion of the patient's own cornea, and the enhanced reference surface is generated using the diameter of the best fit sphere but excluding the area of ectatic protrusion. A 3.5 mm zone centered on the ectatic area is the exclusion zone.[24] By doing this, the ectatic area is further enhanced.
Contact lens fitting: The role of corneal topography in contact lens fitting in normal and keratoconic corneas has been studied in the last two decades. Corneal topography maps may guide the initial diagnostic lens used for the contact lens trial. In keratoconic corneas, the role of corneal topography for rigid gas permeable lens or Rose K lens fitting is more than in normal corneas.[25][26][27]
Progression of ectatic disorders: Amongst the ectatic disorders, keratoconus is the most common. The Amsler-Krumeich classification is most commonly used to grade its severity.[28][29] In this classification, central keratometry, spectacle refraction, presence or absence of scarring, and central corneal thickness are considered for grading the severity of keratoconus from grade1 to grade 4. Several modifications have been made to this classification.[28][29]
Planning placement of intracorneal ring segments: Intracorneal ring segments are essentially made of polymethyl methacrylate and are placed in the corneal stroma to flatten the cornea and ensure lesser aberrations and decrease corneal irregularity.
Placement of these ring segments can be done after making a channel in the corneal stroma either manually or with a femtosecond laser. The location and depth of the channels are mainly guided by corneal tomography and by the manufacturer's nomograms. Postoperatively, the effect of the ring segments is analyzed by changes in the corneal topography.[30][31][32][33]
Planning arcuate incisions: In a study by Koffler, 21 eyes with high post-operative astigmatism after penetrating keratoplasty were treated with arcuate incisions, which were guided by the topography maps.[34] On average, the astigmatic cylinder was reduced by 5.3 D, and an overall 56% reduction was noted in corneal astigmatism. The Femtosecond laser was also used to make arcuate incisions to correct high astigmatism after penetrating keratoplasty.[35] Though this study was about the role of femtosecond lasers in making arcuate incisions, the role of corneal topography in guiding the placement of these incisions is also emphasized.
Diagnosis of subclinical corneal edema in Fuchs endothelial corneal dystrophy: Fourier analysis of cases of Fuchs' endothelial dystrophy by anterior segment optical coherence tomography in 75 eyes of 43 patients showed anterior and posterior flattening in the inferior cornea up to grade 5 and irregularity of the anterior and posterior surfaces in grade 6.[36]
Schiempflug tomography posterior elevation and pachymetry maps can detect subclinical corneal edema in early Fuchs endothelial dystrophy and can be an important diagnostic tool.[36][37][38][39]
Change in corneal curvature after pterygium excision and excision of limbal dermoid: Changes in corneal curvature after excision of pterygium with or without conjunctival autograft and after excision of limbal dermoid can be accurately assessed by corneal topography.[1]
Other Indications of Corneal Tomography
Pachymetry maps, anterior and posterior elevation maps, white-to-white diameter measurements, anterior chamber depth, lens thickness, and ectasia progression indices are additional information given by the slit scanning and Schiempflug technologies.
Pachymetry maps give an indication of corneal thickness across the cornea. Location of the thinnest area, if paracentral, may be an early indication of ectasia. The thinnest and steepest areas, if they coincide, are another indicator of ectasia.
Elevation maps in Schiempflug tomography are calculated based on a best-fit sphere (BFS) or a best-fit toric ellipsoid (BFTE).
