Continuing Education Activity
The retrobulbar block, initially described in 1884, had been widely referred to as the "gold standard" in ophthalmological surgery for many years. Though its rates of adverse effects are low, the introduction of newer techniques with potentially less adverse effects and similar anesthetic profiles has relegated the use of this regional anesthesia technique. This activity reviews the indications, contraindications, and potential complications of the retrobulbar blockade and highlights the role of the interprofessional team in improving the care of patients undergoing ophthalmological surgery.
Objectives:
Identify the anatomical structures, indications, and contraindications of a retrobulbar block.
Select the equipment, personnel, preparation, and technique regarding the retrobulbar block.
Identify the potential complications and clinical significance of the retrobulbar block.
Assess the interprofessional team strategies for improving care coordination and communication to perform a retrobulbar block and improve outcomes.
Introduction
The retrobulbar blockade was first described by Herman Knapp in 1884. That same year, Carl Koller reported a case of successful ocular enucleation using cocaine hydrochloride as an anesthetic agent. Years later, Atkinson (1936) described a retrobulbar technique that rapidly became popular; however, the high incidence of complications made this technique obsolete over time. Since then, several anesthesia techniques for ophthalmological surgery have been added to the repertoire of the anesthesiologist.
Modern techniques for retrobulbar blockade have long been considered the gold standard for akinesia and anesthesia in intraocular surgery. However, complications related to this technique, though rare, are devastating and potentially life or sight-threatening. Therefore, some providers have replaced this block with newer techniques with theoretically less severe complications, such as peribulbar blockade and the Sub-Tenon block, which has a similar profile for anesthesia and akinesia as a retrobulbar blockade. Despite this, some still prefer local anesthesia over regional blocks for certain ocular procedures.[1]
Anatomy and Physiology
Basic comprehension of orbital anatomy and structural relations is paramount to understanding the mechanism of action and potential complications of the retrobulbar block. Generally, the orbital space can be divided into 2 compartments that communicate freely. The intraconal compartment encloses the orbital fat, ciliary ganglion, ophthalmic artery, several cranial nerves (optic, oculomotor, abducens), and a nasociliary branch of the ophthalmic nerve. The extraconal compartment consists of orbital fat, lacrimal gland, abducens nerve, and the frontal branches of the ophthalmic nerve.
Orbits: Despite the classical description of the orbits as pyramidal in shape, their walls are irregular, curvilinear, and perforated by fissures and foramina at their apex. Orbit height can be around 35 mm at the rims, with an approximately 40 mm width and 42 to 54 mm depth from the optic foramen to the orbital rim. For this reason, using needles more than 38 mm for the retrobulbar blockade is not advisable. The medial orbital wall is thin from the apex to the base; it is separated from the ethmoid sinus by the lamina papyracea. Perforation of this lamina with a needle may result in an abscess or orbital cellulitis.[2]
Ocular globe: The eyeball is spherical and lies anteriorly in the orbital cavity. It has an axial length of 25 mm, an essential anatomical characteristic to consider when planning a retrobulbar blockade. Myopia increases the anterior to the posterior diameter of the eyeball. Several studies have shown that more than 26 mm axial length is associated with a higher risk of ocular globe perforation. The presence of staphylomas (protruding defects of the sclera lined with uveal tissue), which typically lie in the posterior or inferior surface of the ocular globe, is also associated with higher perforation risk.[3]
Extraocular muscles: Six muscles control ocular globe movements; four of them are the rectus muscles (superior, inferior, lateral, and medial), and the other two are the oblique muscles (inferior and superior). The rectus muscles are inserted anteriorly into the sclera, where their tendons join in the intraconal space, forming the Zinn ring that encircles the optic canal. Ample fat-filled space, devoid of major anatomical structures, is created by diverting the medial rectus from the medial orbital wall, making it an ideal area for infiltration.
