Continuing Education Activity
Microphthalmia with a cyst is a congenital ocular anomaly characterized by an abnormally small eye associated with a cyst in the orbit. The pathology of this condition generally results from the defective closure of the embryonic fissure during early gestation, consequent to which the ocular structures become underdeveloped and an orbital cyst aberrantly forms. A diagnosis is made after clinical evaluation with imaging modalities, intraocular anatomy assessment, and evaluation of the extent of the cyst. The condition necessitates management strategies adopted by a multidisciplinary team consisting of ophthalmologists, pediatricians, and geneticists to effectively manage the ocular manifestations of the disease and associated systemic manifestations. Treatments may include surgical management for complications and optimization of visual function, supplemented by visual aids and rehabilitation strategies to improve quality of life and visual outcomes in those affected. However, due to the congenital anomaly, many patients have moderate to severe blindness in the affected eye. Prevention of contracted sockets with optimal cosmesis is another aspect of the management.
Participants in the course learn about the genetic underpinnings, clinical presentations, and potential complications of microphthalmia with a cyst. The course emphasizes the importance of interprofessional collaboration in managing this complex condition, illustrating how coordinated care among ophthalmologists, pediatricians, and geneticists can significantly enhance patient outcomes. By working together, healthcare professionals can effectively address the ocular and systemic manifestations, optimize visual function, and improve the overall quality of life for affected individuals.
Objectives:
Identify the genetic and embryological factors contributing to the development of microphthalmia with a cyst.
Screen for potential systemic associations and complications that may accompany microphthalmia with a cyst.
Implement evidence-based protocols for early diagnosis and treatment of patients with microphthalmia with a cyst.
Collaborate with an interprofessional team to provide a comprehensive care plan for patients with microphthalmia with a cyst for improved clinical outcomes.
Introduction
Microphthalmia or microphthalmos is one of the most common congenital ocular malformations, characterized by a small yet identifiable eye with anatomical abnormalities.[1] This contrasts with anophthalmia or anophthalmos, defined as the complete absence of the eye due to deficient development or arrest of differentiation during earlier stages of development.[2] Congenital microphthalmia with an orbital cyst (or microphthalmia with a cyst) is a rare developmental subtype of microphthalmia characterized by microphthalmia associated with an inferior orbital cyst.[3] This must be differentiated from a congenital cystic eye, also known as anophthalmia with a cyst, which is usually present in the superior orbit and the eye is absent.[4]
Microphthalmos and anophthalmos occur due to abnormality during the early phases of embryonic development.[5][6] Microphthalmos, anophthalmos, and coloboma (MAC) are a spectrum of congenital developmental anomalies. Visual acuity is often very poor in such cases. Interprofessional collaboration is needed for early detection and prompt management to ensure proper visual outcome, cosmesis, and orbital development. Microphthalmia with an orbital cyst is a debilitating congenital anomaly whose management must be initiated immediately for satisfactory outcomes.[3]
Etiology
The influence of gestational insult on developing microphthalmia with a cyst is controversial. Possible risk factors for MAC include infection during the first trimester (including rubella), vitamin A deficiency during pregnancy, alcohol use, or use of various drugs during pregnancy, including thalidomide, isotretinoin, and warfarin.[7] Other risk factors for MAC include prematurity, low birth weight, advanced maternal age (older than 40), and multiple births.[8] Other congenital anomalies may coexist with MAC.