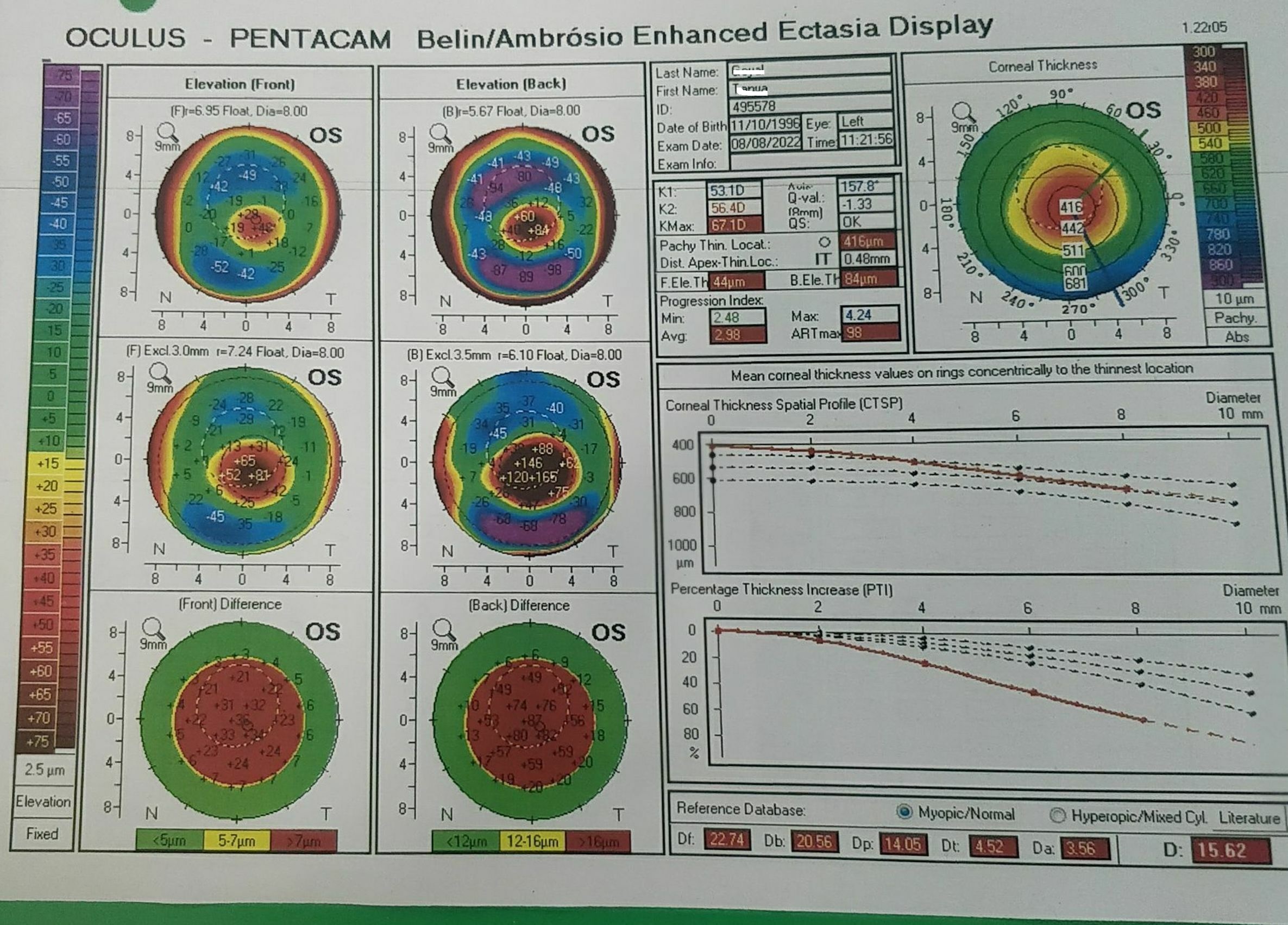
The Belin-Ambrosio ectasia (BAD) display shows several parameters which may be indicators of ectasia.[24] It uses anterior and posterior elevation, pachymetric progression, relational thickness, and the thinnest corneal point. A value of BAD less than 1.6 standard deviations (SD) from the mean is normal, and ≥ 2.6 SD is pathologic.
Potential Diagnosis
Various conditions can be diagnosed by corneal topography, including forme fruste keratoconus, keratoconus, pellucid marginal degeneration, Terrien marginal degeneration, post-refractive surgery ectasia; and keratoglobus.[20] Planned suture removal after penetrating and deep anterior lamellar keratoplasty is aided by corneal topography. The steep axis is identified by the topography maps. The diagnosis of each of these conditions is discussed further under clinical significance.
Normal and Critical Findings
All topographic and tomographic machines have normative data in the system. Additional indices for ectasia, such as the Klyce Maeda and the Rabinowitz indices, are included in the Placido-based systems. The tomographic maps have further been evaluated and analyzed by the Belin-Ambrosio display(BAD-D) and the ABCD progression maps.[9][40][9]
Different Indices and Their Normal Range in Topographic Maps
Indices for Placido-based Topography
- Central K reading (K): <47.2 D (>7.2mm)
- Average Corneal Power (ACP): 40.5 to 46.7 D
- Inferior - Superior Asymmetry (IS): <1.4
- Corneal Asymmetry Index (CAI) positive for prolate surface, negative for oblate surface: -0.114 to 0.806
- Standard Deviation of Power (SDP): 0.37 to 1.33
- Differential Sector Index (DSI): 0.21 to 3.51
- Opposite Sector Index (OSI): -0.55 to 2.09[41]
- Center Surround Index (CSI): -0.28 to 0.80
- Irregular Astigmatism Index (IAI): 0.19 to 0.49
- Surface Asymmetry Index (SAI): 0.10 to 0.42
- Surface Irregularity Index (SRI): 0 to 0.56
- Area Analyzed (AA): 0.70 to 0.94[41]
Indices in Orbscan
- The ratio between the radius of the anterior best fit sphere (BFS) and posterior best fit sphere (BFS): 1.21 or less is normal; 1.22-1.27 is suspect for ectasia.