Motor and sensory innervation: The oculomotor nerve provides motor innervation of the inferior oblique and rectus muscles, except the lateral rectus. The trochlear nerve innervates the superior oblique muscle. This nerve exits the annulus and runs along the muscular surface, typically unaffected by inferotemporal blocks. The orbicularis muscle is innervated by the facial nerve, which frequently must be blocked to prevent blinking during surgery. For this reason, a van Lint block is used at the same time as the retrobulbar block. Sensory innervation of the eye is majorly provided by the first branch of the trigeminal nerve (V1) and its branches (frontal, lacrimal, and nasociliary). The lacrimal and frontal branches of V1 innervate the peripheral conjunctiva. However, these branches run in the extraconal space; thus, the intraconal blockade will not provide any anesthetic effect in these branches. The second branch of the trigeminal nerve (V2) provides only a minor contribution to sensorial innervation through the infraorbital nerve.[4]
Blood supply: The ophthalmic artery irrigates the extraocular muscles and the ocular globe. From its original trajectory entering the orbital space through the optic canal, blood vessel distribution is skewed towards the superior nasal quadrant. Consequently, this area is at high risk for local anesthetic infiltration and must be avoided.
Connective tissue: The Tenon capsule surrounds the ocular globe and extraocular muscles. This dense fibroblastic tissue covers the sclera and forms the episcleral space (Sub-Tenon space). It originates at the sclerocorneal limbus and extends toward the posterior pole of the globe to reach the optic nerve. Local anesthetic injected into Sub-Tenon space diffuses into the retrobulbar space, blocking the extraocular muscles and nerves supplying the globe in this space.
Imaging and contrast spread of retrobulbar block: One small case series comparing gadolinium distribution for the peribulbar vs. retrobulbar block observed that the spread of contrast medium was intense in the intraconal space, laterally greater than medially. Five minutes after injection, contrast surrounded the optic nerve sheath and was visible beyond the optic canal, around the internal carotid artery in its cavernous portion. Contrast remained visible even 90 minutes after injection. At that point, significant signal intensity was observed within the pterygopalatine fossa.[5]
Physiology applied to anesthesia for ocular surgery: Regional anesthesia techniques for ocular surgery can increase intraocular pressure (IOP). The volume injected in the intraconal or extraconal compartment generates external compression on the ocular globe, increasing the IOP by more than 20 mm Hg. Additionally, using digital pressure to improve local anesthetic spread, control bleeding, or reduce chemosis should be avoided. Digital pressure can increase the IOP to 400 mmHg[6] and has been associated with bleeding in the anterior chamber. A Honan balloon can be used with limited pressure between 20 mm Hg to 30 mm Hy if necessary.
Oculocardiac reflex: The Oculocardiac reflex is mediated by the parasympathetic nervous system. The traction of the extraocular muscles (most commonly the medial rectus muscle) produces direct pressure on the ocular globe, which generates bradycardia, auriculoventricular block, ventricular ectopia, and asystole. The afferent pathway involves activating stretching receptors localized in the extraocular muscles. These receptors transmit a signal through the short and long ciliary nerves to a division of the ophthalmic trigeminal nerve, the ciliary ganglion, and subsequently to the Gasser ganglion. Once the signal reaches the trigeminal ganglion, it is conducted to the sensory nucleus of the trigeminal nerve near the fourth ventricle. The internuncial nerve fibers then carry the signal to the motor nucleus of the vagus nerve. The efferent branch of the vagus nerve increases parasympathetic inputs to the heart conduction system.[7]
Indications
Broad indications exist for the use of retrobulbar blockade. Any intraocular surgery that requires anesthesia and akinesia for less than two hours can be an indication to do this block. The most common uses are cataract surgery, corneal transplant, keratoplasty, vitrectomy, tube shunt placement, enucleation or evisceration of the eyeball, and cyclodestructive procedures.