The association may be syndromic or nonsyndromic.[9] Syndromic associations of MAC include CHARGE syndrome (coloboma, heart disease, atresia of the choanae, retarded growth and mental development, genital anomalies, ear malformations, and deafness), Aicardi syndrome, Hallermann-Streiff syndrome, Warburg syndrome, cat-eye syndrome, and Lenz microphthalmia syndrome.[10] Recognition of the related genetic syndromes with appropriate genetic counseling is essential. Although most cases present in isolation, familial occurrence in monozygous twins and siblings has been documented.[11]
Epidemiology
Although the prevalence of microphthalmia varies between 1.4 and 3.5 per 10,000 births, there is a paucity of literature regarding the demographic profile of microphthalmia with a cyst.[11] Several study results have shown a prevalence of 0.3 to 0.6 per 10,000 births.[2][11] Microphthalmia with a cyst is usually a nonhereditary (sporadic) disorder without gender predilection; this generally appears within the first few months after birth and may be detected as early as the neonatal period. Although most cases are unilateral, microphthalmia with a cyst can manifest bilaterally.[1]
A genetic cause may be identified in up to 80% of cases with bilateral severe microphthalmos or anophthalmos.[12] Most commonly, mutations in SOX2 (15% to 40% of MAC cases) or OTX2 (2% to 5% of MAC cases) genes are noted in such cases.[12][13] Molecular diagnosis can be established in up to 10% of unilateral microphthalmia or anophthalmia cases.[9][14][15] CHARGE syndrome occurs due to a mutation in the CHD7 gene.[10]
Commonly involved genes in MAC include the following:
- Autosomal dominant: SOX2, OTX2, PAX6, BMP4, TFAP2A, and CHD7
- Autosomal recessive: RAX, FOXE3, STRA6, and SMOC1
- X-lined recessive: BCOR and PQBP1.[9][16]
Pathophysiology
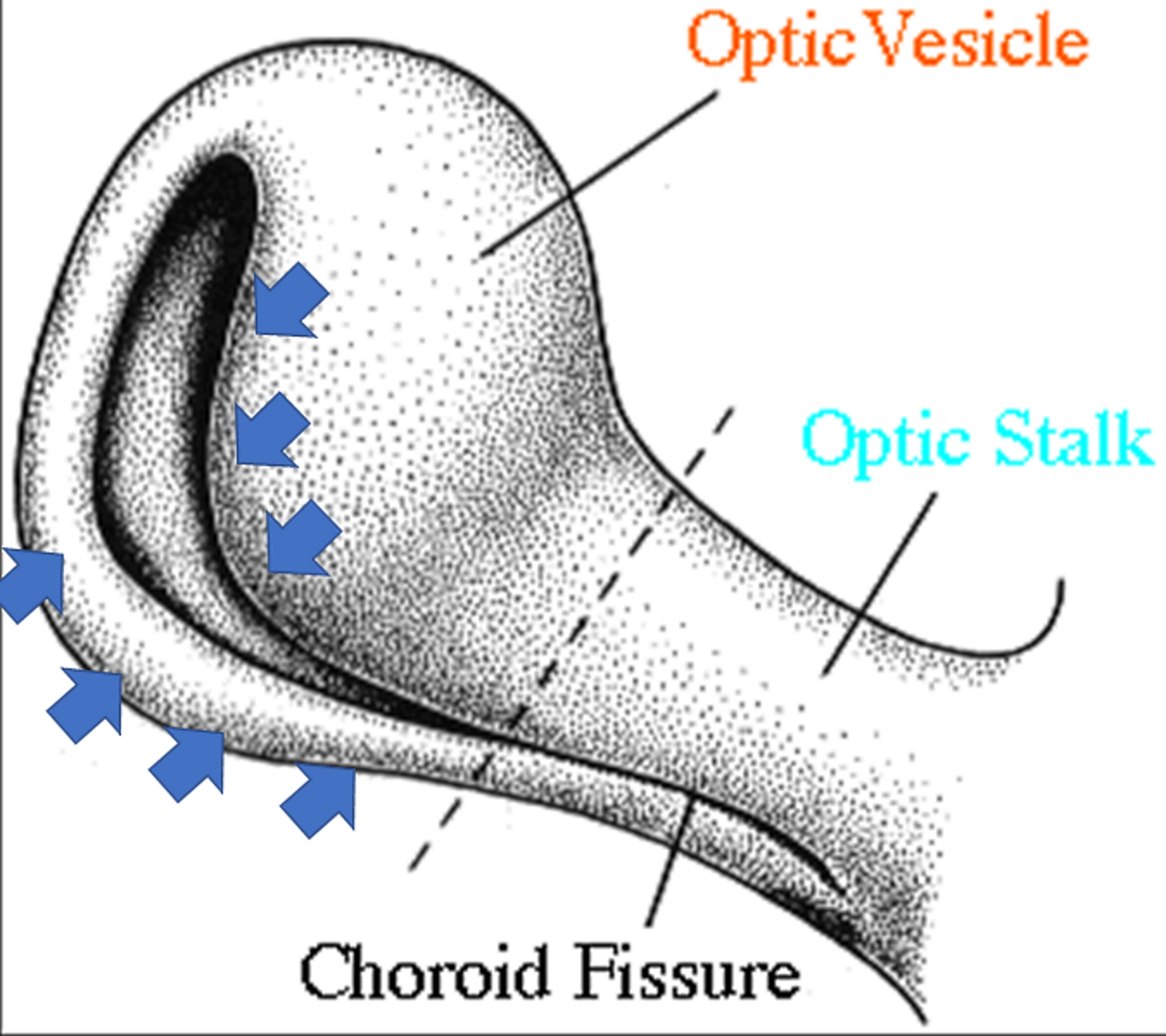
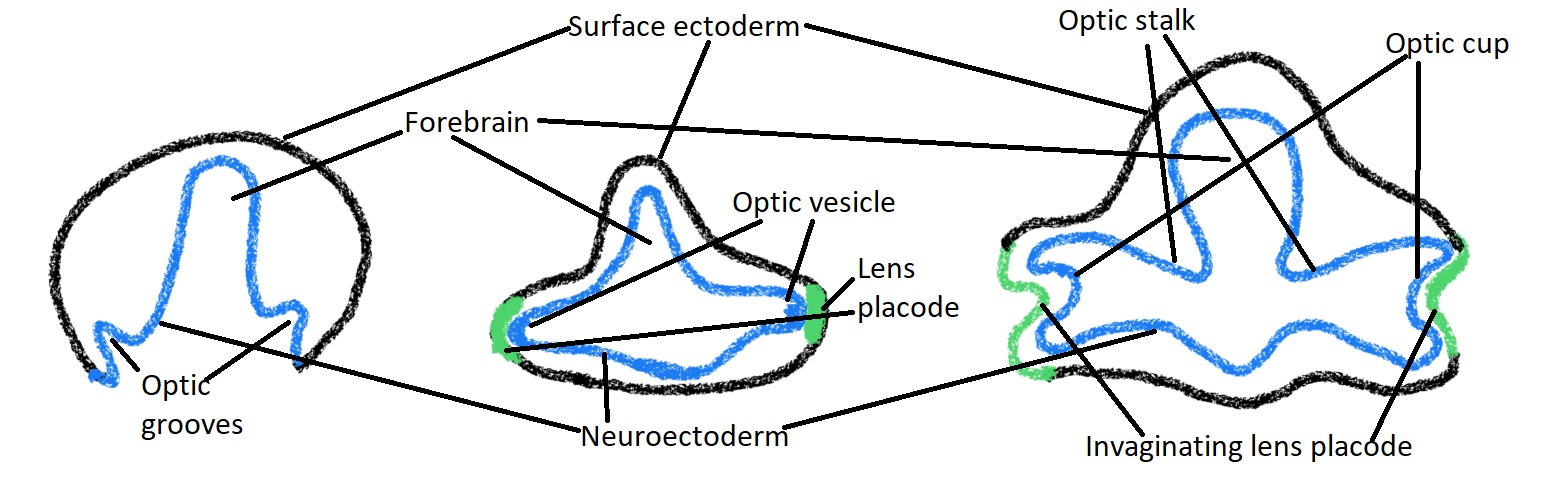
The basis of the development of microphthalmia with a cyst is embryological. The eye's development starts at the embryonic age of 21 to 22 days with the development of the optic pit (optic groove or optic sulci).[17] These grooves gradually become out-pockets of the forebrain, which approach the surface ectoderm and are known as optic vesicles (see Image. Embryological Development of Optic Vesicle).[17] The stalk connecting the optic vesicle to the forebrain is called the optic stalk. The optic vesicle, which is a part of the diencephalon of the forebrain, is fully formed by around the embryonic age of 25 days.[18][19] By 27 days, a part of the optic vesicle nearly reaches the surface ectoderm, which gets thickened and forms the lens placode. The lens placode of the surface ectoderm and the optic vesicle near the placode then invaginates.
