Continuing Education Activity
This activity explores glass ionomer cement (GIC), a revolutionary self-adhesive restorative material in dentistry. Comprising fluoro-aluminosilicate glass powder and polyacrylic acid liquid, GIC has extensive applications in restorative adult and pediatric dentistry. The session covers the comprehensive aspects of GIC, including its composition, manipulation techniques, setting reactions, mechanical and biological properties, indications, and classification. Through this activity, participants will thoroughly understand GIC's clinical utility, positioning them at the forefront of utilizing this innovative material in diverse dental applications.
From its initial introduction, glass ionomer cement has undergone continual refinement, improving its properties and expanding its applications. This activity underscores the pivotal role of GIC in various dental procedures, such as cementing fixed dental prostheses, orthodontic bands, and brackets. Furthermore, it discusses GIC's versatility as liners, core build-up material, pit and fissure sealant, and its application in the atraumatic restorative technique (ART). Participants will emerge with valuable insights into the potent anti-cariogenic action of GIC, enhancing their comprehension of its clinical benefits and reinforcing its significance in contemporary dental practice.
Objectives:
Determine the correct GIC application technique to attain the best properties of the material.
Identify the setting reaction and the factors affecting the setting of GIC for predictable clinical outcomes.
Assess the physical, mechanical, and biological properties of GICs.
Identify the uses and classification of GICs for appropriate clinical decision-making.
Introduction
Glass ionomer cement (GIC) is a self-adhesive restorative material.[1] Chemically, it combines fluoro-aluminosilicate glass powder and polyacrylic acid liquid. GIC has a broad spectrum of restorative adult and pediatric dentistry uses and exhibits potent anti-cariogenic action.
