Continuing Education Activity
Inferior vena cava syndrome (IVCS) is caused by physical invasion or compression by a pathological process or by thrombosis within the vein itself. This activity reviews the evaluation and management of inferior vena cava syndrome and highlights the role of the interprofessional team in evaluating and improving care for patients with this condition.
Objectives:
- Review the risk factors for developing inferior vena cava syndrome.
- Describe the pathophysiology of inferior vena cava syndrome.
- Explain the common physical findings associated with inferior vena cava syndrome.
- Outline the importance of improving care coordination among the interprofessional team to enhance the delivery of care for patients with inferior vena cava syndrome.
Introduction
Inferior vena cava syndrome (IVCS) is a sequence of signs and symptoms that refers to obstruction or compression of the inferior vena cava (IVC). The pathophysiology of IVCS is similar to superior vena cava syndrome (SVCS) because of the presence of an underlying process that inhibits venous return to the right atrium. IVCS is not a primary diagnosis because it is often caused by other underlying pathologies.[1]
Symptoms and signs of IVCS result from a reduced venous return to the heart, as well as a pooling of blood in the IVC, which causes hypotension, tachycardia, lower extremity edema, elevated liver enzymes, end-organ failures and, hypoxia, altered mental status, and death.[2] IVCS is less frequently found in comparison with the superior vena cava syndrome.
Etiology
The etiology of inferior vena cava syndrome (IVCS) depends on the interrupted blood flow location. The pathogenesis of IVCS is divided into two events, including the vena cava obstruction and compression by adjacent structures. The obstruction of the IVC is mostly caused by a primary thrombotic event[1], either congenital or acquired. Congenital thrombosis of the IVC is often asymptomatic which is caused by well-developed collaterals. In contrast, acquired etiologies include spontaneous thrombosis of the vessel either due to external compression or pathological changes of the IVC wall.[1] Thrombosis of the IVC can be due to the propagation of a clot from deep venous thrombosis or from the extension of a thrombus.[1] In addition, conditions that increase the obstruction risk of IVCS are malignancy, pregnancy, infection, obesity, or other intrinsic vein disease.
Malignancies of organs near the IVC, such as renal cell carcinoma[3], gastric adenocarcinoma[4], pancreatic adenocarcinoma[5], primary or metastatic hepatic malignancies or tumor of any organ surrounding the IVC can compress the IVC which leads to obstruction of venous return to the heart. Thus, it causes venous pooling and decreases heart preload. Tumor compression results in thrombosis can sometimes lead to the development of superior vena syndrome in conjunction with IVCS.[6]
In pregnancy, the distended uterus can compress the IVC which leads to obstructing the blood flow to the heart and causes increased venous congestion or pooling.[7] Obesity may also be implicated as an etiology of IVCS. A study showed an association between increased body mass index (BMI), greater than 30 kg/meter square, with increased pressure gradients between the thoracic and abdominal vena cava[8] in patients with signs and symptoms of IVCS.
IVCS can also be due to congenital malformations such as May-Thurner syndrome or Budd-Chiari syndrome. May-Thurner syndrome is a chronic condition in which anatomical variations of vessels in the iliocaval region cause blood flow obstruction.[9] Budd-Chiari syndrome can be classified as primary or secondary. The primary classification refers to any obstruction of the hepatic vein due to a primarily venous process such as thrombosis or phlebitis. In comparison, secondary relates to compression of the hepatic veins due to external lesions such as cancer.[10]
IVCS can also be caused by iatrogenic processes such as IVC filter placement and venous catheters, which promotes thrombosis[1]. In addition, solid organ transplant or surgery, such as hepatic lobe resection can also increase the risk of thrombosis.[2] Evidence from the literature supports that other disease processes, such as cholelithiasis[11] and retroperitoneal hemorrhage.[12], can cause obstruction or compression of the IVC. Hepatic vena cava syndrome, which is associated with poor-hygiene causing bacterial infection leading to thrombophlebitis of the hepatic veins near the IVC outflow tract, is also recognized as an etiology of IVC syndrome.[13]
It has been observed that using Broviac central venous hyperalimentation catheters in pediatric children and teens who need IV therapy usually for an extended period can develop IVC syndrome.[14]
Epidemiology
Because inferior vena cava syndrome (IVCS) is not a primary diagnosis, it is difficult to truly quantify the incidence because of different underlying pathologies. Reported IVCS shows frequencies of 4 to 15% to an association with deep vein thrombosis.[15] Case reports that have been published stated that gastric cancer, renal cell carcinoma, pancreatic cancer, and liver pathology caused IVCS.[4][3][5][13] However, the exact incidence has never been reported.
