Introduction
The skeletal muscles of the hand are responsible for the movement of the hand and fingers.[1] These muscles subdivide into two groups: the extrinsic and intrinsic muscles.[2][3] The extrinsic muscle group is called so because the muscle belly originates in the forearm.[2][4] The intrinsic muscle groups consist of smaller muscles solely located within the various hand osseofascial compartments within the anatomic confines of the wrist (proximally) and phalanges (distally).[3][5][6] The intrinsics are important for various hand functions, such as pinch and grip strength.[7][8] An understanding of the intrinsic hand muscle groups is crucial, as denervation and loss of function may lead to pronounced deficits in hand function.[2][7] This article presents an overview of the intrinsic muscles of the hand and discusses its structure and function, embryology, neurovasculature, muscle groups, physiologic variants, surgical considerations, and clinical significance.
Structure and Function
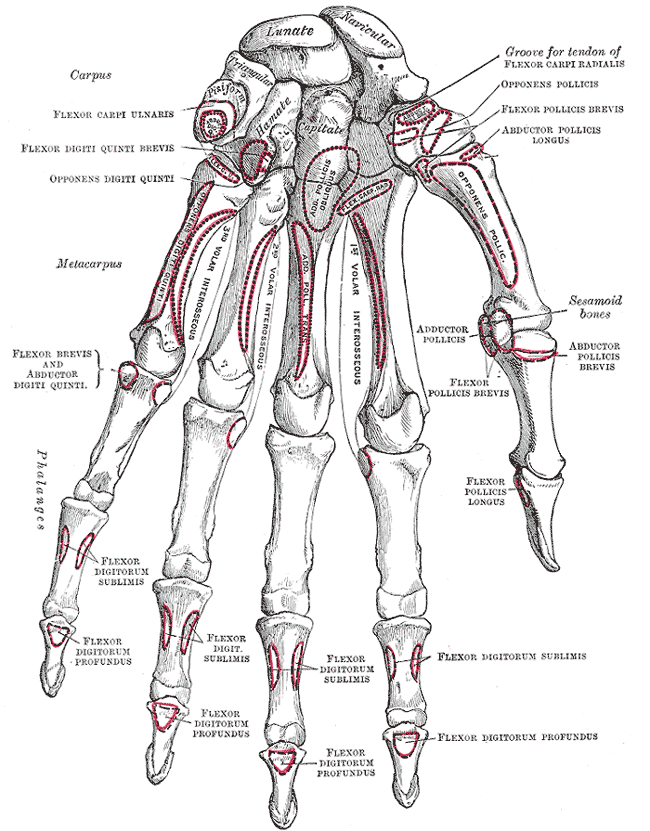
Four muscle groups comprise the intrinsic hand. These are the thenar, hypothenar, interossei and the lumbrical muscles.[2][3][9][1] The thenar muscle, or thenar eminence, is a collection of three muscles at the fleshy base of the thumb (first digit) on the palmar aspect that acts to exert movement about the thumb. The thenar muscles include abductor pollicis brevis (APB), flexor pollicis brevis (FBB) and opponens pollicis (OPP).[10] It is important to note that thumb adduction is via the adductor pollicis muscle and is not part of the thenar eminence.[11][3] The hypothenar muscle is a collection of three muscles at the fleshy base of the pinky finger (fifth digit) on the palmar aspect that acts to exert movement about the pinky. The hypothenar muscles include abductor digiti minimi (ADM), flexor digiti minimi brevis (FDMB) and opponens digiti minimi (ODM).[2] The interossei themselves are comprised of four dorsal (DI) and three palmar (PI) interossei muscles. One commonly used memory tool to remember the function of the interossei is the mnemonic, “DAB and PAD.”[12] The “D” in DAB stands for DI, which act to abduct the digits, while the “P” in PAD stands for PI, which acts to the adduct the digits.[2][9][12] The lumbrical muscles themselves are composed of four muscles that all act to flex their respective metacarpophalangeal (MCP) joint and extend the proximal interphalangeal (PIP) and distal interphalangeal (DIP) joints.[1] Further discussion on the origin and insertion of each muscle group will be expounded further below in “Muscles.”