GIC was first described by Wilson and Kent in 1972 and has evolved gradually to improve its properties and broaden its uses. GIC is used for the cementation of fixed dental prosthesis (FDPs), orthodontic bands, and brackets, to restore carious and noncarious lesions, and as liners or bases, core build-up material, pit and fissure sealant, and for atraumatic restorative techniques (ART).[2]
Function
Composition
Glass ionomer cement is generally supplied as a powder-liquid system that is mixed manually. The powder is fluoro-aluminosilicate glass, and the liquid is an aqueous solution of polyacrylic acid. Polyacrylic acid is copolymerized with carboxylic acid, maleic, tartaric, and itaconic acid to regulate the viscosity and stabilize the liquid. The liquid exhibits a thixotropic behavior: its thickness can be reversed by shaking or warming the bottle. Other supply options include capsules, twin syringes, and single-bottle water-settable form (freeze-dried polyacrylic acid added to GIC powder).[3][4]
Manipulation
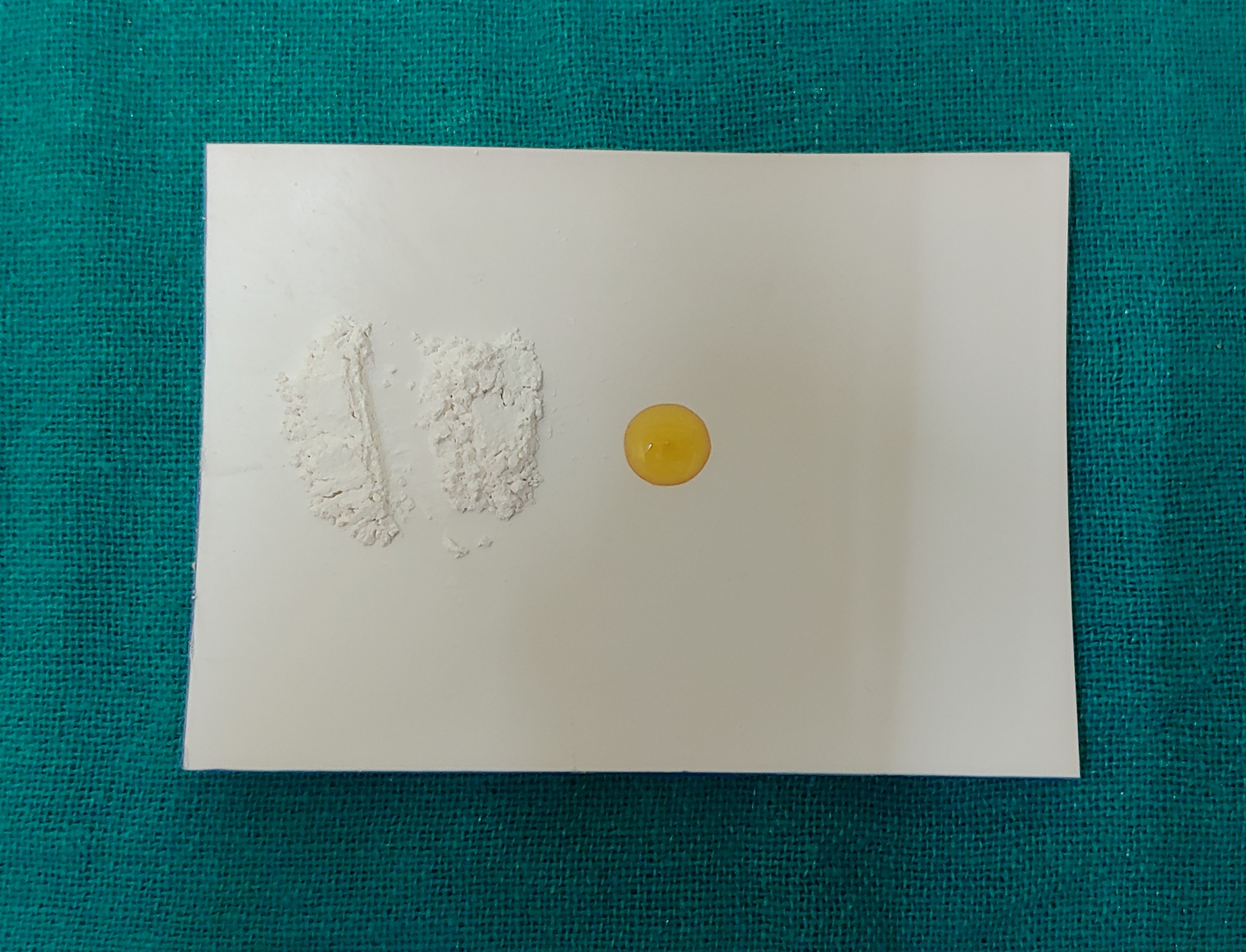
