Continuing Education Activity
Neutrophilia is defined as a higher neutrophil count in the blood than the normal reference range of absolute neutrophil count. Neutrophilia can be seen in infections, inflammation, and/or neoplastic processes. Further evaluation is often necessary. An absolute neutrophil count (ANC), defined as the percent of neutrophils in the bloodstream and adults, typically ranges between 2500 to 7000 neutrophils/microL. An increase in the WBC count of more than 11,000 cells/microL is defined as leukocytosis. Neutrophilia is the most common type of leukocytosis and is defined as an increase in the absolute neutrophil count of approximately more than 7700 neutrophils/microL (11,000 cells/microL x 70 percent), i.e., two standard deviations above the mean. This activity reviews the pathophysiology, causes, evaluation, and treatment of neutrophilia and highlights the role of the interprofessional team in evaluating and treating patients with neutrophilia.
Objectives:
- Review the pathophysiology of neutrophilia.
- Identify the etiologies of neutrophilia.
- Describe the common physical exam findings in patients with neutrophilia.
- Outline how an interprofessional team can coordinate care to treat patients with neutrophilia and obtain the best outcomes.
Introduction
Neutrophils are historically defined as "soldiers of our innate immune system." They are the first line of cells recruited at the site of infection and attack, ingest, and digest microorganisms by producing reactive oxygen species.[1] They also play a vital role in acute and chronic inflammatory settings and autoimmune disorders.[2] In adults, the approximate normal range of white blood cell (WBC) count is 4000 to 11,000 cells/microL, out of which 60% to 70% are mature neutrophils circulating in peripheral blood.[3]
An absolute neutrophil count (ANC), defined as the percent of neutrophils in the bloodstream and adults, typically ranges between 2500 to 7000 neutrophils/microL. An increase in the WBC count of more than 11,000 cells/microL is defined as leukocytosis. Neutrophilia is the most common type of leukocytosis. It is defined as an increase in the absolute neutrophil count of approximately more than 7700 neutrophils/microL (11,000 cells/microL x 70 percent), i.e., two standard deviations above the mean.
Etiology
Causes of Neutrophilia are classified into the following categories:
- Factitious neutrophilia; neutrophilia due to various artifacts encountered during blood sample handling in laboratory settings
- Primary Neutrophilia; neutrophilia due to abnormal increased neutrophils production by bone marrow due to impaired neutrophil production regulation.
- Secondary Neutrophilia; reactive neutrophilia can respond to a wide variety of stimuli mentioned in detail below.
Factitious Neutrophilia
Factitious neutrophilia can be seen in the blood samples that are either inadequately anticoagulated with citrate or heparin or are EDTA- based anticoagulated, causing platelet clumping in an automated cell counter leading to falsely elevated neutrophil count. A repeat blood sample with adequate anticoagulation (with heparin or citrate) and an examination of the peripheral blood smear (showing platelet clumping) can help resolve this problem.[4][5] Another possibility in which neutrophil count can be falsely elevated is precipitated cryoglobulin particles in a blood sample. Cryoglobulin is a cold insoluble protein, and a repeat blood sample at body temperature should resolve this issue.[6]
Primary Neutrophilia
Chronic Idiopathic Leukocytosis: Given neutrophilia is defined as an ANC of at least two standard deviations above the mean, neutrophil counts can vary considerably among asymptomatic healthy individuals, and 2.5 percent of the population can be considered to have neutrophilia based on the definition mentioned above. Serial evaluations may be required in an average healthy individual with mild neutrophilia to rule out the absence of underlying pathology. Since neutrophil count regulation is also genetically controlled, evaluation of a sibling's or parent s blood count can be helpful in this situation.[7]
Myeloproliferative Neoplasms (MPN): MPNs are characterized by excess and autonomous production of red blood cells, white blood cells, and platelets, thus can be a cause of primary neutrophilia. MPNs associated with neutrophilia include Chronic myeloid leukemia (CML), essential thrombocythemia (ET), polycythemia vera (PV), chronic myelomonocytic leukemia, chronic neutrophilic leukemia, Juvenile myelomonocytic leukemia (JMML).[8][9]