Embryology
Understanding the genetics of limb development is an important aspect of both medicine and surgery as signaling errors in embryological development may lead to congenital deformities. Although the genetics are still not fully understood, recent advancements in the study of invertebrates and vertebrates have determined the key steps involved in the complex interactions of limb development.[13][14] Limb formation follows the formation of the three germ layers (ectoderm, mesoderm, and endoderm) during the gastrulation phase of early embryogenesis. It begins when undifferentiated cells within the mesoderm, called mesenchyme, secrete and respond to biochemical signals to develop specific structures in distinct spatial axes. The resulting interaction of biochemical signals between the ectoderm and underlying mesoderm cause the mesenchymal cells in the periphery of the embryo, termed lateral plate mesoderm, to proliferate and move outwards, forming a limb bud.[14][15] Here, we will briefly review the macroscopic and microscopic development of the limb bud that ultimately forms the upper extremity and hand. Similarities exist in the embryological development of the lower extremity but will not be a topic for this paper.
Macroscopic embryological development of the upper extremity and hand
The limb bud consists of undifferentiated mesodermal cells covered by overlying ectoderm. Two important mesodermal tissues are the lateral plate mesoderm, that yields cartilage and bone, and the somites, which yield skeletal muscle.[9] The upper extremity of the human embryo is first visualized by during week 4 (approximately day 26) as a lateral projection, or limb bud. Week 5 (approximately day 36), the arm buds enlarge and appear paddle-like, nerves and vasculature appear and enter the upper extremity in a proximodistal fashion, chondrification occurs and muscles develop. Muscles develop as myogenic progenitor cells divide into superficial and deep layers, with the deep layers contributing to the intrinsic muscles of the hand.[1][16] During weeks 6 to 7, muscle formation and skeletal elongation continues in a proximodistal fashion, and the process of ossification begins. In week 8, the digits of the hand become visible following apoptosis of the interdigital web spaces. At week 9, all upper extremity muscles develop except for the intrinsic hand muscles, but by week 12, all upper extremity muscles including muscles of the intrinsic hand are present.[16]
Microscopic embryological development of the upper extremity and hand
In the limb, not only is it important for the development of the macroscopic structures (muscle, bone, and connective tissue) but it is critical for limb identity and limb outgrowth to occur in a stepwise order.[3][14] Genes and protein factors control the microscopic processes that develop the upper extremity and hand in a process called pattern formation, or patterning.[14] Patterning of the limb bud begins with upregulation of the Hox gene family, a group of genes located in the lateral plate mesoderm that dictate where limb buds will form by initiating downstream signals. These signals create three centers responsible for the growth of the developing limb in three spatial axes: proximal-distal (PD), anterior-posterior (AP) and dorsal-ventral (DV).[14][17]
When the limb bud first appears on week 4 (approximately day 26), activation of mesenchymal cells of lateral plate mesoderm cause PD growth due to the development the apical ectodermal ridge (AER), a thickened area of ectoderm overlying the mesoderm. The process by which this occurs takes place when Hox gene expression initiates the T-box family, Tbx5 and Tbx4, proteins that program limb identity and stimulate ligands called fibroblast growth factors (FGF). T-box proteins initiate FGF10 expression in the proliferating mesoderm to produce the AER, and the AER produces its own FGFs to maintain the growth of the underlying mesoderm. In regards to limb identity, Tbx5 is responsible for the programming upper extremity structures, while Tbx4 is responsible for the lower extremity structures. The importance of the AER and FGFs in the developing limb is shown in experiments that result in severely shortened limbs with the removal of AER or FGFs are absent.[14][17]