Mixing is performed with an agate spatula. A stainless steel spatula is not used because its surface gets abraded by glass particles, contaminating the mixture. The powder and liquid are used in the proportions recommended by the manufacturer (see Image. Mixing Glass Ionomer Cement). The powder is divided into 2 equal increments. The liquid is dispensed later to prevent increased viscosity by water loss on environmental exposure.
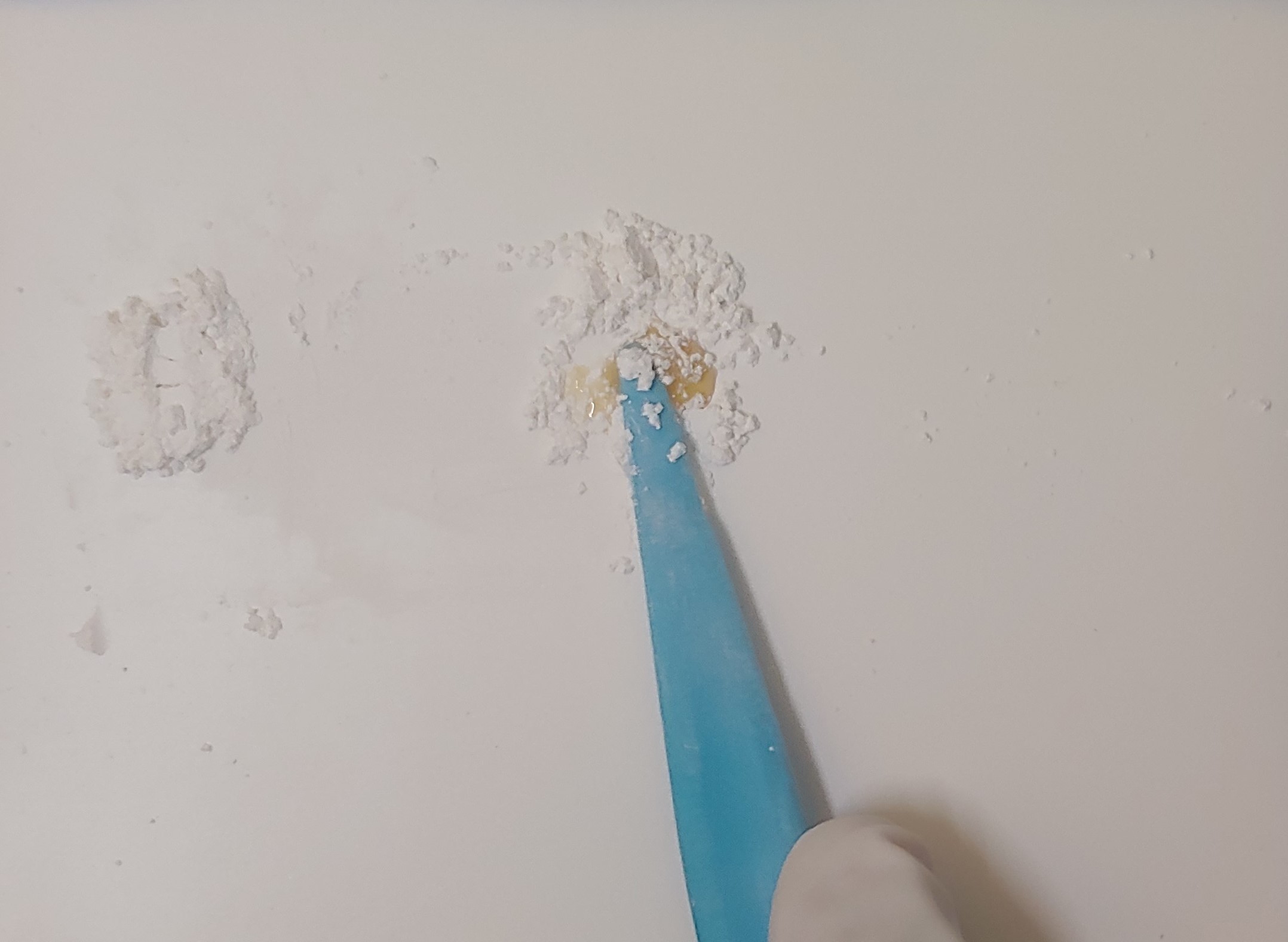
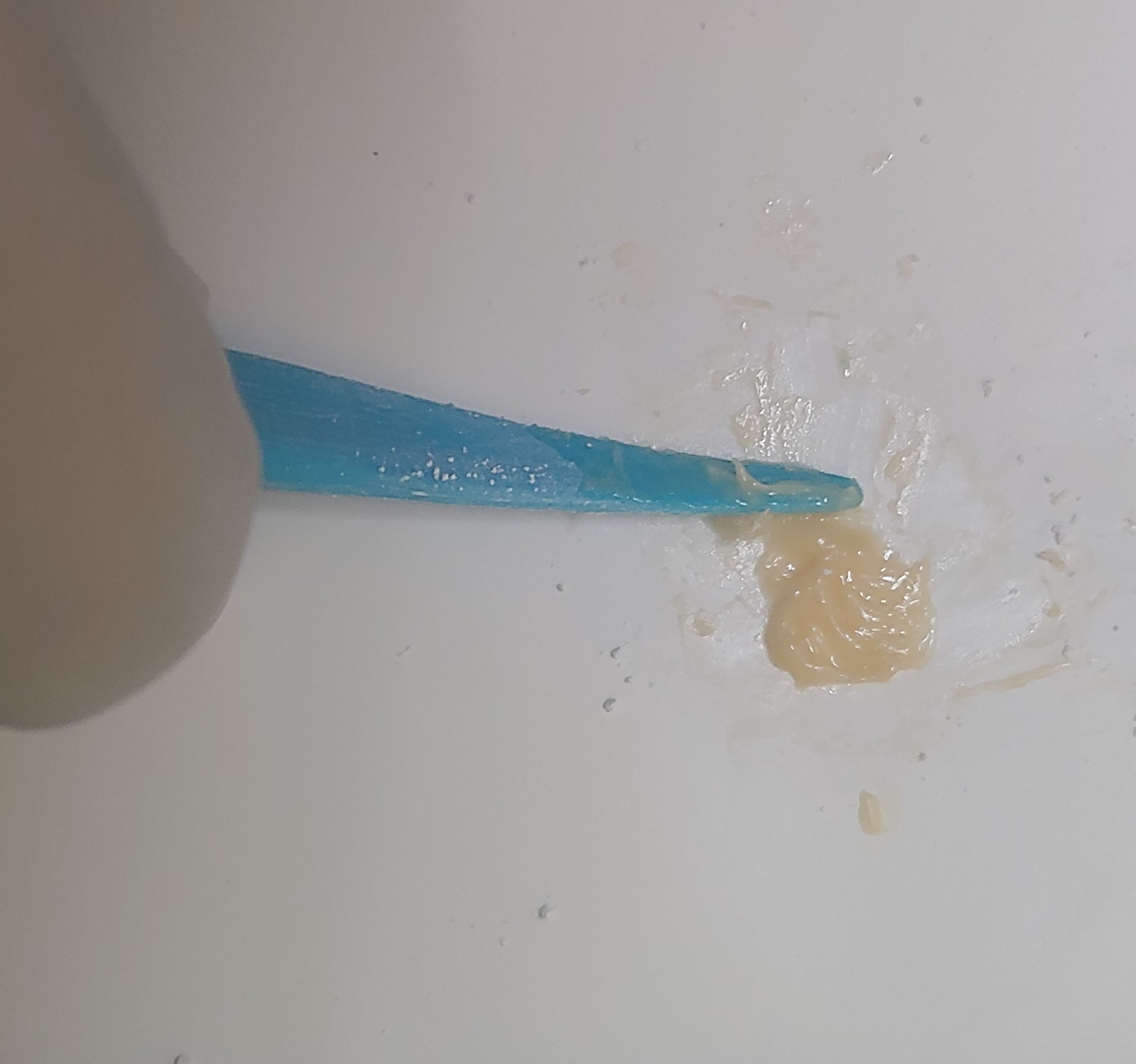
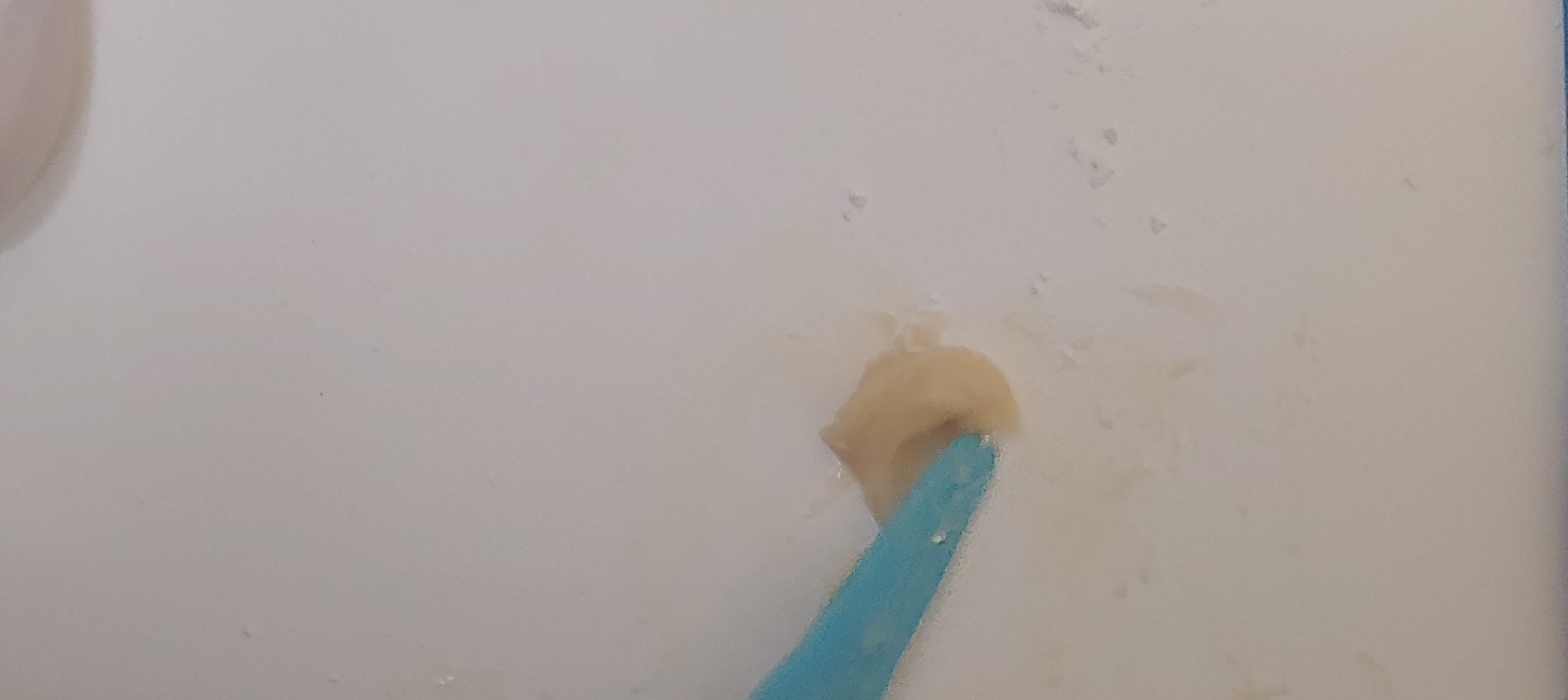
The first increment is added to the liquid and mixed using a folding motion for 15 seconds within a limited area on the mixing pad (see Image. Folding Glass Ionomer Cement). The second increment is added to adjust the consistency. The resultant mixture should have a glossy surface (see Image. Freshly Mixed Glass Ionomer Cement). Such a surface indicates that an adequate number of carboxylic ions are available, crucial for forming chemical bonds with the tooth surface. Mixtures with an opaque surface should be discarded (see Image. Poor Mix Adhesion).
