Continuing Education Activity
Torticollis, also known as twisted or wry neck, manifests as the contraction or contracture of neck muscles, resulting in head tilting, chin rotation, and flexion. While torticollis is not a standalone diagnosis, it is a symptom of various underlying conditions, which can be congenital or acquired at any age. The congenital form typically appears within weeks after birth and is often isolated. Diagnosis hinges on clinical examination findings, with physical therapy as the primary treatment approach. However, surgical intervention may be warranted if conservative measures fail to produce desired outcomes or for cosmetic purposes. In this context, a comprehensive understanding of torticollis evaluation and management and collaboration among healthcare team members is crucial to optimize patient outcomes and ensure well-coordinated care.
This activity provides a comprehensive review of the evaluation and management of torticollis, emphasizing the importance of an interprofessional approach. Participants gain insight into the assessment techniques and treatment modalities employed for individuals with torticollis. Additionally, this activity underscores the significance of collaboration among healthcare team members, including physicians, physical therapists, nurses, and caregivers, to deliver well-coordinated care and optimize outcomes for affected patients.
Objectives:
Identify the clinical signs and symptoms of congenital torticollis during routine pediatric assessments.
Assess the effectiveness of treatment interventions by regularly evaluating neck range of motion and motor development.
Collaborate with interprofessional team members, including physical therapists, pediatricians, and nurses, to provide comprehensive care for patients with torticollis.
Outline interprofessional team strategies for improving care coordination and communication to advance torticollis and improve outcomes.
Introduction
The clinical term torticollis originates from 2 Latin words: tortum and collum, meaning twisted and neck, respectively. Torticollis refers to a contracture or fibrosis of the sternocleidomastoid muscle on 1 side, resulting in an ipsilateral inclination and contralateral rotation of the face and chin.[1][2][3] Usually, torticollis arises as a manifestation of various underlying conditions, and it can be present at birth or develop at any age.
Congenital torticollis typically manifests in the neonatal period or shortly after birth.[4] Presentation timing varies based on severity, with the postural type appearing earlier. Diagnosis is primarily established through physical examination. The global incidence of congenital torticollis varies between 0.3% and 1.9%, with some studies suggesting a ratio of 1 per 250 newborns, making it the third most common congenital orthopedic anomaly following congenital hip dysplasia and calcaneovalgus feet. Congenital torticollis may be accompanied by congenital hip dysplasia up to 20% of the time.[5] There is a male-to-female predominance with a 3 to 2 ratio.
Congenital torticollis is present at birth or within the first weeks of life and requires differentiation from other forms of acquired torticollis. Acquired torticollis can develop at any age secondary to congenital skeletal anomalies, trauma, infections, inflammation of adjacent structures, tumors, or ocular and neurological dystonias.[6]
Physical therapy is the cornerstone of torticollis treatment, whether congenital or acquired. Surgical intervention becomes necessary when physical therapy fails to provide results or for cosmetic reasons.[7][5][8][9]
Etiology
Several theories exist regarding the etiology of congenital torticollis, including ischemia, trauma during childbirth, and intrauterine malposition (pelvic position).[10] However, none of these theories have been proven, and the exact cause remains unknown.
The leading cause is believed to be intrauterine deformation, which often occurs in situations associated with limited intrauterine space, such as in first pregnancies, decreased amniotic fluid volume, or uterine compression syndrome. Other causes of congenital torticollis include positional deformation, vertebral anomalies, unilateral atlantooccipital fusion, Klippel-Feil syndrome, unilateral absence of sternocleidomastoid muscle, and pterygium colli.[11] The most common form of torticollis in childhood is congenital muscular torticollis, characterized by sternocleidomastoid muscle abnormalities.
The neck muscles comprise a complex system, distinguished into 2 levels: a superficial level consisting of long neck muscles and a deep level consisting of paravertebral muscles. Among these, the sternocleidomastoid muscle is the most targeted superficial muscle in the anterior region of the neck, forming a visible and palpable mass. Its insertions on the sternum (sternum furcula), clavicle (two-thirds medial), occipital region (two-thirds side of the neckline), and mastoid apophysis, with its fibers oriented obliquely upward and outward direction. This muscle facilitates contralateral rotation, ipsilateral inclination, and flexion of the head, resulting in the head and neck tilting towards the side of the active muscle and rotation of the head to the opposite side.