The second axis, AP, is controlled the zone of polarizing activity (ZPA), a collection of cells at the posterior border of the limb bud.[14] The zone of polarizing activity is initiated by the Hox gene family and retinoic acid to express the sonic hedgehog (SHH) protein, which is critical for correct digit identity in the hand. The importance of the zone of polarizing activity and sonic hedgehog protein in the developing limb becomes obvious in experiments that duplicate ZPA or remove SHH. With duplication of ZPA in the limb bud mirror-image digits form, and when SHH proteins are removed digits fail to form.[15]
The third axis, DV, is controlled by Wnt7a, a protein expressed in the overlying ectoderm of the limb bud. Wnt7a is involved in interactions between two other factors that help the limb develop its correct dorsal structures.[14][17] Experiments that result in deformed dorsal hand structures with the removal of Wnt7a have shown the importance of Wnt7a in the developing limb.[18]
Blood Supply and Lymphatics
Blood supply to the intrinsic hand muscles comes from the ulnar and radial arteries and their anastomotic branches and collateral circulation. The ulnar and radial arteries cross the wrist to enter the hand and send vessels deep and superficially, forming two anastomoses called the superficial and deep palmar arches. The ulnar artery contributes to the majority blood supply of the superficial palmar arch, while the radial artery contributes to the majority of the deep palmar arch. Arising from the superficial palmar arch, are distal branches called the common and proper palmar digital arteries.[9][1][19]
The thenar muscle is supplied primarily by the superficial palmar arch. The hypothenar muscle is supplied primarily by the ulnar artery.[10] Blood supply to the interossei (DI and PI) muscles all have the same primary source except for the first DI. Blood supply to the first DI is by the first dorsal metacarpal artery, a direct branch from the radial artery. However, the second, third and fourth DI muscles receive supply from their respective dorsal metacarpal arteries, but each arises from the dorsal carpal arch. Blood supply to the PI comes from the palmar metacarpal arteries, branches from the deep palmar arch.[9][12] The lumbricals are supplied primarily from the superficial palmar arch but also receive supply from the deep palmar arch, dorsal digital arteries, and common palmar digital arteries.[1]
Lymphatic drainage of the upper limb and hand drain into the superficial and deep lymphatic systems. The superficial system drains the skin of the palm and dorsal hand via the lymphatic plexuses along the cephalic and basilic veins towards the axillary and cubital lymph nodes. The deep system drains the skeletal muscle of the hand via the lymphatic plexuses along the deep veins and terminates in the humeral lymph nodes.[9][1]
Nerves
Nerves of the intrinsic hand arise from the brachial plexus, a network of nerves from ventral rami between the C5 to T1 nerve roots. The nerves of the brachial plexus that supply muscles of the intrinsic hand include the median and ulnar nerve. The median nerve is composed of C5 to C8 nerve roots and enters the hand through the carpal tunnel, where it divides into a recurrent motor branch and cutaneous branch. The ulnar nerve is composed of the C8 to T1 nerve roots and enters the hand through the Guyon canal, where it divides into a superficial and deep branch.[20][21][22]
The thenar muscle group receives innervation from the recurrent motor branch of the median nerve, a branch of the median nerve.[10] The adductor pollicis muscle receives innervation from the deep branch of the ulnar nerve.[3] The hypothenar muscle group receives innervation from the deep branch of the ulnar nerve, a terminal motor branch of the ulnar nerve.[2] Both interossei (DI and PI) receive innervation from the deep branch of the ulnar nerve.[9] The first and second lumbricals receive innervation by the median nerve, whereas, the third and fourth lumbricals receive innervation by the deep branch of the ulnar nerve.[1]