Glass ionomer cement can also present as a capsule activated by vibrating it in an auto-mixer. The vibration mixes the cement, and the already mixed GIC paste can be used for the chosen clinical indication.
Preparation and Restoration of the Tooth
- Cleaning: A pumice slurry should be applied to the tooth surface using a prophy cup.
- Conditioning of tooth: after rinsing and drying the tooth, 10% polyacrylic acid is applied for 10 seconds to increase the surface energy and wettability of the tooth, which improves chemical bonding.[4]
- Placement of restoration: the mixed GIC is carried to the cavity with the help of a cement carrier and adapted using a condenser. Cement sticking to the spatula should be avoided as it is difficult to remove.
- Protection of the cement: the setting cement should be covered by a matrix band during the initial setting and by varnish, cocoa butter, or vaseline after the initial set because GIC is moisture sensitive during the first 24 hours of setting.
- Finishing and polishing: initial finishing includes the removal of gross excess with a sharp hand instrument. Final finishing is done after 24 hours.
Mechanism of Setting
The setting of GIC is through an acid-base reaction involving the following stages:
- Dissolution and decomposition: after mixing the powder and liquid, the acid dissolves the surface of the glass particles to release SiO44-, Ca2+, Na+, and F- ions.
- Initial setting: the Ca2+ released in the aqueous medium reacts with polyacrylic acid to form a 3-dimensional cross-linked structure. At this time, the material has low strength, and it can be carved using sharp instruments.
- Final setting: the setting reaction continues during the next 24 hours. During this time, SiO44- forms the silica gel. The slow-moving Al3+ ions enter the aqueous medium and cross-link the polyacrylic acid chains, displacing the Ca2+ ions. This increases the final strength of the set cement.
- Maturation: the aluminum and calcium cross-linked polyacrylate chains get hydrated over time by absorbing water from the aqueous medium. This process is known as maturation.[5][6]
The Role of Water in the Setting of GIC
GIC is water-based cement because water constitutes 11% to 24% of the set cement. Water plays a crucial role in the GIC setting. In the initial phases, it acts as a reaction medium. In later stages, it mediates the slow hydration of the cross-linked chains.
The water can evaporate quickly during the initial phases due to exposure to ambient air. On the other hand, water contamination during this stage can cause the matrix's dissolution and calcium ions' leakage.[7] Thus, uptake or loss of water results in a weak, opaque, and more soluble cement. The cement's uptake or loss of free water can be prevented by coating the surface of the restoration with varnish, cocoa butter, or petroleum jelly immediately after placing the restoration.
Indications
Restorative material: Thanks to its easy placement and better marginal adaptation, glass ionomer cement is popularly used in pediatric restorations. GIC is also indicated for restoring permanent teeth in low stress-bearing areas like class III and V lesions and is the material of choice in patients with a high risk of caries due to the release of fluoride.
Luting agent: GIC can lute indirect restorations (metal and metal-ceramic), post, core, and orthodontic bands, and brackets.[4][8]
Pulp protection: GIC is used as a liner or base beneath metallic and composite restorations (sandwich technique).[9]
Pit and fissure sealant: GIC-based fissure sealants offer less retention than resin-based ones, only indicated as temporary sealants in newly erupted permanent teeth. The caries preventive action of GIC-based pit and fissure sealants is comparable to resin-based pit and fissure sealants.[10]
Atraumatic restorative technique: Atraumatic restorative technique (ART) is a minimally invasive procedure that involves removing carious tissue with hand instruments without anesthesia. Restoration of the cavity requires an adhesive material like glass ionomer cement (GIC). ART is performed in those cases where routine dental treatment cannot be done because of a lack of facilities or accessibility to the dental clinic.[11]
Issues of Concern
Mechanism of Bonding
GIC chemically (ionic) bonds to the tooth structure (enamel and dentin). GIC bonds better to enamel than dentin because of the higher inorganic content in enamel. The mechanism of GIC adhesion to the tooth's inorganic structure involves a chelation reaction between the carboxyl groups of the polyacrylic acid and the calcium in the hydroxyapatite crystals of the tooth.
Fluoride Release
Various forms of fluorides (CaF2, SrF2, LaF2, Na3AlF6, AlF3) were added to the powder of GIC during manufacture as a flux, and their antibacterial properties were observed later. In completely set cement, fluoride ions are not an essential part of the matrix and are in an unbound form. These ions are released into the saliva by diffusion.