Congenital torticollis is commonly diagnosed during the neonatal period or infancy.[8] In a prospective cohort study involving 155 infants under 12 months with congenital muscular torticollis, it was found that 30% of patients had gastroesophageal reflux disease (GERD). However, there were no differences in the demographic or clinical characteristics between torticollis patients with and without GERD.[12]
Epidemiology
The global incidence of congenital torticollis ranges between 0.3% and 1.9%, with some studies indicating a ratio of 1 in 250 newborns, ranking it as the third most common congenital orthopedic anomaly. There is a preponderance in males and among first pregnancies.[3][4]
The incidence of congenital torticollis has been reported to be 2% in traumatic deliveries and 0.3% in nontraumatic deliveries.[13] Additional data indicate an incidence of 53% in children born to primiparous mothers, particularly those with a history of traumatic childbirth. Typically, congenital torticollis is identified in neonates around 2 to 3 weeks of age and can persist until 1 year. It commonly manifests unilaterally but rarely can be bilateral. There may be a visible, palpable swelling known as a sternomastoid tumor in up to 50% of cases.[14]
Congenital muscular torticollis is categorized into 3 types:
- Postural (20%): The infant exhibits a postural preference without muscle tightness or restriction to the passive range of motion.
- Muscular (30%): Characterized by tightness of the sternocleidomastoid muscle and limitation of passive range of motion.
- Sternocleidomastoid mass (50%): Presents with thickening of the sternocleidomastoid muscle and restricted passive range of motion.
There is a noted correlation between congenital muscular torticollis and developmental dysplasia of the hip. Therefore, in infants diagnosed with congenital muscular torticollis, conducting physical examinations and imaging to screen for and identify developmental dysplasia of the hip can result in early diagnosis and treatment, increasing the likelihood of successful nonoperative management.[15] However, congenital muscular torticollis has not been recognized as a risk factor when treatment for developmental dysplasia of the hip fails.
Pathophysiology
In congenital muscular torticollis, where a palpable mass is present in the sternocleidomastoid muscle, it primarily consists of fibrous tissue. This mass usually disappears during infancy, being replaced by a fibrous band. Muscle biopsies and MRI studies of the mass have suggested the presence of muscle injury, likely resulting from compression and stretching of the muscle.
Venous neck compression during childbirth could have contributed to decreased blood supply and subsequent compartment syndrome. Histological studies of material collected at delivery revealed edema, muscle fiber degeneration, and fibrosis, supporting the presence of compartment syndrome.[3][11]
In a retrospective study involving 2599 children diagnosed with congenital muscular torticollis, ultrasound examination of the sternocleidomastoid muscle identified 3 types: local mass, uniform thickening, and atrophy. Among these, children with the local mass type of congenital muscular torticollis demonstrated high success rates with nonoperative management.[16]
A retrospective study examining the sternocleidomastoid muscle, upper trapezial muscle, and cross-sectional area of the accessory nerve identified thicker structures in patients with congenital muscular torticollis. The study postulated that the size of the sternocleidomastoid muscle might influence the thickness of the upper trapezius muscle via the accessory nerve in congenital muscular torticollis patients.[17]
Histopathology
The basic tissue abnormality observed in congenital torticollis is endomysial fibrosis, characterized by collagen deposition and the accumulation of fibroblasts around the muscle fibers, resulting in muscle atrophy.[14][18] In addition, this fibrotic process can lead to decreased flexibility and range of motion in affected muscles, contributing to the characteristic symptoms of torticollis.
Gross examination reveals no hemorrhages or necrosis. Microscopic examination reveals a diffuse proliferation of uniform fibroblasts and myofibroblasts, degenerative skeletal muscle fiber, and scar-like collagen. Biopsied tissue stains positive for vimentin and actin. Pathological study with hematoxylin and eosin staining shows apparent interstitial fibrosis around residual myofibers in the lesion specimens.[19]
History and Physical
Parents often notice the infant's tilted head and raise concerns. The evaluation of a newborn with congenital torticollis should include a comprehensive clinical history, including any history of oligohydramnios, traumatic delivery, or pelvic presentation, and a thorough physical examination, paying particular attention to palpation of the sternocleidomastoid muscle. Clinical signs of congenital torticollis include:
- Fibrosis or shortening of the sternocleidomastoid muscle.