Muscles
Intrinsic Muscles of the Hand
Thenar Muscles:
Abductor pollicis brevis (APB)
- Function: Abduction of the first digit (thumb)
- Origin: Flexor retinaculum and the tubercle of the scaphoid
- Insertion: Lateral aspect of the proximal phalanx of the thumb
- Nerve: Recurrent motor branch of the median nerve
Flexor pollicis brevis (FBB)
- Function: Flexion of the thumb
- Origin: Flexor retinaculum and the tubercle of the trapezium
- Insertion: Lateral aspect of the proximal phalanx of the thumb
- Nerve: Recurrent motor branch of the median nerve
Opponens pollicis (OPP)
- Function: Opposition of the thumb
- Origin: Flexor retinaculum and the tubercle of the trapezium
- Insertion: Lateral aspect of the thumb
- Nerve: Recurrent motor branch of the median nerve
Intrinsic Thumb Adduction Component:
Adductor pollicis
- Function: Adduction of the thumb
- Origin: 2nd and 3rd metacarpal, and the capitate
- Insertion: Proximal phalanx and extensor expansion of the thumb
- Nerve: Deep branch of the ulnar nerve
Hypothenar Muscles:
Abductor digiti minimi (ADM)
- Function: Abduction of the 5th digit (pinky)
- Origin: The pisiform
- Insertion: Medial aspect of the proximal phalanx of the 5th digit
- Nerve: Deep branch of the ulnar nerve
Flexor digiti minimi brevis (FDMB)
- Function: Flexion of the pinky
- Origin: Flexor retinaculum and the hamate
- Insertion: Medial aspect of the proximal phalanx of the pinky
- Nerve: Deep branch of the ulnar nerve
Opponens digiti minimi (ODM)
- Function: Opposition of the pinky
- Origin: Flexor retinaculum of the hamate
- Insertion: Medial aspect of the 5th metacarpal
- Nerve: Deep branch of the ulnar nerve
Interossei Muscles:
Dorsal Interossei (DI)
- Function: Abduction of the 2nd, 3rd, and 4th digits
- Origin: Metacarpals
- Insertion: Extensor hood and proximal phalanges of the 2nd, 3rd, and 4th digits
- Nerve: Deep branch of the ulnar nerve
Palmar Interossei (PI)
- Function: Adduction of the 2nd, 3rd, and 4th digits
- Origin: Palmar aspect of the 2nd, 4th, and 5th metacarpals
- Insertion: Extensor hood and proximal phalanges of the 2nd, 4th, and 5th digits
- Nerve: Deep branch of the ulnar nerve
Lumbricals[3][23]:
- Function: Flexion of the MCP joints with the extension of the PIP and DIP joints
- Origin: Tendons of the flexor digitorum profundus
- Insertion: Extensor hood of the 2nd, 3rd, 4th, and 5th digits
- Nerve: Median nerve for the 1st and 2nd lumbricals, whereas, the 3rd and 4th lumbricals receive innervation by the deep branch of the ulnar nerve
Physiologic Variants
Physiologic variants of the upper extremity may manifest within and around the intrinsic hand muscles. Anomalous muscles and neurovasculature may create compressive neuropathies of the hand or distorted anatomical landmarks. Although they exist as a minority, it is important to distinguish normal anatomy from clinically relevant and asymptomatic variants to avoid misdiagnoses or overdiagnoses.[24] Some of the common variants pertaining to the intrinsic hand are discussed below.
Variants of the lumbrical muscles have been the subject of much study.[24] Normal physiology has the lumbricals arising from the flexor digitorum tendon at a level distal to the carpal tunnel. However, in 22% of individuals, the lumbricals will arise within the carpal tunnel. The pathological concern is if this variant muscle were to hypertrophy in the confined space of the carpal tunnel, it might lead to carpal tunnel syndrome.[25]
Studies have also shown variants of neurovasculature within the hand.[24] In one study analyzing 526 elective carpal tunnel releases, anatomic variants were present in 6% of cases. Concerning the median nerve, an important nerve for the intrinsic muscles, there was variability shown in the alignment of the median nerve in the carpal tunnel, its shape and its relationship to the flexor tendons. In regards to the ulnar nerve, another important nerve for intrinsic muscles, an aberrant branch was found crossing the carpal tunnel.[26][27] The concern for neurovasculature variants arises when anatomical landmarks during surgical procedures become distorted.