- Power of posterior BFS up to 55 D is normal, and >55 D is suspect for ectasia.
- CTI (corneal thickness index): CTI up to 1.16 is normal, and CTI >1.16 is ectasia suspect.
- Irregularity in the 3 mm zone up to 1.15 D is normal, and > 1.15 D is suspect.
- Irregularity in the 5 mm zone up to 2.5 D is normal, and > 2.5 D is suspect.[42]
Indices in Schiempflug-based Corneal Tomography
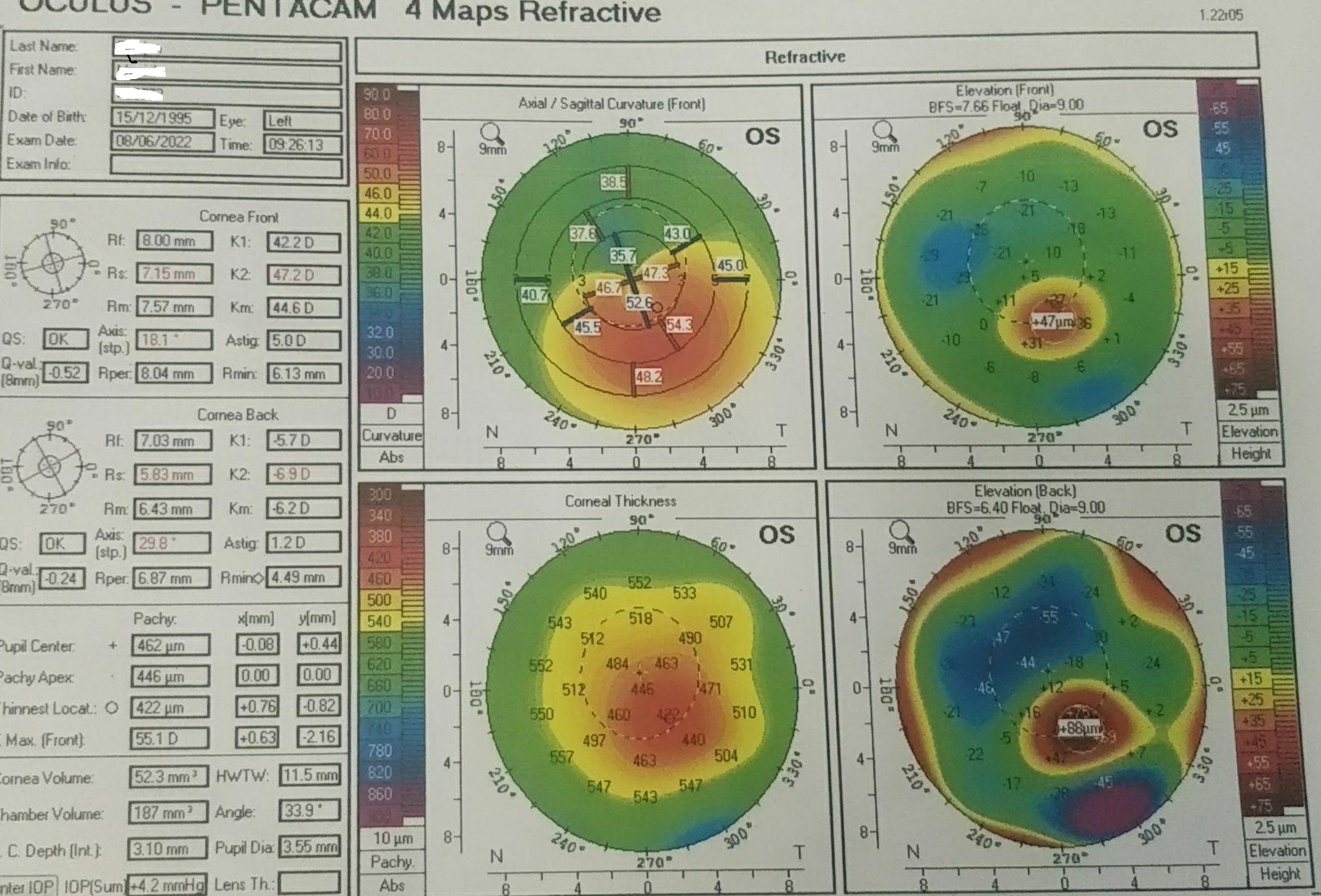
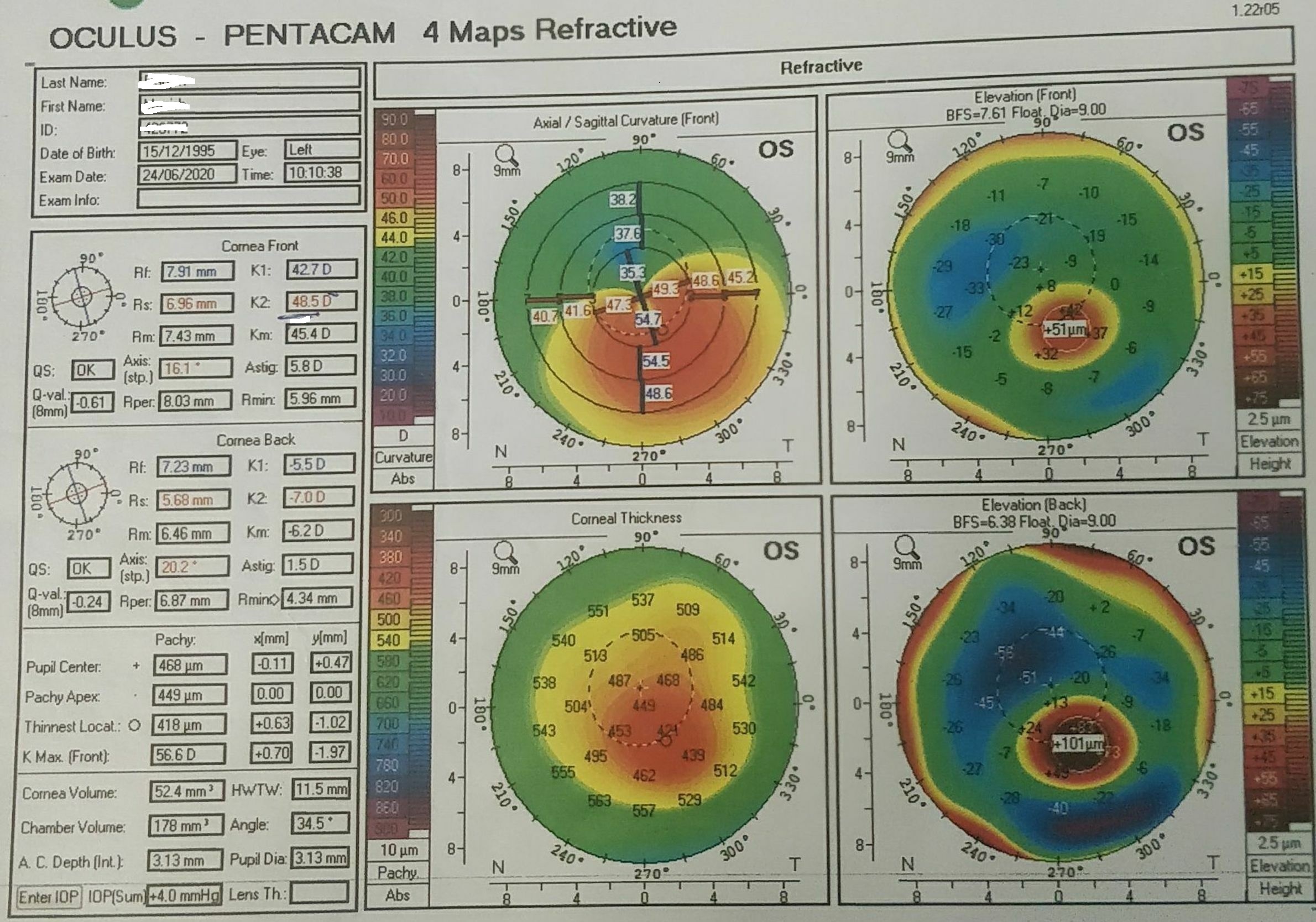
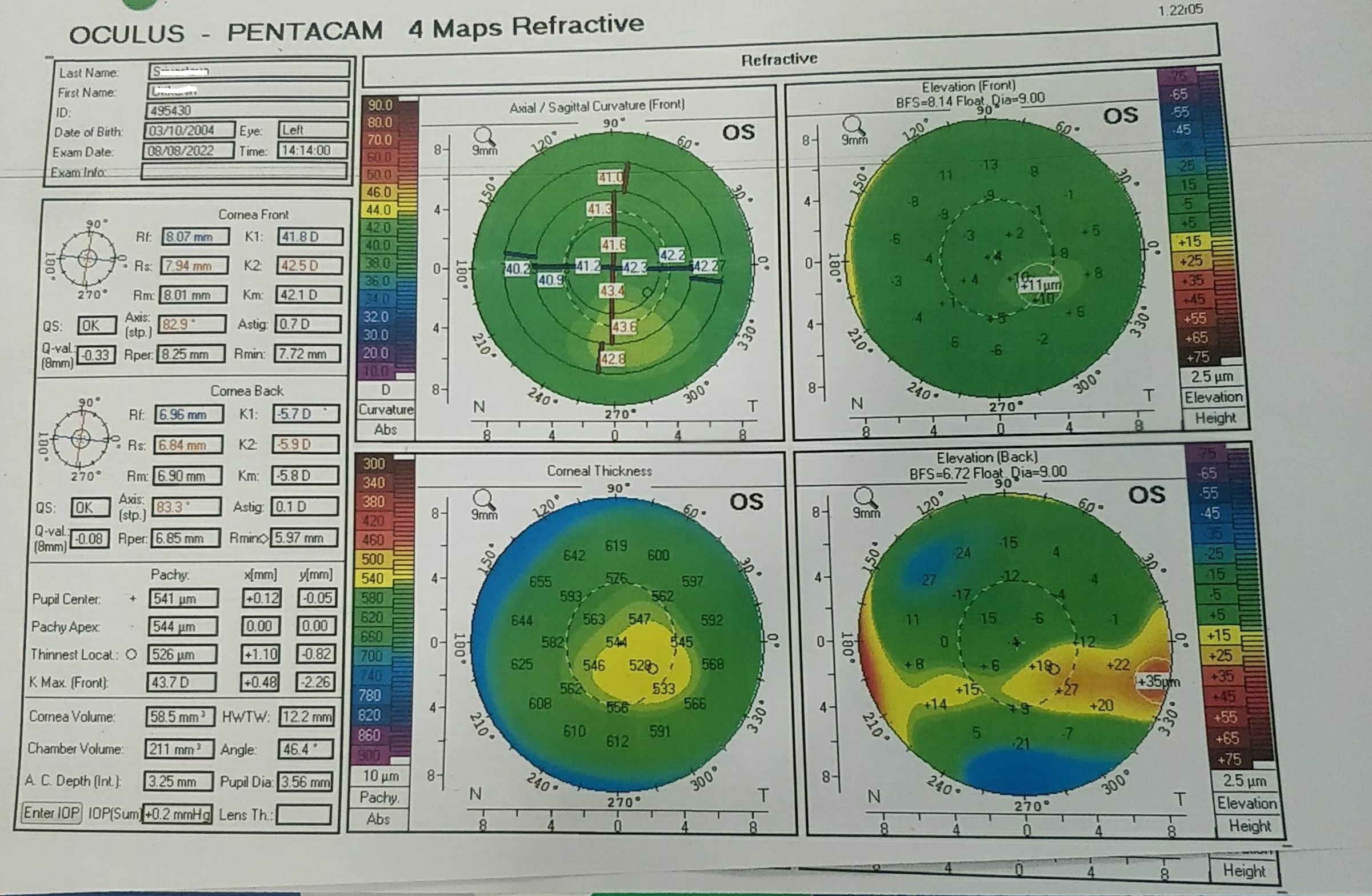
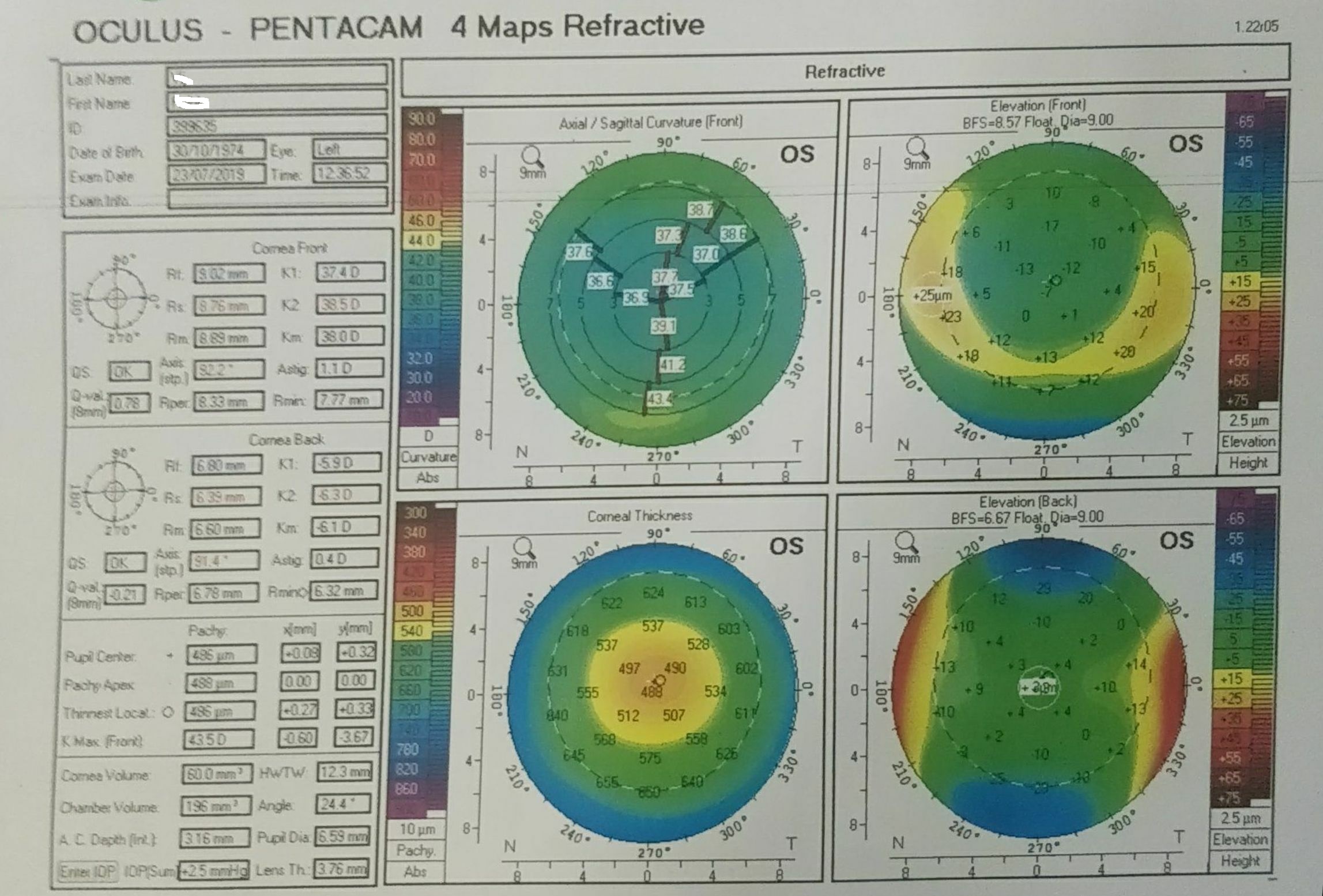
Four maps are displayed together in a Pentacam image. Four Map Refractive is the most commonly used display (Figure). Here one map displays the front axial or sagittal curvature, similar to the Placido display. The second map in this four-map display is the pachymetric map. Anterior and posterior elevation maps are the remaining two maps. The anterior and posterior elevation maps are based on the best-fit sphere. Use of best fit toric ellipsoid is done under some circumstances.[24][19]