Pathophysiology
The inferior vena cava (IVC) returns blood to the heart, along with superior vena cava (SVC). Obstruction or compression to the IVC reduces the venous return to the heart, causing an imbalance in the hemodynamic equilibrium. Decreased venous return causes hemodynamic instability in several ways. When there is a decrease in venous return, it will decrease the oxygenation of the blood, which results in hypoxia and subsequent tachycardia. Besides, decreased venous return causes a decrease in heart preload, which leads to decreased cardiac output, and the heart compensates by beating rapidly to maintain adequate perfusion to end organs.[16]
Thrombosis of the IVC can be caused by either compression or physical obstruction, which leads to venous stasis. Venous stasis is one of the three criteria of Virchow's triad of thrombus formation; the other two: hypercoagulable state and endothelial damage. The impedance in blood flow causes stasis, which promotes thrombus formation.[17]
The decreased venous return in inferior vena cava syndrome (IVCS) mimics the presentation of hypovolemic shock and causes tachycardia, diaphoresis, hypotension, shortness of breath on exertion, dizziness, and cold extremities. IVC congestion causes pallor, ascites, lower extremity peripheral edema, and hypoxia. IVCS also presents with generalized symptoms such as nausea, headache, malaise, and fatigue. In extreme cases, the decreased blood, either through thrombotic or non-thrombotic mechanisms, can lead to altered mental status and even death.[16]
History and Physical
Inferior vena cava syndrome (IVCS) is not a primary diagnosis but is a consequence of any underlying pathology. As described in the pathophysiology section, the presentation of IVCS is dependent on the patient’s comorbidities and underlying diseases. Accurate diagnosis is based on a thorough history taking and physical examination.
The symptoms which a patient shows are in accordance with the pathophysiology of IVCS. It is important to inquire about other signs and symptoms, such as fatigue, dizziness, weight loss, abdominal pain, night sweats, anorexia, palpitations, diaphoresis, dizziness, shortness of breath on exertion. In addition, the history taking also has to get deep into previous illness history, including the history of abdominal surgeries, organ transplantation, lower extremity swelling and pain, family and past medical history of coagulopathy, prior deep venous thrombosis (DVT), as well as occupation and lifestyle.
A thorough physical examination will assist in the accurate diagnosis of IVCS. The vital signs will usually reveal hypotension, tachycardia, and possibly tachypnea with hypoxia. Signs of anemia, such as pallor or pale conjunctiva, might be the earlier sign of malignant disease, and with additional constitutional symptoms of malignancy can lead to the diagnosis of IVCS.
While there are no specific tests with pathognomonic findings of IVCS, certain findings such as lower extremity edema, signs of DVT and pulmonary embolism (PE), cold and clammy extremities, abnormal neurological exam, hepatomegaly, and abdominal distention, lead to the decrease of venous return which then impair the perfusion of end organs.
