Introduction
The coronary arteries provide the main blood supply to the heart. The coronary arteries also supply the myocardium with oxygen to allow for the contraction of the heart and thus causing circulation of the blood throughout the body. Two main coronary arteries originate from the base of the aorta as it exits the left ventricle: the left and right coronary arteries. These arteries further branch into smaller arteries to supply specific parts of the heart like the atria, ventricles, SA, and AV nodes. It is important to realize that the paths these arteries take may vary slightly from person to person.
Structure and Function
The function of the arteries of the heart is to provide oxygen and nutrients to the myocardium to allow for contraction of the heart, which causes blood to circulate throughout the body. The arteries of the heart are also capable of autoregulation and can control the amount of blood flow supplying the heart according to its need. The coronary arteries receive the most blood flow during diastole because this is when the heart is relaxed, and they received the least blood flow during systole because this is when the myocardium contracts are decreasing the blood flow through the coronary arteries.
Blood Supply and Lymphatics
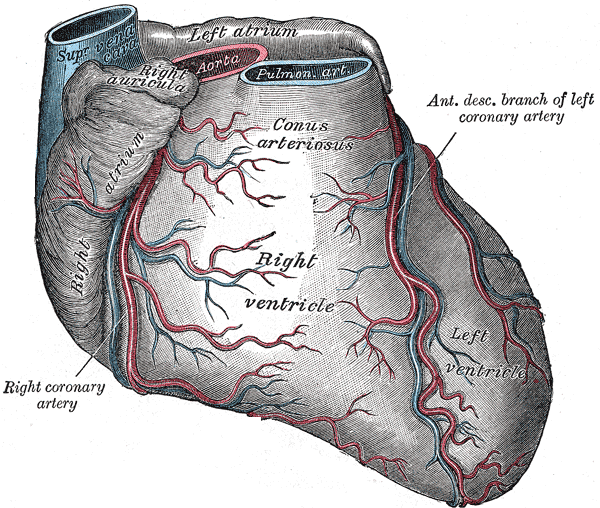
The coronary arteries split into two, main arterial branches from the base of the aorta. They are the left and right coronary arteries:
The left coronary artery (LCA) extends along the coronary sulcus and supplies the left portion of the heart. It further branches into the circumflex artery and the anterior interventricular artery (left anterior descending artery). The anterior interventricular artery further divides into septal branches and diagonal branches.
- The septal branches supply the anterior two-thirds of the interventricular septum and bundle of His.
- The diagonal branch supplies the anterolateral papillary muscle and the anterior and lateral portions of the left ventricular wall.
- The circumflex artery follows the coronary sulcus to the left portion of the heart and further divides into the left marginal artery and posterior left ventricular artery. The circumflex artery and its branches supply the posterolateral section left ventricle.
The right coronary artery (RCA) traces along the right coronary sulcus and provides blood flow to the anterior and diaphragmatic surfaces of the right atrium and ventricle; as well as the posterior two-thirds of the interventricular septum.
- The initial two branches that come off the RCA are the conus artery which provides blood flow to the infundibulum of the right ventricle where the pulmonary artery arises and the branch of the SA node which provides blood supply to the SA node.
- As the RCA travels along the coronary sulcus, it gives off the right marginal artery which travels along the acute margin (anteroinferior border) of the heart. The right marginal artery is used in angioplasty to distinguish the inferior border of the heart, and it provides blood flow to the right ventricle.
- As the RCA travels to the posterior portion of the heart, the posterior interventricular artery (posterior descending artery) and right posterolateral artery at the crux cordis branch off. The crux cordis is used as a landmark in angiography.
- Both the posterior descending artery (PDA) and the right posterolateral artery are terminal branches. The posterior descending artery (PDA) gives off septal branches that supply the posterior one-third of the interventricular septum. The right posterolateral arteries may provide part of the left posterior atrium and ventricles.
- Eventually, at the end of the RCA course, it gives off the branch of the AV node. The branch of the AV node branches off at the diaphragmatic surface and supplies the AV node.
Anastomosis occurs in a few places of the heart even though the coronary arteries are considered end arteries.
- One anastomosis is between the branches of the LAD from the LCA and the branches of the PDA from the RCA.
- Another one is between the RCA and the left circumflex artery in the coronary sulcus.
- A third anastomosis occurs with the septal branches of both arteries at the interventricular septum.
Coronary Venous Anatomy
Just like the coronary arteries, there are coronary veins that drain the myocardium of deoxygenated blood. In general, there is twice the number of coronary veins as arteries, and the flow occurs during both systole and diastole.
The coronary veins are organized into two groups: greater and smaller cardiac veins. The greater cardiac veins consist of the coronary sinus, atrial veins, anterior cardiac veins, and veins draining the septum. The greater cardiac veins account for 95% of all venous drainage from the heart. The smaller cardiac veins also known as the thebesian veins are luminal vessels and drain directly into the respective cardiac chambers.