Contraindications
Absolute
- The patient refuses the retrobulbar block
- Local anesthetic allergy
- Local infection
- Nystagmus
Relative
- Open ocular trauma
- Intraorbital vascular tumors
- Previous scleral buckling
- Highly myopic eye (with an axial length greater than 26 mm) with or without myopic staphyloma
- Thyroid-associated orbitopathy
- Bleeding diathesis
- Anticoagulant use
- Strong orthopnea
- Poor control of psychiatric disorders or inability to cooperate with block performance
- Monocular status
Equipment
Sedation
- Intravenous access
- Midazolam 1 to 2 mg
- Fentanyl 50 to 100 mcg
- American Society of Anesthesiology (ASA) basic monitoring (noninvasive blood pressure, pulse oximetry, capnography, electrocardiography)
Retrobulbar Block
- Povidone-iodine 5% ophthalmic preparation
- Topical anesthetic drops (proparacaine hydrochloride 0.5%)
- Gauze package
- Syringe 5 mL to 10 mL
- Local anesthetic for infiltration (see technique)
- Sharp needle 23 to 25 gauge; length 30 to 38 mm
Peribulbar Block
- Sharp needle 25 to 27 gauge; length 15 to 25 mm
- Honan balloon
Sub-Tenon Block
- Sub-Tenon cannula 19 gauge; length 25 mm with a flat, curved tip. (The sub-Tenon block is out of the scope of this review)
Personnel
The retrobulbar block is considered an advanced regional anesthesia technique. Thus, it must be performed by trained providers, mostly anesthesiologists and ophthalmologists. It is helpful to perform with the assistance of a nurse trained in anesthesia to help administer sedation to the patient.
Preparation
Ophthalmological surgeries are common in an older population, with a higher incidence of comorbidities. Thus, a thorough preoperative assessment should be conducted, including a history of the present illness, a physical exam, and an airway assessment. It is essential to review prior test results, especially those that provide information about the length of the ocular globe and the patient's coagulation status (prothrombin time and activated partial thromboplastin time). Likewise, a current list of medications, including analgesics and anticoagulants, should be noted.
Though rates of complications during ophthalmological procedures are low, it is the responsibility of the anesthesiologist to holistically approach the explanation of potential risks and take necessary measures to minimize them. There is no consensus on the management of patients receiving anticoagulation therapy for ophthalmological surgery. However, most physicians follow the American Society of Regional Anesthesia (ASRA) 2018 guidelines for managing anticoagulation or antithrombotic therapy in patients undergoing peripheral regional and neuraxial blocks.[8] The procedure should be delivered in a setting with appropriate resuscitation and monitoring equipment (noninvasive blood pressure, pulse oximetry, capnography, electrocardiography).
Technique or Treatment
Selection of the Local Anesthetic
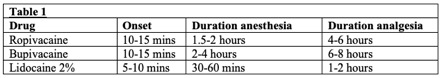
The selection of local anesthetic is based on drug onset and duration of action. Thus, it is common to find a mixture of short-acting and long-acting drugs (see Table 1). Lidocaine should not be used in concentrations higher than 2% to prevent muscular toxicity induced by local anesthetics.
Some physicians have used hyaluronidase as an adjuvant agent to decrease the onset time and facilitate local anesthetic spread through the tissue. Hyaluronidase may also decrease the incidence of postoperative strabismus by limiting local anesthetic myotoxicity. A safe dose is 50 IU per milliliter of local anesthetic. Epinephrine has been used to increase the duration of nerve blockade. However, the risk of vasospasm and subsequent retinal ischemia coupled with the increased availability of local anesthetics with long durations of action has limited its use in recent years.[9]
Retrobulbar Technique
- Two drops of local anesthetic can be instilled in the eye.
- Clean the lower and upper lids with an alcohol wipe or povidone-iodine.
- Localize the point of insertion. This can vary between different authors as the junction of 2/3 medial and 1/3 lateral along the lower orbital rim or the inferotemporal quadrant as laterally as possible.
- Ask the patient to fix the gaze in a neutral position. Avoid Atkinson gaze position upward and inward due to the high risk of optic nerve damage.
- With the non-dominant hand, place the index finger between the inferior orbital rim and the ocular globe. This maneuver elevates the globe to prevent direct trauma with the needle.