Two mechanisms have been proposed to explain the fluoride release from GIC into an aqueous solution.[12] The first mechanism is a short-term process involving rapidly dissolving fluorides from the outer surface into the solution.[12] The second mechanism is a continuous and gradual diffusion of fluoride through the cement.
The bulk of the GIC matrix plays a vital role in the fluoride release capacity. The fluoride release is influenced by intrinsic factors such as the composition of the matrix, setting mechanism, and fluoride content, and extrinsic factors like the pH of saliva, plaque, pellicle formation, liquid-to-powder ratio, mixing, setting and curing time, and the amount of exposed surface. Bleaching and tooth brushing do not significantly affect fluoride release.[13] The coverage of the surface of GIC with an adhesive or surface protective agent results in a 1.4 to 4-fold decrease in fluoride release.
Anticariogenic Action
Various mechanisms can explain the anticariogenic action of fluoride, including decreased demineralization, increased remineralization, enhancing the resistance of enamel to acid attack by conversion of hydroxyapatite to fluorapatite, and the inhibition of enolase enzyme, thus interrupting microbial replication and metabolism. A sustained fluoride release from the restoration in the marginal gaps (between restoration and tooth) helps prevent secondary caries. This property of GIC makes it the material of choice for restorations in patients with high caries activity.
Biological Activity
GIC is both biocompatible and bioactive. Although the pH of freshly mixed GIC ranges between 0.9 and 1.6, the pulp response to GIC is mild.[5] The excellent tolerance of GIC by the pulp is attributed to 2 factors. First, the pH rises significantly in the first 20 minutes. Secondly, the high molecular weight and the large molecules of polyacrylic acid prevent the penetration of the acid molecules in the dentinal tubules to a considerable depth. There is no requirement for pulpal protection while restoring with GIC when the remaining dentinal thickness (RDT) is more than 1 mm.
Mechanical Properties
Glass ionomer cement has compressive strength equivalent to zinc phosphate cement, whereas its tensile strength is slightly higher than zinc phosphate cement. Type I GIC has lower compressive strength than Type II GIC. GIC is less stiff and has a lower modulus of elasticity comparable to dentin but lesser than zinc phosphate cement.[8] The resilience of GIC is similar to dentin, which is why it is known as man-made dentin.
The powder-to-liquid ratio determines the mechanical properties of the set cement. More powder increases the consistency of the cement, strength, and speed of the setting reaction. However, the powder-to-liquid ratio can be increased until a critical point. The volume of the physical matrix will be deficient in binding and holding the cement ingredients together; the mechanical properties will be compromised significantly. Thus, the powder-to-liquid ratio should strictly comply with the manufacturer's instructions. Using pre-graduated self-contained mixing capsules solves this problem.[14]
Physical Properties
The thermal expansion coefficient of GIC is similar to enamel and dentin. The thermal diffusivity of GIC is similar to dentin, providing thermal insulation to the pulp. The solubility of GIC in water is higher than zinc phosphate and zinc polycarboxylate.[14] GICs are tooth-colored restorative materials but are not recommended to restore anterior teeth because of their opacity and lack of translucency.
Advantages
- Chemical bonding to the tooth structure [5]
- Caries preventive action [8]
- Thermal compatibility with tooth structure
- Mild pulp response [5]
- Tooth-colored restorative material [14]
Disadvantages
- Poor mechanical properties, eg, low compressive strength, low abrasion resistance, and fracture resistance, make its use restricted to low stress-bearing areas [5][7]
- Poor esthetics due to lack of translucency
- Moisture sensitive while setting [7]
The longevity of glass ionomer cement restorations is affected by occlusal forces, porosities in set cement, desiccation or water absorption during initial setting, and use of the mixed cement after the loss of gloss. Furthermore, larger GIC particles decrease the wear rate; the cement's solubility depends on the amount of cement at the margins.