- A lateral tilt of the head in the frontal plane and contralateral rotation in the transverse plane with notable limitation of the active and passive cervical range of motion and a fixed postural stiff neck resulting from a restricted or fixed muscle.
- A painless palpable mass or tumor over the side of the neck along the sternocleidomastoid muscle; these are evident in neonates aged 2 to 3 weeks. The swelling is firm, movable under the skin, and soft. If the mass is small or missed in the neonatal period, the infant's head is usually tilted and flexed to the side of the lesion. Diagnostic confirmation is found in 50% of cases within 2 months. The nodule may grow for 2 months until it reaches the approximate size of an almond before it begins to regress; it may disappear entirely until the eighth month of life.[20]
- Modification of cranial morphology (related to the presence of plagiocephaly) by flattening the parieto-occipital zone and anteriorization of the contralateral ear to the affected sternocleidomastoid muscle with frontal flattening homolateral to the affected sternocleidomastoid muscle.[5]
- Compensatory postures of the cervical, thoracic, trunk, extremities, shoulder elevation, or trunk inclination to the affected side.
Due to unilateral muscle shortening, children with congenital torticollis often prefer to sleep in the prone position, with the affected side down. This position can exert asymmetrical pressure on the skull and developing facial bones. The constant pressure on the head can lead to remodeling of the cheekbones and result in facial hemihypoplasia or plagiocephaly. These changes affect proper breastfeeding positioning, making it difficult for the baby to suckle during breastfeeding. Throughout the child's motor development, language, and balance in different positions, such as sitting and crawling, compensations from disparate systems may occur, potentially resulting in consequences on orthostatic postures, such as scoliosis.[21]
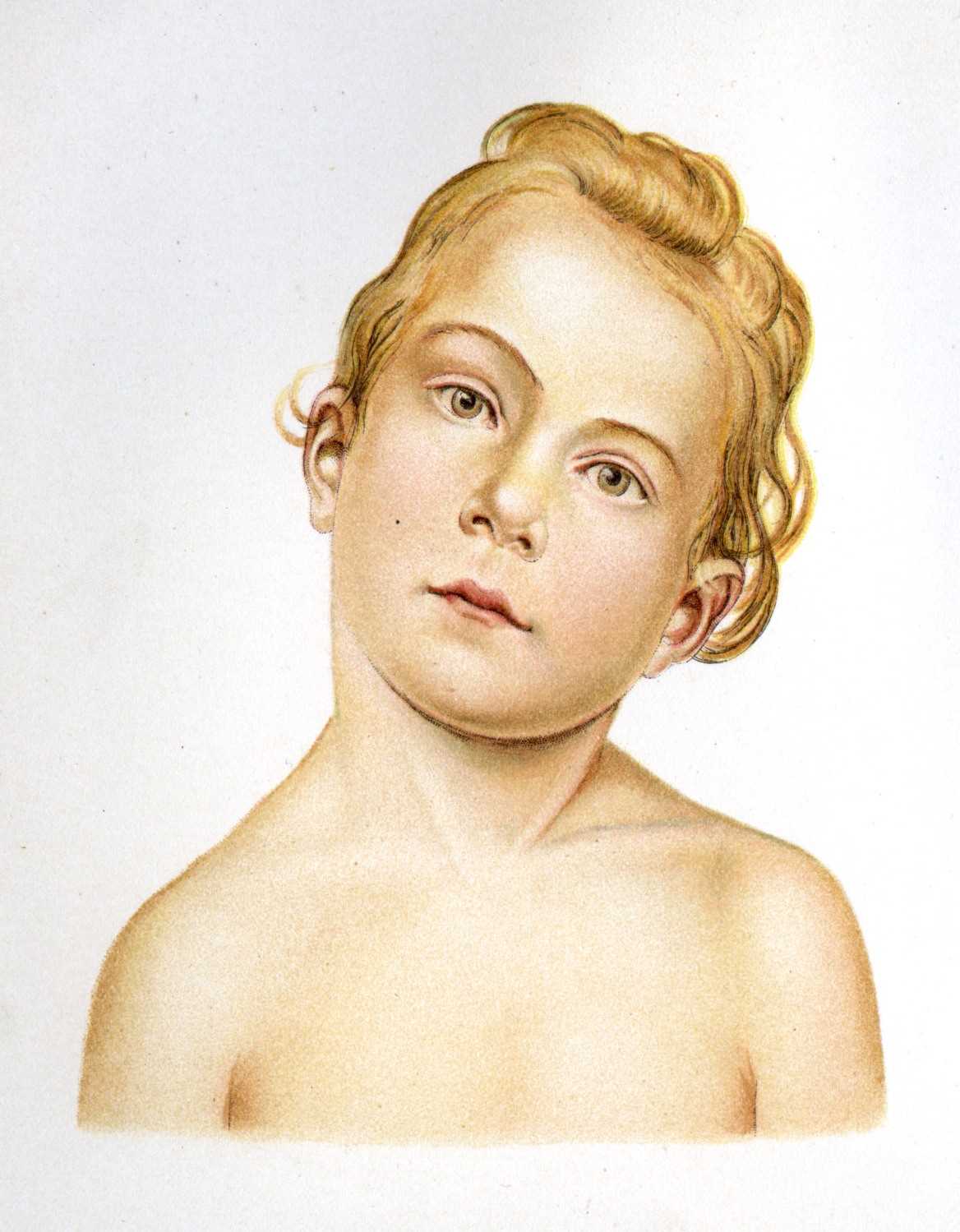
In older children, the sternocleidomastoid muscle often appears thickened and condensed along its length, resulting in restricted rotation and lateral neck flexion towards the unaffected side (see Image. Child with Torticollis). These rotational changes can lead to flattening of the head, known as positional plagiocephaly. This condition may correlate with other musculoskeletal abnormalities, such as positional musculoskeletal deformities, including metatarsus adductus, calcaneovalgus feet, developmental dysplasia of the hip, and brachial plexus palsy.[2]