- Hold the syringe with your dominant hand. Stabilize your hand by placing the little finger and hypothenar eminence over the bones of the patient's cheeks.
- Insert the needle perpendicular to the skin and advance it parallel to the orbital floor. You might feel a first pop penetrating the orbital septum.
- After the first pop, advance the needle approximately 1 cm to 1.5 cm until it crosses the equator line of the ocular globe. Redirect the needle 30° to 45º in the superior and medial direction. Advance the needle 2.5 cm to 3.0 cm until a second pop is felt crossing the muscle cone where the needle is stopped.
- Aspirate to verify the needle tip is not in the intravascular space.
- Slowly inject 3 mL to 5 mL of local anesthetic, monitoring for any resistance to injection, excruciating pain, or significant rotation of the globe.
- Check ocular globe akinesia after 5 minutes of infiltration.
Peribulbar Technique
- Two drops of local anesthetic can be instilled in the eye.
- Clean the lower and upper lids with an alcohol wipe or povidone-iodine.
- Localize the point of insertion (junction of 2/3 medial and 1/3 lateral along the lower orbital rim or inferotemporal quadrant as laterally as possible).
- Ask the patient to fix the gaze in a neutral position. Avoid Atkinson gaze position upward and inward due to the high risk of optic nerve damage.
- With the non-dominant hand, place the index finger between the inferior orbital rim and the ocular globe. This maneuver elevates the globe to prevent direct trauma with the needle.
- Insert the needle perpendicular to the skin and advance it parallel to the orbital floor beyond the equator of the ocular globe. Infiltrate with 6 mL to 8 mL of local anesthetic.
This block requires a second infiltration, as the superior oblique muscle may not receive the effects of the block with just one injection.
- Several anatomical landmarks have been described for the second injection, including the medial canthus, tear caruncle, and medial third of the superior orbital rim (nasal superior site). However, there are some important considerations to review:
- The insertion of the needle through the nasal superior site must be avoided. At this level, the distance between the orbital roof and the ocular globe is reduced, increasing the risk of ocular globe perforation and superior oblique damage. Instead, a nasal inferior injection should be attempted.
- Insertion of the needle for a second puncture should be no deeper than 25 mm, as this increases the risk of injecting a local anesthetic into the retrobulbar compartment and subsequent optic nerve damage.[10]
- Infiltrate with 3 mL to 5 mL of local anesthetic.
- Honan balloon at a pressure of 20 mm Hg to 30 mm Hg can increase the spread of local anesthetic. This is also an alternative in the case of chemosis.
- Check ocular globe akinesia after 10 to 15 minutes of infiltration.
Complications
Complications of regional anesthesia techniques for eye surgery are rare, though they can put the sight or life of the patient at risk. The incidence of life-threatening events is low at 3.4 per 10,000 cases.[11] Most of these events are associated with a retrobulbar block. Studies have demonstrated that the use of a peribulbar technique with a needle length of less than 31 mm is rarely associated with adverse systemic effects.[12]
Retrobulbar hemorrhage: Retrobulbar hemorrhage has an incidence of 0.04% to 1.7% [13][14] for retrobulbar blockade and may originate from a venous or arterial source. This complication has been associated with the use of a needle larger than 38 mm.[15] As the needle advances, vascular structures are more compact, thus increasing the risk of vascular puncture. An arterial retrobulbar hemorrhage is characterized by a sudden onset of proptosis, decreased visual acuity, excruciating pain, and increases in intraocular pressure. It is considered a medical emergency and may require lateral canthotomy, cantholysis, or orbital decompression by an ophthalmologist. Retrobulbar hemorrhage with a venous source usually presents with a slower onset, characterized by chemosis and less effect on the intraocular pressure. This complication may improve with external digital pressure and administration of acetazolamide or mannitol.