Axial or sagittal map: It is a two-dimensional image that shows the dioptric power/radius of curvature of the cornea in the central, paracentral and peripheral cornea up to 9 mm. Warm colors like orange and red denote steepening, and cooler colors like blue and green suggest flattening. Corneal power (keratometry) can also be shown as the radius of curvature. The axial or sagittal map is similar to the maps seen on Placido-based systems. Normal corneas are green throughout, with gradual flattening from center to periphery.[24][19]
Pachymetry map shows corneal thickness in various areas up to 9 mm. The thicker areas are depicted in cooler colors, and the thinner areas in warmer colors.
Elevation maps: The difference between the examined anterior or posterior corneal surface and a standard reference shape 8 mm best fit sphere (BFS) or best fit toric ellipsoid (BFTE) is depicted as the elevation map.[43] Areas above the BFS and BFTE are represented by warmer colors and the areas below by cooler colors. Anterior and posterior elevation of the cornea is mapped relative to a standard reference shape such as a sphere or a toric ellipsoid. Posterior elevation may occur very early during the process of ectasia.
Interfering Factors
Tear film abnormalities and contact lens wear can alter corneal topography maps. In addition, the patient's eye movements, ptosis, and improper placement of the patient's head on chin rest can cause problems in data acquisition.
Comparison between topography maps of the same patient cannot be made between devices. K1, K2, and sim K astigmatism may not be the same across all devices.
There are several indices that are unique to a particular device. K max, for instance, is measured by Schiempflug tomography and not by Orbscan or Placido-based instruments.
Instilling fluorescein or mydriatic drops significantly affected the pachymetry at the pupillary center by 17+/- 53 microns in a study involving 131 eyes of 131 patients who had pentacam analysis before and after instilling either fluorescein, mydriatics, or both.[44] However, corneal shape measurements of anterior or posterior corneal surfaces were not affected. It is recommended to do corneal topography before any other tests to get an accurate assessment
Displaced apex syndrome: Asymmetric bowtie pattern can be produced due to astigmatism in a completely normal eye when the curvature reference axis does not pass the corneal apex. Placido-based topography may label such eyes as ectatic, but these eyes have a best-corrected visual acuity (BCVA) of 20/20, normal pachymetry, and orthogonal astigmatism and have good results after refractive surgery.[24] Elevation maps will be able to confirm such eyes as normal astigmatic eyes.