Surgical Considerations
Surgical considerations should consider physiologic variants. Because of the variety of anatomic changes that may distort landmarks during hand imaging and surgery, it is important to consider anomalous muscles and nerves.[27][25][26]
The creation of muscle flaps, utilizing the intrinsic hand muscles, have been described in the literature to treat carpal tunnel syndrome and other nerve palsies.[1][28] In patients presenting with an exposed or compressed median nerve, the first and second lumbrical muscles have been used as flaps to cover the nerve to buffer it from the surrounding environment.[1] Another study also pointed to the use of thenar muscle flaps, in addition to lumbricals, for the treatment of painful neuromas.[28]
Tendon transfers for the treatment of median and ulnar nerve palsies leading to deficits in muscles of the intrinsic hand are a well-covered topic in the literature.[8][22][29] The primary goals of tendon transfer surgery for ulnar nerve palsy are to restore pinch and grip strength and the correction of clawing. Pinch strength is obtained through the action of the first DI and adductor pollicis muscle, both of which receive innervation from the ulnar nerve.[8] Transfers utilizing wrist and finger extensors, finger flexors and the brachioradialis have been shown to restore pinch strength without leaving a functional deficit when harvested. Correction of ulnar clawing have been successful by harvesting and reinserting tendons to limit the action of MCP hyperextension. The primary goal of tendon transfer surgery for median nerve palsy is to restore the loss of thumb opposition. Because thumb opposition is a complex activity that requires palmar abduction, pronation, and thumb flexion, a tendon transfer to the APB insertion best approximates the action of thumb opposition; however, many more surgical techniques exist.[22][8]
Clinical Significance
When the hand is at rest, there is an equilibrium in the forces between the intrinsic and extrinsic muscles of the hand, especially from lumbricals and the interossei.[30] As stated in the “Structure and Function” and “Muscles” section, we know the lumbricals are responsible for flexion of the MCP and extension of the DIP and PIP joints; therefore, when there is loss of nerve innervation to the lumbricals, the equilibrium is also lost, and forces from the extrinsic muscles predominate. [30][22] Furthermore, current literature now points to the interossei as muscles that significantly contribute to the function of the lumbricals.[7][12][30] Thus, the remaining extrinsic muscles highlight the loss of the intrinsic muscles, causing extension of the MCP and flexion of the DIP and PIP joints, distorting the hand. Compressive, traumatic or systemic neuropathies causing damage to the median and ulnar nerves are common and may lead to distortions of the hand. Common hand distortions include ulnar clawing, Pope’s hand of benediction and Klumpke palsy.[30][31][32] It is important for the astute physician to recognize such clinical presentations, as any untreated nerve palsy may lead to long-standing dysfunction that negatively impacts a patient’s activities of daily life.[12][22]
Ulnar clawing and Pope’s hand of benediction present similar but arise from different nerve lesions. Ulnar clawing results from a distal ulnar nerve lesion, at the level of the wrist, yielding paralysis of the interossei in the presence of functioning extrinsic muscles. Recalling that the ulnar nerve innervates all the interossei and the third and fourth lumbricals, if the equilibrium is lost, the opposing forces exaggerate MCP flexion and PIP and DIP extension, which impacts a patient’s ability to cup their hand around objects.[22][30][32] The Pope’s hand of benediction presents similarly but arises from a proximal median nerve injury, at the level of the elbow, and does not affect the intrinsic hand muscles. Proximal median nerve injury results in paralysis of the extrinsic flexors of the hand while sparing the ulnar half of the extrinsic flexors. Thus, when attempting to flex the hand, there is partial flexion of digits four and five while the other digits remain extended. In contrast to ulnar clawing, where the hand deformation occurs at rest, the Pope’s hand of benediction occurs only when a patient attempts to make a fist.[30][32]
Klumpke palsy, or total hand claw, is a neuropathy involving the lower trunk of the brachial plexus (C8 to T1). Deficits to the lower brachial plexus lead to loss of all intrinsic hand muscles. Loss of lumbricals and interossei result in an extension of MCP joints and flexion of DIP and PIP joints. Loss of thenar and hypothenar muscles result in palmar atrophy and weakness in thumb and pinky finger abduction, flexion and opposition. The most common mechanism of injury is hyper-abduction of the upper extremities. Two populations in which this occurs is: in the neonate with upward traction of the arms during delivery, and in adults with traumatic upward traction of the arms.[31]
Other Issues
A comprehensive analysis of hand function will include overall visual inspection, assessment of the strength, coordination, and speed of hand movements. By combining a thorough physical exam with knowledge of the intrinsic hand muscles, an astute physician should be able to comfortably recognize and workup patients presenting with distortions of normal hand anatomy.[33][30]