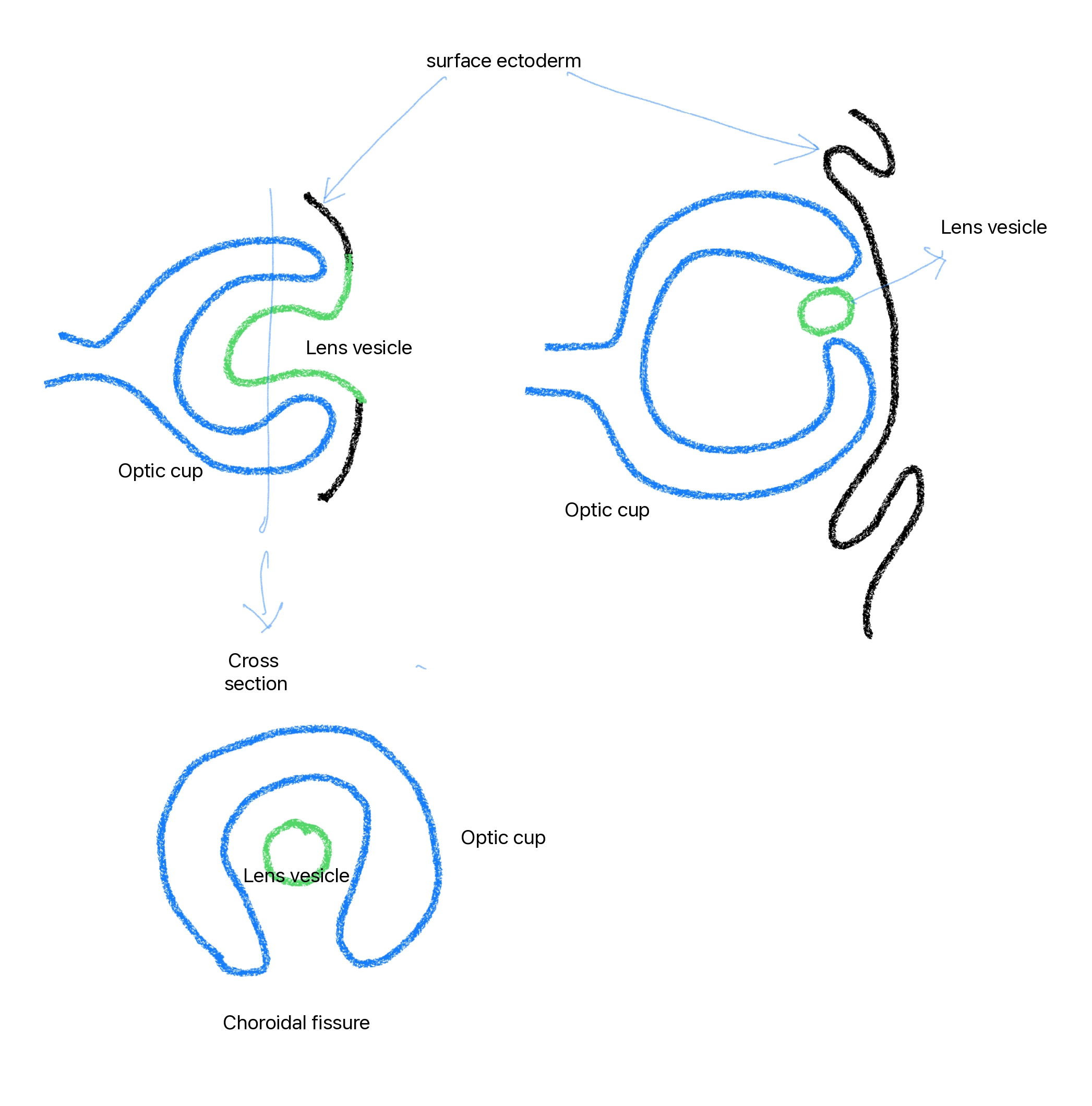
The invagination of the optic vesicle results in the optic cup, which has 2 layers (inner and outer). The lens placode invaginates to form a lens vesicle that ultimately separates from the surface ectoderm at 33 days. At 5 weeks of gestation, the margins of the optic cup grow over the lens vesicle and envelop it except on the caudal side of the lens vesicle and the caudal (or inferior) side of the optic stalk (see Image. Invagination Process of the Optic Stalk and the Optic Vesicle). This gap or fissure in the inferior side of the optic cup is called the embryonic fissure, fetal fissure, or choroidal fissure (see Image. Choroidal Fissure and Lens Vesicle), through which the hyaloid vessels pass.[19] The choroidal fissure closes by 6 to 7 weeks of embryonic age.[19]
Normally, the embryonic fissure's closure begins at the 11 mm stage and completes by the 18 mm embryonal stage. The invagination of the optic vesicle begins before the sixth to seventh embryological week. Following this, differential growth of the inner layer of the optic cup occurs (where the inner layer develops faster than the outer layer), resulting in everted margins of the fissure. The complete formation of the retina at these margins may prevent the closure of the optic cup. In the case where the closure fails, a typical coloboma is formed. When no closure occurs, these retinal layers are further distended, followed by an accumulation of fluid between the layers—forming a cyst.[20] The gradual accumulation of fluid in the cystic cavity may be attributed to the presence of microvilli in the inner layer of the cyst comprising the glial tissue.