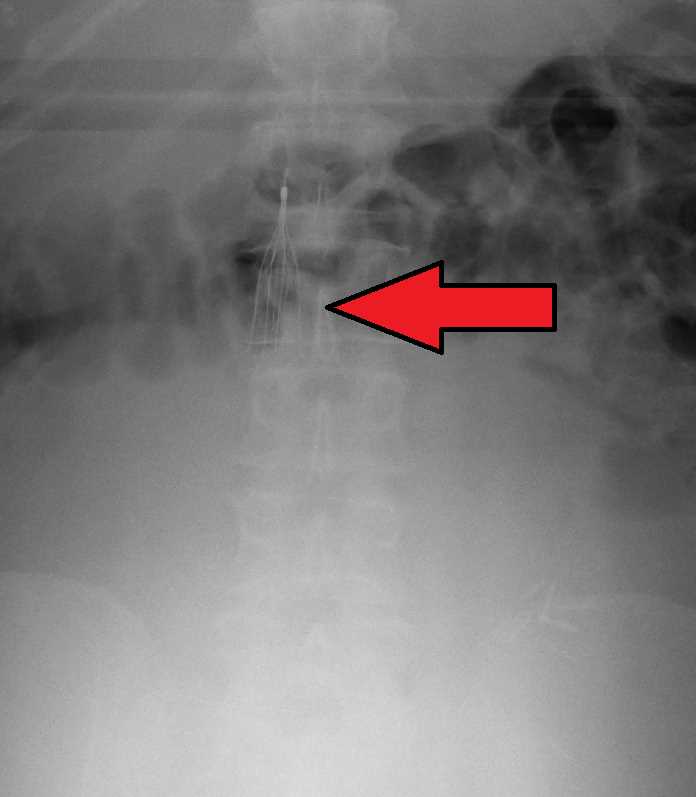
Evaluation
Duplex ultrasound is the first line of modality can be used in a hemodynamically unstable patient. It is a rapid, accurate, and non-invasive modality to investigate the etiology of IVC obstruction. However, interference, i.e. obesity, limits the use of ultrasound in identifying the cause of obstruction. Esophagogastroduodenoscopy can also be used to reveal esophageal, gastric, or duodenal pathologies, especially tumor which compresses the IVC.[4]
CT abdomen and pelvis can then be used as an alternate non-invasive modality. Contrast venography, the standard for diagnosis, is used to assess the thrombotic obstructions of the abdomen in hemodynamically stable patients. Although it is an invasive procedure, it gives the most accurate finding of IVC obstruction and compression. Magnetic resonance (MR), a non-invasive but expensive instrument, can also be used to access obstruction of the IVC in hemodynamically stable patients and is replacing CT scans. Etiologies should be urgently obtained in hypotensive patients in order to prevent complications.[1]
Treatment / Management
The guideline treatment of inferior vena cava syndrome (IVCS) has not been clearly described. Therefore, treatment and management are determined by the etiology of the causative lesion and tailored to a patient’s condition. If the lesion is thrombotic, immediate treatment is focused on the prevention of propagation of the clot, causing a pulmonary embolism, and management of pain, edema, and the resulting hypotension. Either medical or surgical intervention can accomplish this. Medical treatments include anticoagulation using either low-molecular-weight heparin (LMWH), fondaparinux, or direct thrombin inhibitors. These medications reduce the buildup and propagation of the thrombosis but do not eliminate the primary thrombosis.
Endovascular procedures can subsequently be utilized to facilitate the introduction of thrombolytics to lyse the clot. These can include catheter-directed thrombolysis, pulse-spray pharmaco-mechanical thrombolysis, and then angioplasty with or without inserting stents, which increases patency of the IVC. Performing such procedures is required within a short period (within 14 days) of the onset of symptoms to minimize complications and decrease mortality rates. Surgical modalities such as thrombectomy, bypass, reconstruction/replacement, and ligation are used as a last resort due to the high invasive and significant intervention nature.[1]
If the stent placing is not advisable, placing IVC filters can alleviate symptoms for some time.[6] Recently, the use of IVC filters has increased, especially in advanced-stage cancer patients, in order to prevent the pulmonary embolus, although there is no explicit evidence of improved survival rate.[18] Temporary IVC filters are usually used in cancer patients during systemic chemotherapy.[19]
If lesions are due to non-thrombotic etiologies such as malignancy, then the treatment is directed to manage the underlying cause of the compression. This may include surgery, chemotherapy, radiation, or combination. Resection is a surgical option to remove tumor compression. However, resection is not possible to be done in unstable patients, thus, palliative care is provided. Another option is to place an intravascular stent or surgical bypass grafting, which increases the patency of the IVC to alleviate symptoms.[1][20] Recanalization of the occluded veins is usually done by implanting the metallic stents into the IVC from the superior vena cava via the right atrium.[21]
IVCS patients of intrahepatic obstruction due to malignant hepatic enlargement are usually treated using strip radiotherapy to the intrahepatic IVC, with or without a hepatic arterial infusion of chemotherapy.[22] The IVC obstruction is generally managed by crossing the tumorous lesion with either a guidewire or Brockenbrough needle along with a Mullins sheath assembly, and then a balloon dilatation was done with the help of Inoue or Mansfield balloon.[23]