Classification of GIC
GIC may be classified based on application as follows:
- Type I - Luting cement used for cementation of crowns and bridges
- Type II - Restorative cement used for aesthetic fillings
- Type III – GIC used as liners and bases
- Type IV – GIC used as pit and fissure sealants
- Type V – GIC used for orthodontic cementation
- Type VI – GIC is used for core build-up in highly mutilated teeth
- Type VII – Fluoride releasing light-cured GIC
- Type VIII – GIC for atraumatic restorative treatment (ART)
- Type IX – GIC used for pediatric and older adult restorations
GIC may also be classified as follows:
First Generation
This material was developed because silicate cement was showing poor clinical performance. To overcome this problem, the alumina-to-silica ratio was increased. The first glass ionomer developed was ASPA I (aluminosilicate polyacrylic acid), which had a sluggish setting, was sensitive to moisture while sitting, and had poor esthetics, resulting in limited clinical utility. Wilson and Crisp added d-tartaric acid to the liquid, allowing the use of glasses containing lesser fluoride, which is more translucent. ASPA I was then named ASPA II and accounted for the first glass ionomer cement used for clinical applications.[15]
Second Generation
In this type of cement, the polyacid was already added to the powder, and the setting was achieved by mixing the powder with water or a tartaric acid solution. This GIC is known as water-hardening cement. The main advantages of the second-generation system are enhanced shelf life, decreased initial viscosity, and improved strength.
Reinforced Cement
The conventional GICs are suitable for restoring low stress-bearing areas like Class V and Class III cavities and sealing pits and fissures. However, they are not indicated in high-stress-bearing situations such as Class II cavities because of their low tensile strength (7 to 12 MPa). To widen its range of applications, attempts were made to improve the strength of GIC by the following methods:[5]
- Dispersed phase glasses: using dispersed phases of strengthening crystallites like aluminum oxide, titanium oxide, and zirconium oxide improved the strength.[16]
- Fiber-reinforced glasses: adding alumina fibers, glass fiber, silica fiber, and carbon fiber to the glass ionomer powder increased flexural strength.[17][18]
- Metal reinforced GIC: the mixture of amalgam powder and GIC, commonly known as 'miracle mix.'[19]
- Cermet ionomer cement: manufactured by sintering the metal and glass powders together, which helps achieve a strong metal bond to the glass.[20]
- Highly viscous conventional glass ionomer cement: mainly useful for ART. The highly viscous GIC can be inserted in the cavity, similar to dental amalgam.[21]
- Resin-modified glass ionomer cement: resin-modified glass ionomer cement was developed by adding resins and photoinitiators to the conventional glass ionomer.[22]
- Amino acid modified glass ionomer cement: substituting copolymers of unsaturated carboxylic acids with acrylic acid copolymers such as N–methacryloyl–glutamic acid improved the fracture toughness of GIC.[23][24]
Metal Modified GIC
Metal particles in the silver alloy are added to the conventional GIC powder to improve the mechanical properties of GIC and permeate its use in Class I cavities in molar teeth. The GIC can be reinforced with metal in a silver admixture or cermet mixture.
Silver Alloy Admixed GIC
The powder of this modification of GIC is obtained by adding 1 part of spherical silver alloy particles to 8 parts of conventional GIC powder. The liquid consists of polyacrylic acid. The powder and liquid are mixed at a ratio of 3:2 by weight.[18]
Cermet Mixture
McLean and Gasser introduced cermet in 1985. Cermet is obtained by sintering the microfine silver alloy with glass particles at high temperatures and pressure. The pellet thus formed is ground to form finer powder particles.[18]
Properties of Metal Modified GIC
The wear resistance is substantially improved in metal-modified GIC compared to conventional GIC. The wear resistance of cermet is greater than that of silver alloy admixed GIC. The compressive strength and fracture resistance are mildly improved. The use of metal-modified GIC in high-stress-bearing areas is restricted to primary dentition only.
Chemical bonding to the tooth structure is slightly lessened due to the silver present in the composition. Both silver alloys admixed GIC and cermet release fluoride in significant quantities. However, the fluoride release is comparatively less in cermet than in silver alloy admixed GIC. Metal-modified GICs have improved handling properties and exhibit fewer porosities in set cement.
Indications
- Core build-up
- Class I cavities in primary dentition
Resin-modified Glass Ionomer Cement
Hybrid ionomer or resin-modified glass ionomer cement was developed by the addition of resins (bisphenol A-glycidyl dimethacrylate or urethane dimethacrylate) and photoinitiators to the conventional glass ionomer.
Composition of Resin-modified Glass Ionomer Cement
- Powder: fluoroaluminosilicate glass, light, and chemical initiators
- Liquid: aqueous solution of polyacrylic acid and 10% 2-HEMA
Setting Reaction
Hybrid ionomers are set by a dual-reaction curing mechanism involving acid-base and polymerization reactions. When the liquid and powder are mixed, the polymerization reaction starts with chemical or light-mediated initiation. This set resin protects the ongoing acid-base setting reaction in the cement matrix from moisture contamination. This phenomenon is known as the "umbrella effect," reducing the early moisture sensitivity of GIC and providing greater initial strength.[25] The slowly proceeding acid-base reaction determines the final strength.