Another postulated theory is the presence of communication between subarachnoid space and the cyst, which may result in the enlargement of the cyst. The glial tissue's extensive, non-neoplastic, reactive proliferation may further lead to cavity expansion.[21][22] The timing of the developmental arrest plays a key role in understanding this entity's etiology. Microphthalmia with a cyst results when the embryological disturbances occur later at the 7 to 14 mm stage during 6 to 7 weeks of gestation, when ocular structures are already present. On the contrary, when the arrest occurs during the 2 to 7 mm stage, causing failure of invagination of the primary optic vesicle, anophthalmos with cyst results.[23]
Histopathology
Histopathology with immunohistochemistry (IHC) remains the gold standard investigation for confirming the diagnosis of microphthalmia with a cyst (see Image. Immunohistochemistry for Glial Fibrillary Acid Protein). The outer wall of the cyst is composed of dense fibrous connective tissue; the inner layer, derived from the neuroectoderm, comprises thick neuroglial tissue with variably differentiated immature retinal elements. A varying amount of calcification and pigmentation may be found in the cystic cavity. Surrounding rudimentary ocular structures may be seen in connection with the cyst.[20]
The cyst is usually found attached to the inferior portion of the globe in microphthalmos, unlike anophthalmia, where the cyst is usually centrally or superiorly located with the absence of ocular structures. IHC may reveal glial positivity using glial fibrillary acid protein staining, owing to the expression of astrocytes. Optic nerve elements are identified using the neurofilament protein, and the surrounding meningeal tissue may demonstrate epithelial membrane antigen positivity. Disorganized retinal tissue may stain positive for S-100, vimentin, and neuron-specific enolase.[4] Recent advances in IHC, scanning, and transmission microscopy have aided in gaining further insights into these complex malformations.