Evaluation
Physical examination is the easiest and most effective means of diagnosing congenital torticollis. Assessment methods include evaluating the passive cervical range of motion using an arthrodial goniometer, often performed by physical therapists. Additionally, assessing an active range of motion, if possible, and conducting a global assessment is essential.
Neurological and auditory assessments are fundamental to exclude other potential differential diagnoses. It is crucial to evaluate visual function, including eye alignment, the presence of red reflex, and pupillary reaction to light, to determine whether the eyes fixate and follow objects. Weakness in oculomotor muscles, such as the lateral rectus or superior oblique, may suggest that the torticollis results from a compensatory mechanism to improve vision.
During physical examination, if no muscle contracture is evident and joint amplitudes remain intact, this suspicion warrants referral to ophthalmology.[22] A collaborative approach involving ophthalmologists and other relevant specialists can ensure comprehensive care and optimal outcomes for patients with suspected visual involvement in congenital torticollis.
The incidence of hip dysplasias in patients with congenital torticollis is approximately 15%; however, other studies report that 1 in 5 babies with congenital torticollis has associated hip dysplasias. Regular hip examination and ultrasound scan by 4 to 6 weeks of age or a plain radiograph of the hips at 4 to 6 months are recommended.[2] Several risk factors correlate with a higher incidence of hip dysplasia, including female sex, first childbirth, family history of hip dysplasia, presence of other deformities such as congenital torticollis, birth with a pelvic presentation, cesarean delivery, and large fetus. While hip dysplasia can be bilateral, it is most often unilateral.
Early diagnosis of hip dysplasia is crucial as it is typically asymptomatic in newborns, and early detection allows for effective treatment, thereby improving prognosis. Late diagnosis can result in sequelae such as lameness, chronic pain, degenerative arthritis, and mental impairment. Thus, appropriate screening for this condition is essential, focusing on clinical signs indicative of hip dysplasia and the need for early diagnosis. When in doubt, referral to a specialist is recommended.