In some mild compression etiologies like pregnancy, physical maneuvers to move the uterus away from the IVC can be applied.[7]
Differential Diagnosis
Inferior vena cava syndrome (IVCS) is characterized by tachycardia, hypotension, tachypnea, hypoxemia, and shortness of breath. The differential diagnosis of IVCS is broad, mainly because it is rarely ever diagnosed as a primary disease process. The differential diagnosis of IVCS are:
- Chronic venous insufficiency
- Shock
- IVC compression
- Malignancy[5]
- Deep vein thrombosis
- Iliocaval syndrome
- Aortocaval syndrome[7]
Prognosis
Prognosis of inferior vena cava syndrome (IVCS) depends on the underlying patient condition, including the hemodynamic status of the patient, the severity of compression or vein obstruction, the grading of the malignancy, and previous comorbidities. The outcome of patients who have inferior vena cava thrombosis overall relates to the embolic risk associated with DVT. If the IVC is occluded, pulmonary embolism does not present a significant risk. However, if the IVC lumen remains, embolization may occur.
Complications
Complications of inferior vena cava syndrome (IVCS) depend on the underlying comorbidity and patient's risk factors for the following but include:
- Pulmonary embolism (PE)[24]
- Deep vein thrombosis[25]
- Chronic venous insufficiency (CVI)
- Post-thrombotic syndrome (PTS) progressing to venous ulceration, venous gangrene
- Hemodynamically instability[1] leading to cardiac arrests and possibly death.
Deterrence and Patient Education
Patient education should be focused on modifiable risk factors and finding the etiology of the syndrome. Patients with an increased risk of thrombosis such as pregnancy, obesity, oral contraceptive pills (OCPs), smoking, venous insufficiency, immunocompromised, diabetes, or hypertension are at risk for developing obstruction of the IVC and an increased risk of malignant neoplasm development. Education needs to be tailored more towards mobility, weight loss, dietary modification, smoking cessation, stop alcohol consumption, and a healthier lifestyle.[15]
Pearls and Other Issues
Inferior vena cava syndrome (IVCS) is not a primary diagnosis, but rather a diagnosis of exclusion. It mimics a variety of etiologies, and the signs and symptoms can overlap with other lethal conditions. So a prompt diagnosis can prevent significant morbidity and mortality. In addition to imaging, a thorough history and physical examination are vital to the diagnosis of IVCS. Although IVCS can predispose to thrombus formation, it protects against pulmonary embolism coming from the lower limbs deep vein thrombosis.[26]
Enhancing Healthcare Team Outcomes
Because of inferior vena cava syndrome (IVCS) is not a primary diagnosis; it is often missed and leads to adverse outcomes for the patients. Superior vena cava syndrome (SVCS) is a better-recognized entity because of its specific presentation: right upper extremity swelling with skin discoloration and signs of decreased blood return to the right heart. In contrast, IVCS causes bilaterally lower extremity swelling, which can be misdiagnosed as congestive heart failure exacerbation, nephrotic syndrome, lymphangitis, or varicose veins.
IVCS can also be accompanied by symptoms consistent with hemodynamic instability, which can mimic several conditions such as circulatory shock, cardiogenic shock, pulmonary embolism, acute heart failure, acute pulmonary edema, etc. As a result, the responsibility of the entire interprofessional team, which includes both primary care providers, specialists such as trauma surgeons, transplant surgeons, hematologists, oncologists, and general surgeons, to name a few, nurses, social workers, pharmacists to counsel regarding medications that can cause prothrombotic states to advise the patients on how to reduce the risk of thrombosis, counsel on the importance of medications compliance if the patient is on anticoagulation or antiplatelet therapy, and to promote lifestyle modifications to reduce the risk of thrombosis as well as obstruction of the IVC, which can cause severe morbidity and increased risk of mortality.