Genetic/ Inherited neutrophilia: The subset of the population affected by this category is neonates and children, with some disorders being detected in adulthood. Leukocyte adhesion factor deficiency is a rare but life-threatening disorder characterized by a defect in leukocyte adhesion molecules, leading to marked leukocytosis, recurrent infections, and delayed umbilical cord separation.[10] Other causes include congenital anomalies and leukemoid reaction, transient myeloproliferative disorder [TMD] of Down syndrome, familial cold urticaria, and leukocytosis, hereditary chronic neutrophilia (also known as chronic neutrophilic leukemia).[11][12]
Secondary Neutrophilia
Infection/Inflammation; The most common cause of secondary neutrophilia is infection and inflammation. Bacterial infections are usually associated with left shift (i.e., an increase in the percentage of band forms of leukocytes), toxic granulations, and Döhle bodies on peripheral smear.[13] Whereas viral infections may have a high neutrophil count with atypical lymphocytes. Worth mentioning here is a leukemoid reaction, i.e., WBC count of more than 50,000 cells/microL, caused by various infections such as clostridium difficile, tuberculosis, and medications such as ATRA and some nonhematological malignancies. It is essential to distinguish leukemoid reaction from acute leukemia, which is a hematological malignancy. Both acute and chronic inflammation can lead to neutrophilia, to name a few, including Still disease of young, juvenile, and adult-onset rheumatoid arthritis, granulomatous disease, vasculitis, myositis, chronic hepatitis, and inflammatory bowel disease.[14]
Nonhematological neoplasms: Neutrophilia can be seen in solid tumor malignancies. Mechanisms leading to increased neutrophil count can be a paraneoplastic leukemoid reaction, bone marrow metastasis, nonspecific tumor-related inflammation, infections, and high-dose corticosteroids for tumor therapy.[15]
Medications: Many medications can cause neutrophilia by various mechanisms, some of which are listed below.
- Recombinant granulocyte and granulocyte-macrophage colony-stimulating factors (G-CSF or GM-CSF), All-trans retinoic acid; Increase neutrophil count via direct stimulation of bone marrow myelopoiesis.
- Glucocorticoids, Plerixafor; Increase neutrophil count by causing the release of granulocytes from the bone marrow into circulation.
- Other drugs include lithium and catecholamines.
Many medications can cause neutrophilia due to adverse drug reactions, i.e., allergic or inflammatory responses to a drug.
Others: secondary neutrophilia may also result from various stimuli. These stimuli may include physical or emotional stress, vigorous exercise, temperature changes, seizure activity, cigarette smoking, surgery, obesity, asplenia or hyposplenism, and generalized bone marrow stimulation, such as in hemolysis.[16][17][18]
Epidemiology
There is a limitation in predicting which patients are at increased risk of developing neutrophilia, given multiple contributing factors. Certain social factors like smoking status, stress, and exercise level can also impact neutrophilia risk. There are more consistent ethnical differences among patients with neutropenia than neutrophilia patients; relative to white people, black people have a lower total WBC count and lower neutrophil count. However, the Latino population is noted to have a higher leukocyte count (mean difference 0.16×10^9/L) and higher neutrophil count (mean difference 0.11×10^9/L) compared to the white population.[19]
Pathophysiology
Circulating neutrophils are mature neutrophils in transit from the bone marrow into the peripheral blood. The life span of neutrophils in bone marrow is approximately ten days, 2 to 3 days in peripheral tissue, and approximately less than 24 hr. in circulation.[20] The production, proliferation, differentiation, and entry of neutrophils in peripheral blood are tightly regulated by cytokines and controlled by various transcription and growth factors.[21][22][23] Neutrophilia can be due to aberrant neutrophils' production by the bone marrow, demargination of neutrophils into the bloodstream, and reactive response to infection, inflammation, and allergic reaction to the medication.