The clinical diagnosis of hip dysplasia systematically relies on major and minor clinical signs. Major signs are the Ortolani/Barlow sign and hip abduction limitation, while minor signs encompass the Galeazzi sign and asymmetry of the folds (inguinal and thighs).[23]
The evaluation of congenital torticollis plays a crucial role in treatment planning.[2][24] Diagnosis is primarily clinical, with only a few cases requiring complementary diagnostic tests. Typically, diagnosis occurs 2 months of age in 50% of cases, often identified by parents and sometimes correlated with plagiocephaly.
Ultrasonography is the most common imaging modality, especially in the neonatal period. Magnetic resonance imaging (MRI) can be helpful to rule out nonmuscular causes of torticollis. Ultrasound is advantageous for assessing a neck mass, such as a pseudotumor, and long-term monitoring and posttreatment evaluation.
The tumor on the affected side of the neck along the sternocleidomastoid muscle usually resolves between 4 and 8 months of age.[2][25][26] Histopathologic studies are rarely necessary when imaging modalities regarding the etiology are inconclusive. Fine-needle aspiration cytology (FNAC) specimens are an option. Biopsy or surgical specimens yield fewer findings in the early course of the condition since they are obtained later in the disease course.
Treatment / Management
Treatment of congenital torticollis can be approached in several ways, with no standardized therapeutic approach. Professionals from various fields, including physiotherapy and osteopathy, may recommend techniques for treating torticollis in infants.[27]
With proper treatment, 90% to 95% of children show improvement before the first year of life, and 97% of patients improve if treatment begins before the first 6 months.[20][28][29] In cases of congenital torticollis, a palpable sternocleidomastoid mass is an important indicator for initiating intervention by the second month of life, as it influences the child's normal motor development.[10] The main objective is to attain an age-appropriate active and passive range of motion of the neck to prevent contractures and promote symmetry of the face, head, and neck.
Initial treatment focuses on passive range stretching and close follow-up. Parents are advised to incorporate positioning maneuvers into the infant's daily routine, such as during feeds, including chin rotation towards the affected shoulder. Infants can also benefit from supervised time spent on their stomachs when awake, facilitating motor skill development in the prone position.
Manual stretches involving flexion, extension, and lateral rotation should be performed at least 3 times a week, with each set comprising 15 stretches. Each stretch should be held for 1 second with a 10-second pause between each repetition. If the sternocleidomastoid muscle exhibits a fibrous aspect, stretching techniques are considered the most essential and evidence-based treatment.[2][7]
While numerous protocol studies in the literature demonstrate the effectiveness of physical therapy for congenital torticollis, there is limited reported data on the frequency and types of exercise. In many studies, the initial frequency of therapy sessions ranged from 2 times per week in the 1st month, progressing to once per week; some authors advocate for an initial frequency of 3 times a week. The duration of physiotherapy treatment for congenital torticollis varies depending on the timing of rehabilitation initiation, with studies indicating that earlier intervention leads to quicker establishment of normal cervical biomechanics and better outcomes. Published studies predominantly focus on stretching, muscle energy techniques, and other exercises promoting motor development.[30]
The Tubular Orthosis for Torticollis (TOT) collar is recommended for children over 4 months of age. It supports the impaired side of the neck in a neutral position and can be worn during the daytime while the child is awake.[31]
Physical therapy may not always yield effective results for treatment, prompting the exploration of alternative interventions. One such approach involves the adjunctive use of botulinum toxin injections in the sternocleidomastoid muscle and other affected muscles in the region.[32] Surgery may be considered a last resort in more severe cases where conservative measures fail. However, physical therapy remains integral at all stages of treatment and follow-up. A retrospective study has reported that botulinum toxin type A is a safe and effective treatment option for refractory cases of congenital torticollis.[33]
Surgical intervention may be indicated in cases where there is no improvement after 6 months of manual stretching, if there are more than 15°in passive rotation and lateral bending, or if a tight muscular band is present in the sternocleidomastoid muscle. Surgical procedures may include unipolar or bipolar sternocleidomastoid muscle lengthening, "Z" lengthening, or radical resection of the sternocleidomastoid muscle.[34][35]