History and Physical
Most of the patients encountered in the ophthalmic setting present with visual impairment at birth, bulging of the lower eyelid (this condition may rarely involve the upper lid), firm bluish swelling (sometimes seen through the conjunctiva) with positive transillumination, an orbital mass, forward protrusion of the globe, or an inability to open the eye (since birth).[24] See Image. Patient ith Bilateral Microphthalmia With Cyst. Irido-fundal coloboma, optic disc coloboma, cloudy cornea, microcornea, shallow anterior chamber, angle-closure glaucoma, or pupillary membrane are the reported associations of the microphthalmic globe.[25] Evaluating the status of the contralateral eye in unilateral cases to exclude an underlying pathological condition is essential.[26] Looking for other systemic abnormalities such as microcephalus, cardiac conduction defects, basal encephalocele, cleft lip, corpus callosal agenesis, saddle nose, pulmonary hypoplasia, renal agenesis, and midbrain deformities in a case of microphthalmia with a cyst is important—especially if the condition is bilateral.[23]
Evaluation
Clinically, microphthalmia with a cyst is classified into 3 types (Duke-Elder classification):
- Type 1: Relatively normal eye with a clinically inapparent cyst
- Type 2: Grossly deformed eye with an obvious cyst
- Type 3: Large cyst pushing the globe backward, rendering it clinically invisible [11]
Although the diagnosis of microphthalmia with a cyst is mainly derived clinically, the role of orbital imaging can not be overemphasized. Standardized ultrasonography (USG A + B-scan) is the preferred initial investigation modality as it is rapid, noninvasive, easily accessible, and helps determine the eye's status (whether anophthalmic or microphthalmic). Magnetic resonance imaging (MRI) aids in identifying associated neurological abnormalities and can be safely used in children. This imaging modality may also detect communication channels between the globe and the cyst. Diffusion-weighted MRI and the apparent diffusion coefficient, in cases of rapidly enlarging cystic mass, may assist in differentiating it from a malignancy. Computed tomography (CT) scan is better for delineating osseous structures and is especially useful for surgical planning in hypoplastic orbits. CT-based 3-dimensional reconstruction is currently being utilized for presurgical planning. However, CT scans should be used cautiously in children due to a 0.1% risk of radiation malignancies.[27] Radiologically, the microphthalmic globe can be divided into mild (17 to 21 mm), moderate (12 to 16 mm), and severe (<12 mm) according to the axial length.[24][28] Similarly, the orbital cyst can also be classified as small (<10 mm), moderate (>10 mm to 20 mm), and large (>20 mm).[24]
Once the diagnosis is established by corroborating clinical-radiological and histopathological findings, the next step is to assess the visual potential of the eye. Approximately 80% of microphthalmia cases with a corneal diameter of less than or equal to 5 mm have no perception of light.[29] Electrodiagnostic tests such as visual evoked potential may be useful in cases of doubtful visual potential. Associated systemic abnormalities must be evaluated and addressed accordingly, along with a pediatric review.
Treatment / Management
There is a lack of concrete guidelines on managing microphthalmia with a cyst. Certain critical factors determine the basic approach toward managing this condition. Prime consideration should be given to the following:
- Age at presentation
- Volume of the orbit
- Pattern of the cyst growth
Visual and cosmetic rehabilitation should be initiated only after ensuring no visual potential in the microphthalmic globe. Orbital volume in an unaffected individual linearly expands up to 5 to 6 years of age, followed by a marked decrease in the rate in the subsequent years.[30] The presence of a cyst in a microphthalmia eye may contribute to the orbital expansion of the affected eye, thereby minimizing the interorbital asymmetry.[31] Hence, careful consideration should be given before surgically intervening in a child younger than 7.[32]
The indications of early cyst removal are as follows:
- Ill-fitting prosthesis or orbital wall displacement in the presence of the cyst
- Rapidly progressive cystic enlargement due to spontaneous or posttraumatic hemorrhage into the cavity. Dark red fluid (instead of the usual translucent yellow fluid) is revealed on examination
- Cyst prolapse through the palpebral fissure [33]
Conformer therapy must be initiated in a child younger than 7 after the patient’s first clinic presentation for best outcomes. For the first few months, a weekly follow-up is usually recommended. Serial augmentation of the conformer’s size with successive visits is necessary as the child grows. Customized, painted, or centrally hollow (when the vision is preserved) conformers are being worn lately. If the orbital volume is severely reduced (<85% compared to the contralateral side), using orbital expanders over rigid conformers is the preferred approach.[27]
Socket enlargement is directly proportional to the implanted volume in the socket. Compared to the rigid, static spheric implants made from silicone, orbital expanders (dynamic orbital implants) increase in volume to stimulate bony orbital growth in these hypoplastic juvenile sockets. An autogenous dermis fat graft, a natural biocompatible, slow-growing dynamic implant, is an effective option for socket reconstruction in a hypoplastic orbit.