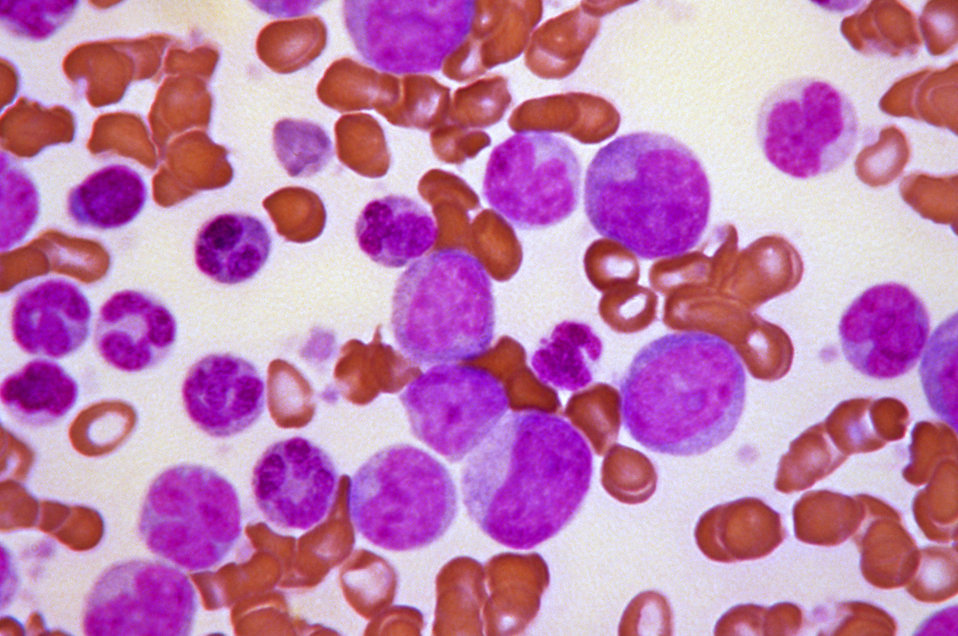
Histopathology
Examination of peripheral blood smears can be beneficial in distinguishing various causes of neutrophilia. Platelet clumping can be seen on peripheral smears in factitious neutrophilia. Myelocytes, metamyelocytes, and increased band forms are seen in severe infections or CML. The presence of toxic granulations and Dohle bodies can also be seen in various infectious and inflammatory states.
Granulomatous diseases are characterized by granulomata, which are defined as the localized accumulation of activated epithelioid macrophages. In Leukocyte adhesion factor deficiency(LAD), marked neutrophilia accompanied by mild lymphocytosis can be seen even in the absence of any ongoing infection. If there is an ongoing infection, then biopsies of infected tissues can show inflammatory infiltrates devoid of neutrophils.
History and Physical
History should be focused on the following:
- Evidence of active or prior infection and or inflammation
- Prior complete blood count (CBC) results
- Any recent medication changes
- Evaluation of hematological or non-hematological malignancies (recent weight loss, decreased appetite, swollen glands, new palpable mass, generalized body ache, fatigue, night sweats, fever or new cold symptoms, etc.)
- Family history of neutrophilia
- History of vigorous exercise, cigarette smoking, new physical or emotional stress
- History of functional or surgical asplenia
Physical examination, in general, should be comprehensive and focus on ruling out above mentioned history clues.
- Vitals assessment for fever, tachycardia
- Head and neck examination for facial and conjunctival pallor and lymphadenopathy
- Pulmonary examination for decreased breath sounds or any added breath sounds
- Abdominal examination for abdominal distention, tenderness, mass, and hepatosplenomegaly
- Musculoskeletal examination for joints erythema, tenderness, swelling, and or deformity
- Skin examination for any new lesions, nodules, and color changes
Clinical manifestations in LAD are periodontitis, recurrent skin and mucosal infections, absent pus formation, poor wound healing, and delayed umbilical cord separation.
Evaluation
CBC and peripheral blood smear: Evaluation of neutrophilia can be started by reviewing CBC with differential and confirming automated differential with a manual by reviewing peripheral blood smear. A peripheral blood smear review can also help differentiate causes of neutrophilia, as mentioned above in the histopathology section.
Other Laboratory Studies
Certain laboratory studies can help us distinguish primary versus reactive neutrophilia, such as
- Inflammatory markers, including ESR, CRP, LDH, ferritin
- Liver and renal function tests.
- Coagulation profile including APTT, PT/INR, fibrinogen, D dimer
- Blood culture, sputum culture, urine culture, wound culture, stool culture, and cerebrospinal fluid analysis (chemistry, histopathology, and culture).
- Clostridium difficile testing
Special Tests
Other tests that can help diagnose neutrophilia once CBC and peripheral blood smear have been reviewed are bone marrow biopsy, flow cytometry, and molecular/genetic testing.
- Bone marrow biopsy helps establish the diagnosis of various hematological and non-hematological malignancies invading bone marrow. The biopsy can be utilized to run morphological analysis, flow cytometry, and molecular testing.
- Flow cytometry can help diagnose various MPNs, such as CML, PV, and ET, by immunophenotyping peripheral blood.