Patient Safety and Education
Topography is essential to screen and plan for refractive procedures, especially photorefractive keratectomy (PRK), LASIK (Laser in situ keratomileusis), arcuate keratotomy, and intracorneal ring segments. It is important to advise patients to undergo serial topographies in suspected ectasias to monitor progression and to diagnose post-refractive regression and ectasia.
Cataract surgery in patients with prior LASIK, radial keratotomy, or PRK needs topography to calculate intra-ocular lens power accurately. Corneal astigmatism measurement in the case of toric IOL (intraocular lens) power calculation also needs corneal topography. Patients must be educated about corneal topography's importance in these situations.
The optometrists and technicians operating the topography machines must be trained to advise the patients about the procedure. They have to be educated regarding the need to discontinue contact lens wear well before undergoing topography. Tear film abnormalities also have to be identified. Otherwise, the maps may be inaccurate. Proper positioning of the patient's forehead and chin on the machine and reduced or no blinking and eye movements must be explained.
Topography and tomography are essentially safe procedures and can be repeated as often as required.
Clinical Significance
Screening for Keratoconus: Keratoconus is a progressive noninflammatory ectatic disorder. It is the most commonly encountered corneal ectasia in clinical practice. Clinical diagnosis may be made by frequent changes of glasses, shadowing around letters, and poor vision, even with spectacle correction. It is objectively characterized by scissoring during retinoscopy and in later stages by apical scarring, stromal striae (Vogt striae), and bulging of the lower lid on down gaze (Munson sign). In later stages, the Descemet membrane may split, leading to corneal edema (hydrops).[45]
Rabinowitz established specific criteria to diagnose keratoconus, which were modified to include the following criteria: dioptric power > 47 D, irregular corneal curvature (asymmetric bowtie), and inferior-superior index >1.4 D.[46] An average of five points in each hemi-meridian which are 3 mm from the center and at 30-degree intervals are compared between the superior and inferior hemi-meridians.[47]
Amsler-Krumeich classification system grades keratoconus from 1 to 4 based on spectacle refraction, central corneal thickness, presence or absence of scarring, and central keratometry.[28] Several modifications to this system have been proposed.
Videokeratographic indices to detect keratoconus even before clinical signs were incorporated into software systems by Rabinowitz and Klyce-Maeda.[48][49] The TMS 1 topographic system has software incorporated with eight quantitative indices for each topographic map to identify keratoconus, and it assigns an index that is expressed as a percentage to assess the severity of Keratoconus (KCI). This system could distinguish keratoconus from other ectasias with a false negative rate of 2 in 130 and a false positive rate of 1 in 43.[45] Forme fruste keratoconus, subclinical keratoconus, keratoconus suspect, and preclinical keratoconus are all terms used when keratoconus is not established clinically.
Forme fruste was identified as the apparently normal "other" (fellow) eye of a patient with one eye diagnosed as keratoconus.[50] Stable refraction and normal corneal curvature in such cases may be associated with asymmetric bow tie patterns on topography. On the other hand, the absence of scissoring on retinoscopy, with an asymmetric bowtie pattern with a skewed radial axis (AB/SRAX), has been identified as a keratoconus suspect.[50]
Using the Pentacam system, the Belin Ambrosio enhanced ectasia display (BAD-D), diagnosis, and progression of keratoconus are made more accurate.
Other indices which are recommended are the following:
- Ambrósio Relational Thickness (ART) values,
- the index of vertical asymmetry (IVA),
- pachymetric progression indices (PPI).
- Keratoconus index (KI) is the ratio between the mean radius of curvature values between upper and lower segments.KI can distinguish normal from clinical keratoconus.
- The index of height decentration (IHD) is the degree of centration in the vertical direction.
- The index of vertical asymmetry (IVA), the level of curvature symmetry with respect to the horizontal meridian, is given by this data.[51] This index may be a strong predictor in pre-keratoconus cases.[52]
- The index of height asymmetry (IHA) is another important parameter.[52]
- The index of surface variance (ISV) is the deviation of the corneal radius as compared to the mean value. ISV may be useful for tracking progression.