Ocular globe injury: Ocular globe injury is also a rare complication, with incidence varying from 1 in 12,000 [16] retrobulbar blocks to 1 in 16,224 [17] for peribulbar blocks. The principal risk factor for this complication is an axial ocular length of more than 26 mm and the presence of staphyloma in the posterior pole of the eye. Duker et al described that up to 45% of ocular globe perforations are related to an increased axial length and that the retrobulbar block increases the risk of perforation 30-fold.[16] Symptoms of an ocular perforation vary but can be suspected when the patient experiences pain at the injection site and sudden vision loss. Upon physical examination, hypotonia of the ocular globe may be evident, along with poor red reflex and vitreous hemorrhage.[18] When a puncture of the ocular globe is suspected, it is helpful for the operator performing the block to ask the patient to move the eye. If movement is not observed, this may be because the tip of the needle is preventing it from moving.
Optic nerve damage: Optic nerve damage occurring with modern techniques of ophthalmologic nerve blocks is rare. The use of needles more than 31 mm in length has been associated with this complication. According to a study conducted by Unsold et al, the Atkinson gaze position “upward and inward” exposes the optic nerve, superior orbital vein, ophthalmic artery, and posterior pole of the eye to the tip of the needle, predisposing to puncture, perforation, and infiltration of local anesthetic of the nerve sheath.[19] This can lead to compression and ischemia of the nerve, requiring surgical decompression.
Extraocular muscle injury: The mechanism of extraocular muscle injury seems related to the direct injection of local anesthetic into the muscle, high volume of local anesthetic, and direct local anesthetic toxicity. Direct local anesthetic injection has been reported more commonly occurring in the inferior rectus, with strabismus, ptosis, and diplopia as principal signs. Ptosis can be a normal finding up to 24 hours after ocular surgery, though the persistence of other signs raises the suspicion of muscular or even nerve damage. Delayed recovery of more than six weeks may be related to permanent damage in up to 25% of cases.[10] The volume injected with the retrobulbar block should not exceed 5 mL in the intraconal compartment. Most authors suggest a safe dose is between 3 mL to 4 mL of local anesthetic. A high concentration of local anesthetic can cause direct toxicity, which is why concentrations of lidocaine higher than 2% are not recommended.[20]
Central spread of the local anesthetic and brain stem anesthesia: Fortunately, this life-threatening complication has a reported incidence as low as 0.3% to 0.8% of cases.[21][22] The exact mechanism of the central spread of local anesthetic and brain stem anesthesia is a matter of debate. Some authors conclude central spread is due to the direct puncture of the optic nerve sheath that communicates with the subarachnoid space.[23] Others suggest that puncture of a vascular structure and retrograde flow may place the local anesthetic in contact with encephalic structures. Symptoms of this complication usually start 10 to 15 minutes after local anesthetic injection and may initially manifest as tinnitus, amaurosis, slurred speech, tremors, agitation, and seizures. Within a few minutes, patients can present with respiratory depression and alterations in cardiac rhythm (bradycardia, asystole). Symptoms last approximately 2 to 3 hours, though, during this period, the patient will require intensive care unit observation and ventilatory support.
Clinical Significance
For many years, the retrobulbar block was considered the "gold standard" technique for ocular anesthesia. However, its use has declined since the introduction of newer techniques with similar efficacy in anesthesia and akinesia, yet lower rates of complications. The physician must recognize the potential usefulness of the retrobulbar block and its advantages in generating faster pain relief and akinesia over other techniques. Equally important is understanding the basic anatomy of the orbital space to facilitate comprehension of the risks associated with any regional anesthesia technique.
Enhancing Healthcare Team Outcomes
Though complications associated with this technique occur at a relatively low incidence, they can be sight or life-threatening, contributing to extended and expensive treatments and even medical support in the intensive care unit (ICU). While acknowledging the potential usefulness of this technique, physicians must recognize the associated complications and be prepared to react. The use of retrobulbar blockade must be discussed preoperatively with both the surgeon and patient to rule out potential risk factors, such as local anesthetic allergies, staphyloma, axial eye length more than 26 mm, presence of nystagmus, coagulopathy, or anticoagulant medications, and to improve patient safety and surgical outcomes.[24] [Level 2]