There are 3 types of synthetic orbital expanders:
- Hard spherical implants: Patients with these implants often require subsequent surgeries, thereby undergoing repeated surgical trauma.[34]
- Inflatable soft tissue expanders: Saline-filled fluid chambers are fixed to the subperiosteal orbital space, and the filling port is attached subcutaneously in the temporalis fossa. Disadvantages include premature extrusion, uncontrolled directional expansion, and a painful injection.[35][36]
- Hydrogel implants: These solid hydrophilic expanders are made of methyl methacrylate and N-vinylpyrrolidone and may expand up to 30 times their original volume when hydrated. Although an appealing alternative, cessation of expansion on reaching the equilibrium and its long-term fragility are matters of concern.[37] These implants are available in spheric, hemispheric, and pellet forms.[26][38]
The integrated tissue expander, approved by the United States Food and Drug Administration in 2006, fulfills all basic criteria for an ideal expander with minimal tissue loss and subsequent surgical procedures. Since it is inserted through a lateral canthal incision, simultaneous prosthesis placement over an intact conjunctival surface may be performed. Surgically excising the cyst (in-toto) is the recommended method of removal; cyst aspiration may be performed before surgical removal or as a stand-alone procedure. A high recurrence rate limits its use as the first line of surgical treatment.[24][11] Few authors have advocated using concurrent sclerotherapy, using ethanolamine oleate, to enhance resolution rates.[39][40] Although a more comfortable approach, evidence regarding using sclerosants in microphthalmia with a cyst is scarce, and the potential fibro-inflammatory response may render the subsequent surgery extremely challenging.
In a severely microphthalmic globe (with no visual potential) with an associated cyst, excision may be combined with enucleation/evisceration followed by placement of an orbital implant (dermis fat graft, hydroxyapatite, Medpor porous polyethylene, or silicone) in the same setting. Any eyelid procedure or socket reconstruction using mucous membrane grafts should be reserved for the late phase of life. In patients with blepharophimosis and increased intercanthal distance, a combined Z-lateral canthoplasty and V-Y medial canthoplasty is an effective correction method. A secondary surgery in the earlier stage of life leads to cicatrix formation, resulting in poorer cosmesis. A customized prosthesis must be considered for better outcomes.[31] Orbito-cranial advancement surgery that allows for the advancement of bone forward and outward by bone grafts should be kept as a last resort in hypoplastic orbits.[41]
Differential Diagnosis
Congenital cystic eye, also known as anophthalmia with a cyst, is a close differential diagnosis of microphthalmia with a cyst; both conditions may present with a clinically invisible globe. Therefore, as discussed above, appropriate investigations must be performed to identify the presence of any ocular elements.[42] Unlike the cyst associated with microphthalmia, the cyst related to the congenital cystic eye has a predilection towards the upper and central part of the orbit. On histopathology, unlike microphthalmia, no rudimentary ocular structures are seen.
A sudden onset, rapidly progressive orbital mass may raise a suspicion of malignancy. Conditions such as a dermoid cyst, epidermoid cyst, lymphangioma, arachnoid cyst, meningocele, orbital teratoma, primary optic nerve sheath cysts, and encephalocele may mimic the intraorbital cyst associated with microphthalmia.[20] A meticulous evaluation with a dedicated work-up is paramount in these cases.
Prognosis
Microphthalmia with a cyst is associated with a poorer prognosis than other types of microphthalmia. The various prognosticating factors associated with an unfavorable prognosis include the following:
- Absence of visual potential confirmed on electrodiagnostic tests
- Severe disease
- Poor orbital volume
- Late age at presentation
- Avoidable cyst excision before age 7: Unless indicated, a cyst in a child younger than 7 years should be left untouched owing to its contribution to orbital growth.