Structure of Set Cement
The cement consists of a core and matrix. The core constitutes unmixed powder particles, whereas the matrix comprises polyacid and HEMA polymer linked with hydrogen bonding.
Properties
The hybrid ionomer bonds chemically to the tooth structure. However, the ionic activity is reduced due to the presence of resin. This results in a lesser bonding tendency.
The fluoride release is slightly lesser than conventional GIC.[13] The formation of complex fluoride derivatives in a reaction with polyacrylic acid influences the release of fluoride. This hybrid may also be affected by the type and amount of the resin used. The initial pH of the hybrid ionomer (pH=3.5) is higher than conventional GIC (pH=2), which reduces pulp irritation.
Wear resistance, fracture toughness, flexural, and diametral tensile strength of hybrid ionomer are superior to conventional GIC, whereas compressive strength is inferior.[2][3] The translucency of the hybrid ionomer is superior to conventional GIC. Hybrid ionomer exhibits a slight tendency for shrinkage due to the polymerization of the resin component.
Indications
- Class V restorations due to reduced moisture sensitivity
- Restoration of non-carious cervical lesions [7]
- Class I and II restorations in primary teeth [26]
- A liner or base under composite restorations (sandwich technique)
Polyacid Modified Glass Ionomer/Compomer
Compomer is formed by combining composite resin with glass ionomer. In this material, ion-leachable glass particles of GIC are added as fillers in the composite matrix. This combination integrates some of the composite resins and glass ionomer cement properties. Compomer is supplied as a single-component material.[27]
Mechanism of Setting
Setting occurs by light-induced polymerization. The acid-base setting mechanism does not exist due to the absence of polyacids from the composition.
Properties
Mechanical properties such as wear resistance, strength, and fracture toughness are superior to conventional GIC but inferior to composite resins. Compomer bonds micro-mechanically with tooth structure but has no chemical bonding ability. Fluoride release is reduced compared to conventional GIC, but esthetics are superior.
Indications
- Pit and fissure sealant
- Cementation of post and core
- Restoration of deciduous teeth
- Class III and V lesions
Clinical Significance
Glass ionomer cement (GIC) is also known as man-made dentin because it simulates dentin in terms of modulus of elasticity, resilience, coefficient of thermal expansion, and thermal conductivity. GIC chemically adheres to the tooth structure, is biologically compatible, and has fluoride-releasing properties.[4][5] These features proclaim GIC an excellent substitute for dentin.[7] However, reduced strength, abrasion resistance, and esthetics contribute to its decreased usage in various clinical scenarios.[4][5] The material selection for a clinical condition should be made after weighing the merits and demerits of the available materials.
GIC and its modifications have a wide array of uses. Owing to resiliency, very low shrinkage, and thermal compatibility with tooth structure, these materials have proven to be liners underneath restorative materials like dental composites (sandwich technique).[28] Attributing to the property of bonding to dentin surfaces without removing the smear layer, their biological compatibility, and fluoride release, GICs and modified GICs are the materials of choice in restoring carious teeth in high-risk patients.[29] Because of the ease of placement and snap set property, light-cured GICs are the material of choice for restoration in children.[7]
GICs are highly successful as luting agents for cementation of stainless steel crowns for deciduous teeth, cast metal crowns, fixed dental prostheses for permanent teeth, space maintainers, orthodontic bands, and brackets. Resin-modified GIC is used for luting zirconia and alumina-based crowns.
GICs can repair defects in tooth structure before crown preparation to stabilize the weakened portions of the tooth.
Along with amalgams and composites, GICs are used as core build-up materials. GICs are preferred as core build-up materials because of their property of chemical adhesion to the tooth structure. When used as fissure sealants and cervical restorations, GIC demonstrates good performance.[4][5][7]
Nursing, Allied Health, and Interprofessional Team Monitoring
Nurses play a crucial role in assessing patients before and after GIC procedures. They must monitor for any allergic reactions, discomfort, or adverse events related to using GIC. Nurses should maintain detailed and accurate documentation of GIC procedures, including the type of GIC used, dosage, patient response, and complications. This information is essential for patient care continuity and communication with other healthcare providers. Interprofessional teams, which may include dentists, physicians, nurses, pharmacists, and other healthcare professionals, should collaboratively decide on using GIC based on the patient's overall health, treatment goals, and available alternatives. Interprofessional communication is crucial for reporting and addressing any adverse events associated with GIC. This allows for prompt intervention, shared learning, and adjustments to clinical practices if necessary. All team members, including nurses and allied health professionals, should participate in ongoing training and workshops to stay updated on the latest advancements, techniques, and safety considerations related to GIC.