All the venous blood from the heart arrives at the coronary sinus which is located in the atrioventricular groove. The coronary sinus is the biggest cardiac vein, and it empties directly into the right atrium at the conjunction of the coronary and the interventricular grooves. The coronary sinus does have a small valve-like structure.
Nerves
The medulla provides sympathetic and parasympathetic innervation to the heart and coronary arteries. The sympathetic innervation is via the cardiac fibers from the superior, middle, and inferior cervical ganglion. Sympathetic innervation causes vasodilation of the coronary arteries. The parasympathetic innervation is via the vagus nerve. The vagus nerve will constrict the coronary arteries.
Physiologic Variants
There are many anatomic variations in the blood supply of the heart. One of the biggest distinctions is determining whether the heart is RCA dominant, LCA dominant, or codominant. The dominance of the heart depends on where the PDA is derived from.
- If the PDA is a branch of the RCA, then it is said to be RCA dominant, this occurs in at least 70% of cases.[1]
- If the PDA branch comes off the LCA, the patient is said to be LCA dominant; this occurs in about 10% of cases.
- The patient may also be codominant, meaning the PDA is supplied by both right and left coronary arteries, this occurs in 20% of cases. This is significant because if the LCA and obstruction supply the PDA, the LCA can be more damaging and critical
Important congenital coronary artery anomalies exist. Children born with an anomalous left coronary from the pulmonary artery (ALCAPA) present with congestive heart failure around 4-6 months of age. An anomalous left coronary artery from the right sinus coursing between the pulmonary artery and the aorta is associated with sudden death during exercise.[2][3]
Coronary artery disease is uncommon in young people except in rare cases of homozygous familial hypercholesterolemia.[4]
Surgical Considerations
Percutaneous coronary intervention (PCI) are non-surgical procedures that are recommended once a patient is diagnosed with unstable angina, non-ST elevated myocardial infarction, or ST-elevated myocardial infarction. The goal of this procedure is to relieve the narrowing or occlusion of the coronary artery. PCI includes procedures such as angiography, angioplasty, and stent placement and should be done within 90 minutes of the patient's arrival to the emergency department. These procedures are done in the cath lab to help visualize the obstruction and revascularize the heart. Angioplasty allows the visualization of the arteries and localizing of the narrowing of the coronary artery. After narrowing is identified a balloon angioplasty can be done where a balloon is inflated causing expansion of the narrowed artery and improving blood flow. A stent is a mesh tube that can be placed to keep the coronary artery open.[5]
Clinical Significance
A myocardial infarction occurs when there is a narrowing or occlusion of a coronary artery due to atherosclerosis (plaque buildup due to cholesterol). In an infarction blood supply is insufficient to the contracting myocardium and oxygen supply does not meet oxygen demand causing cell death. This causes an ST-segment elevation on an ECG due to abnormal conduction through the heart.
Coronary arteries are end arteries, and this means there is only one source of blood supply to the myocardium increasing the risk of endocardial damage due to narrowing.
Considering that the function of the arteries is to supply the heart with oxygen, it is important to know which artery supplies which portion of them in order to be able to read an electrocardiogram (EKG). Knowing which leads in an ECG correspond to specific arteries helps localize the location of the obstruction which can produce predictable patterns.[6][7]
- An inferior infarction shows ST elevation in leads II, III, and aVF and the vessel involved is the RCA.[8]
- A posterior infarction shows ST depression in leads V1, V2, V3, and large R wave, and the vessels involved are proximal RCA and left circumflex.
- An anterior infarction shows an ST elevation in leads V1, V2, V3, and V4, and the vessel involved is the LAD.
- Lateral infarction shows ST elevation in leads I, AVL, V5, and V6, and the vessel included is the left circumflex.
- Right ventricular infarction shows elevations in leads II, III, and V1, and the vessel included is the proximal RCA.
Other Issues
Anomalous coronary arteries can be a diagnostic challenge. They may occur either singly or in combination with other congenital heart disorders. The incidence of anomalous coronary vessels has been reported to be about 0.1% to 0.3% in necropsy reports. Although rare, they can often present with hemodynamic abnormalities. Many coronary anomalies are first identified on an angiogram because of their anomalous course.
Type of Coronary Anomalies
High Takeoff: where the origin of the LCA or RCA is above the usual anatomical location. These anomalies may present with difficulty in cannulation during angiography.
Multiple ostia where the RCA and the conus branch may arise separately, or the LAD and left circumflex may arise with no left common coronary artery.
Single Coronary Artery: when there is only one coronary artery arising from the aortic trunk. It may be the RCA or the LAD. If the single coronary passes between the aorta and pulmonary artery, it can be compressed and present with sudden death.
Anomalous origin of the coronary artery from the pulmonary artery is the most serious congenital coronary artery anomaly. Most infants are symptomatic at birth. In the most common type, the left common coronary arises from the pulmonary artery with the RCA arising normally. These patients need some procedure to convert it into a dual coronary artery system. The bypass can be conducted with a saphenous vein graft or internal mammary, but the small size of the coronary is a major limiting factor. Rarely, this can present in adolescents and adults.[9][2][10]