- Early lid surgery and socket reconstruction (prepubertal)
- Enucleation/evisceration without orbital implants
- Discontinuation of expanders in early childhood/refusal to maintain the prosthesis
- Inability to maintain socket and prosthetic hygiene
- Infrequent follow-up visits [43]
Complications
Cosmetic disfigurement and absent visual potential are a few of the most worrisome complications of this complex disorder. Surgery-related complications include bleeding, secondary infections, extensive cicatrix formation postoperatively, contracted socket, recurrence, and orbital hematoma.[24] Graft-related complications include fat atrophy, lagophthalmos, pyogenic granuloma, malpositioned lids, and necrosis in the case of dermal fat grafts.[44] Notably, the incidence of fat atrophy is rare in the pediatric age group, making fat a viable alternative for volume replacement.[45][46] In children younger than 4, dermal fat grafts may grow, leading to proptosis, and may require surgical debulking.[45]
Consultations
Patients with microphthalmia with cyst require multidisciplinary consultations to ensure comprehensive care. Ophthalmologists and ocularists are essential for diagnosing the condition, assessing the extent of ocular involvement, and planning surgical interventions. Geneticists are crucial for evaluating the genetic basis of the disorder, identifying associated syndromes, and providing genetic counseling to families. Pediatricians are key in monitoring overall child development, managing systemic complications, and coordinating care. Plastic and reconstructive surgeons may be involved in addressing cosmetic concerns and enhancing orbital development. Additionally, consultations with a psychologist or counselor can help address the psychosocial impacts of the condition on both the patient and their family, ensuring holistic care.
Deterrence and Patient Education
Microphthalmia with a cyst is a challenging entity. While the condition is congenital and cannot be entirely prevented, educating families on the importance of early diagnosis and intervention can significantly improve outcomes. Genetic counseling is essential to inform parents about the risks of recurrence in future pregnancies and to address potential genetic testing. Patient and parent education plays a significant role in addressing the aesthetic, functional, and psychosocial ramifications. Maintenance and disciplined use of conformer therapy and orbital expanders should be encouraged. Proper counseling helps the family understand the condition's prognosis. The value of a regular follow-up with the surgeon, the ocularist, and the rehabilitation team should be explained to the patient and their family. Even with minimal visual potential, cosmetic and visual rehabilitation is essential for significantly better outcomes.[47]
Pearls and Other Issues
Microphthalmia with a cyst is a congenital malformation. However, the associated cosmetic and functional disability can be minimized if appropriate measures are taken at every step. As opposed to losing an eye in adulthood, an early loss in childhood results in hypoplasia and volume loss of the affected orbit; this leads to distorted orbital-facial growth, rendering the management more challenging. Hence, an early presentation and timely intervention are recommended to effectively manage this condition. Another issue is the loss of follow-up and the parents' unwillingness to place a conformer/orbital expander/prosthesis in the child's orbit. The importance of close monitoring of the orbital growth and volume and the need for these therapeutic measures to minimize asymmetry and achieve desirable aesthetic and functional outcomes should be emphasized.
Enhancing Healthcare Team Outcomes
Effectively managing microphthalmia with a cyst requires an interprofessional approach involving the collaboration of physicians, advanced clinicians, nurses, pharmacists, and other healthcare professionals. Each role contributes uniquely to enhancing patient-centered care, improving outcomes, ensuring patient safety, and optimizing team performance. Clinicians and advanced clinicians lead diagnosis and treatment, while nurses provide ongoing patient care and support. Pharmacists ensure the safe administration of medications, particularly in managing pain and post-surgical care. All team members share the responsibility for patient education and advocacy.
A well-coordinated strategy is necessary for managing patients with microphthalmia with a cyst. This includes establishing standardized protocols for diagnosis, treatment, and follow-up care. Early intervention strategies, including timely genetic testing and surgical planning, are crucial for optimizing visual and cosmetic outcomes. Care coordination is vital in managing the complex needs of affected patients. This involves scheduling timely consultations with various specialists, coordinating surgical and therapeutic interventions, and ensuring consistent follow-up care. Effective care coordination minimizes the risk of complications and enhances patient safety.
Improving patient outcomes involves addressing the immediate medical needs and focusing on long-term quality of life. This includes optimizing visual function, ensuring cosmetic results, and providing psychosocial support. Addressing psychosocial issues, connecting with the patient’s family, setting up futuristic goals and endpoints, and increasing awareness regarding important time frames in a child’s life will maximize the outcomes. Regular outcome assessments help refine treatment strategies and achieve better results. Continuous education on emerging research and best practices is essential to providing high standards of care. Regular training, team-building exercises, and performance evaluations help maintain an effective, cohesive team that delivers the best possible care for affected patients and families.