- Index of vertical asymmetry (IVA), the level of curvature symmetry with respect to the horizontal meridian, is given by this data.[51] This index may be a strong predictor in pre-keratoconus cases.[52]
- Minimal sagittal curvature (R min) is the minimum radius of curvature that corresponds to the maximum anterior curvature. It has high correction with the best spectacle-corrected visual acuity.[29]
- Posterior elevation maps are considered superior to anterior elevation maps in detecting subclinical keratoconus.[50] While anterior elevation maps show frank keratoconus, posterior maps detect subclinical keratoconus.[46][53][54]
Minimal sagittal curvature (R min) is the minimum radius of curvature that corresponds to the maximum anterior curvature. The enhanced best fit sphere is a concept introduced by Belin wherein a 3.5 mm diameter zone centered around the thinnest area is excluded.[55] This removes the influence of the area around the thinnest point, which would otherwise cause a steepening effect.
Progression of Keratoconus: Several indices measure the progression of keratoconus. An increase in values of anterior and posterior K1 and K2, progressive thinning, and an increase in anterior and posterior elevation are all signs of progression. However, certain indices have been proposed to be more reliable such as the pachymetry progression index (PPI).[47]
Screening for refractive surgery: The main aim of screening candidates for refractive surgery is to identify those at risk for post-surgery ectasia. To identify pre-keratoconus, subclinical keratoconus, or forme fruste keratoconus, several classification systems, indices, and criteria have been formulated, such as the collaborative and longitudinal evaluation of keratoconus (CLEK) criteria, keratoconus index (KCI) and keratoconus prediction index (KPI) by Klyce-Maeda, and the Ectasia Risk Score system (ERSS) by Randleman et al.[47][56]
Corneal topographic patterns and pachymetry are still considered the cornerstone in screening candidates for laser refractive procedures. Corneal mechanical strength and collagen mapping are recent additions to the armamentarium.[57]
The following indices have been recommended by Motlagh et al. as the most effective for the detection of pre-keratoconus: Belin-Ambrósio Enhanced Ectasia Display Total Deviation Value (BAD_D), pachymetry progression index (PPI), Ambrósio relational thickness (ART) values, and the index of vertical asymmetry (IVA).[56]
Contact lens fitting and contact lens warpage: Contact lens fitting software was incorporated even in Placido-based topographers such as Eye-Sys. Topographic maps can show the central and peripheral radius of curvature, unlike the keratometers, which show only central curvatures.[16][17] Contact lens fitting can be made more accurate by referring to topographic maps.[16][17][18]
Short-term discontinuation of soft contact lenses did not interfere much with corneal topography measurement.[17] However, warpage due to rigid gas permeable lenses may occur and confuse the topographic maps unless they are discontinued for several weeks.
Placing intracorneal ring segments: Topographic maps, along with pachymetric maps, assist in calculating the placement and depth of intracorneal ring segments. Postoperatively, the flattening of the cornea is also measured by the topographic maps.[58]
Placement of arcuate incisions: The steeper axis is identified by topographic maps after penetrating or lamellar keratoplasty or even for placing arcuate incisions in Femto laser cataract surgery and limbal relaxing incisions in cataract surgery (LRI). The topographic maps also dictate the extent of the arc of incision and depth.[59]
Predictors of post-refractive surgery ectasia: Ectasia risk score system devised by Randleman et al.[56] An analysis of 50 eyes that developed ectasia post-LASIK and 50 eyes that did not develop ectasia was done.[56] Preoperative risk factors analyzed were age, gender, preoperative manifest refraction spherical equivalent (MRSE), corneal thickness, topographic pattern, and residual stromal bed thickness (RSB).
The risk factors in order of importance are preoperative topographic pattern, RSB (residual stromal bed), age, preoperative pachymetry, and myopia. Topographic pattern preoperatively is the most important factor. The other risk factors are asymmetric bow tie, abnormal and inferior steep, skewed axis, and severe asymmetry between eyes. This scoring system was based on Placido-based topography. [56]
Differentiating post-refractive surgery regression from ectasia: Several parameters, such as corneal thinning, increase in dioptric power of the cornea, change in refraction, and change in the best corrected visual acuity, are all important in distinguishing regression from ectasia. Corneal topography is an important part of this process.[56]
Terrien marginal degeneration: Usually, Terrien marginal degeneration starts in the superior cornea. There is peripheral thinning, vascularization, and lipid deposition. Recurrent episodes of inflammation may occur, and the thinning may lead to perforation. The topographic pattern is an inverted crab claw configuration.[60]
Pellucid marginal corneal degeneration (PMCD): It is a noninflammatory corneal ectatic disorder that presents later in life than keratoconus and progresses more slowly. "Butterfly pattern" or crab claw pattern in Placido-based topography may not be the main diagnostic feature. Schiempflug-based tomography gives more importance to the pachymetric map to distinguish PMCD from Keratoconus.[61]