Surgical management has yielded positive outcomes in patients with long-standing untreated torticollis, including correction of head position and improvement in cervical range of motion. However, facial asymmetry typically does not get corrected through surgical intervention.[36] Additionally, a prospective study has reported significant improvements in health-related quality of life and clinical outcomes after surgical treatment of congenital torticollis.[37]
Differential Diagnosis
Differential diagnosis is essential to rule out other pathologies. Some of the potential differential diagnoses for congenital torticollis include:
- Vertebral anomalies like hemivertebrae and Klippel-Feil Syndrome
- Unilateral congenital absence of the sternocleidomastoid muscle
- Congenital scoliosis
- Ocular torticollis
- Sandifer syndrome
- Arnold Chiari malformation
- Neurological diseases
- Visual disturbances
- Syringomyelia
- Cervical spine tumor
- Brain tumor [8][26]
Prognosis
Most cases of congenital torticollis are benign and resolve spontaneously or with manual stretching. With proper treatment, 90% to 95% of children improve before the first year of life, and 97% of patients improve if treatment starts before the first 6 months. Craniofacial asymmetry also improves, especially in cases treated early. When the patients present late or when physical therapy fails to yield results, surgical management may be necessary. The results of surgical treatment are generally positive, with improvement in neck range of motion and correction of deformity.[8]
Complications
Delayed or unavailable treatment for congenital torticollis can lead to permanent anatomic abnormalities, including disfigurement, cosmetic concerns, and functional impairment. Craniofacial asymmetry may develop as a long-term complication if the contracted sternocleidomastoid muscle is not released. Therefore, it is imperative to correct torticollis promptly to prevent the progression of facial asymmetry and mitigate potential long-term consequences.[22]
Positional plagiocephaly is commonly associated with muscular torticollis, underscoring the importance of distinguishing this benign condition and craniosynostosis. A careful examination of the sutures, along with imaging such as a radiograph or ultrasound, may be necessary for accurate differentiation.
Management of plagiocephaly involves advising parents to implement frequent positional changes to halt the skull remodeling. Referral to physical therapy to improve neck motion is paramount for comprehensive management.
Deterrence and Patient Education
Early suspicion and identification of the condition are of paramount importance. Parents should report to the pediatrician or a physical therapist if they notice a swelling in the neck muscle or any neck deformity in children. With early diagnosis, the prognosis is generally good, and most cases can be fully corrected with stretching exercises. However, delayed diagnosis may necessitate surgical management, and persistent facial and skull asymmetry may occur.
Pearls and Other Issues
Key points to keep in mind about congenital torticollis include the following:
- Torticollis is characterized by a contraction or fibrosis of the sternocleidomastoid muscle, leading to abnormal head and neck positioning.
- Torticollis can occur due to congenital and acquired causes, including intrauterine factors, trauma during birth, or idiopathic factors.
- Typical signs and symptoms of torticollis include lateral tilt of the head, contralateral rotation of the chin, and restricted range of motion of the neck.
- Physical examination includes evaluation of the neck's passive and active range of motion.
- Ultrasonography or MRI may confirm the diagnosis and rule out other potential pathologies.
- Primary treatment modalities for torticollis include conservative measures such as stretching exercises and physical therapy.
- Potential complications of untreated or inadequately managed torticollis include craniofacial asymmetry, functional impairment, and long-term musculoskeletal abnormalities.
Enhancing Healthcare Team Outcomes
An interprofessional team is best suited to manage congenital torticollis effectively, minimizing postural morbidity. Typically, parents are the first to identify the condition and seek evaluation from the primary care provider. Early identification of congenital torticollis is crucial for optimizing outcomes. Early diagnosis enables the prompt initiation of noninvasive corrective measures, which can prevent long-term disfiguring complications. Parents should receive comprehensive education about the condition, its prognosis, and their role in its management.
Healthcare providers should recognize the relationship between congenital torticollis and its impact on the child's gross motor development; most children resolve any associated motor delays by 3 to 5 years of age. A pediatric nurse should provide ongoing monitoring until congenital torticollis is resolved. Most children can expect a favorable outcome with appropriate therapy from a collaborative interprofessional team.