- LAD can be diagnosed by molecular testing and or flow cytometry.
Imaging
Imaging that can help differentiate causes of neutrophilia include.
- Computed tomography (CT) of the head and neck, chest, abdomen, and pelvis.
- Magnetic resonance imaging of the head and neck, chest, abdomen, and pelvis if CT was inconclusive
- Positron emission test PET scan
- Chest Radiography
- Diagnostic ultrasonography
Treatment / Management
Treatment of neutrophilia is based on treating the underlying cause of neutrophilia. In a leukemoid reaction where the WBC count is more than 50,000, emergent leucopheresis, aggressive hydration, and cytotoxic therapy with hydroxyurea are indicated to prevent hypercoagulability-associated complications. Antibiotic and anti-inflammatory therapies should be undertaken for neutrophilia associated with infection/inflammation.
Medications noted to cause neutrophilia should be carefully monitored and may need to be discontinued if leading to complications. MPNs are usually treated with cytoreductive drugs; the commonly used is hydroxyurea with serial monitoring of CBC. Specific treatment options for CML include tyrosine kinase inhibitor (TKI) therapy with imatinib which inhibits bcr-abl tyrosine kinase, the abnormal gene product of Philadelphia chromosome t (9;22) in CML, and allogeneic hematopoietic stem cell transplant (HCT).[24][25][26]
Referral to a hematologist should be considered as a part of the workup for MPNs.
Differential Diagnosis
Differential diagnosis of neutrophilia includes:
- Infections including bacterial, viral, fungal, and parasitic
- Acute and chronic inflammation, e.g., granulomatous diseases, vasculitis, inflammatory bowel disease
- Leukemoid reaction
- Hematological and non-hematological malignancies
- Medications
- Asplenia or hyposplenia
- Physical and emotional stimuli (stress, active smoking, vigorous exercise, pregnancy, obesity)
- Tissue damage, e.g., surgery, trauma, burns
- Laboratory artifacts
- Inherited causes like LAD, hereditary neutrophilia
Prognosis
The prognosis of neutrophilia depends on the prognosis of the underlying cause of neutrophilia. Neutrophilia seen in infection/inflammatory state resolves with treatment of these states. Neutrophilia associated with medications can also resolve once either treatment is over or the drug is discontinued. The prognosis in CML has been drastically improved with the introduction of TKIs, including Imatinib and HCT.[27] HCT has also successfully improved survival in LAD patients.[28]
Complications
Complications of neutrophilia are those that are of the causes of neutrophilia, such as
- Hypercoagulability associated with leukemoid reactions
- Bacteremia, septic shock, and multiorgan failure in untreated infections
- Impaired wound healing, severe periodontitis, severe mental impairment, and failure to thrive in untreated LAD
- Thrombosis, hemorrhage, transformation to acute leukemia, and fibrosis are seen in untreated MPNs[29][30]
Consultations
An infectious disease specialist should evaluate patients with infection-associated neutrophilia both in inpatient and outpatient settings. Hematology/Oncology consultation should be considered in patients with hematological and non-hematological malignancies associated with neutrophilia. To rule out LAD, a pediatric consultation should be considered in children presenting with poor wound healing, periodontitis, and repetitive infections.
Deterrence and Patient Education
Educate patients about smoking cessation, weight loss, balanced diet, and relaxation techniques for neutrophilia seen in various physical and emotional stimuli. Educate patients about the side effects of medications like ATRA, lithium, and G CSF that can cause neutrophilia.
Enhancing Healthcare Team Outcomes
Due to the complexity of this condition, management of neutrophilia-associated conditions requires an interprofessional team of health care professionals, including hospital physicians, primary care physicians, specialists including infectious disease specialists, hematologists/oncologists, pediatricians, microbiologists, specialty-trained nurses, and pharmacists working together collaboratively to enhance patient-centered care and improve outcomes. Specialists should recommend treatment options, including antimicrobials, cytoreductive therapies, leucopheresis, immunotherapy, and HCT. Pharmacists should review the indication, dosage, interactions, and contraindications of medications. Nurses taking care of these patients should monitor signs and symptoms associated with neutrophilia-related conditions and report emergent concerns to hospitalists and specialists. Thus, the morbidity and mortality related to neutrophilia-related conditions can be lowered through an interprofessional team approach. [Level 5]