[1]
Armstrong D,Matangi M,Brouillard D,Myers MG, Automated office blood pressure - being alone and not location is what matters most. Blood pressure monitoring. 2015 Aug;
[PubMed PMID: 26154710]
[2]
O'Brien E,Dolan E, Ambulatory Blood Pressure Monitoring for the Effective Management of Antihypertensive Drug Treatment. Clinical therapeutics. 2016 Oct;
[PubMed PMID: 27615192]
[3]
Kjeldsen SE, Hypertension and cardiovascular risk: General aspects. Pharmacological research. 2018 Mar;
[PubMed PMID: 29127059]
[4]
Kallioinen N,Hill A,Horswill MS,Ward HE,Watson MO, Sources of inaccuracy in the measurement of adult patients' resting blood pressure in clinical settings: a systematic review. Journal of hypertension. 2017 Mar;
[PubMed PMID: 27977471]
Level 1 (high-level) evidence
[5]
Vischer AS,Burkard T, Principles of Blood Pressure Measurement - Current Techniques, Office vs Ambulatory Blood Pressure Measurement. Advances in experimental medicine and biology. 2017;
[PubMed PMID: 27417699]
Level 3 (low-level) evidence
[6]
Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research., Pickering TG,Hall JE,Appel LJ,Falkner BE,Graves J,Hill MN,Jones DW,Kurtz T,Sheps SG,Roccella EJ,, Circulation, 2005 Feb 8
[PubMed PMID: 15699287]
Level 3 (low-level) evidence
[7]
Blood pressure measurement--an overview., Dieterle T,, Swiss medical weekly, 2012 Jan 27
[PubMed PMID: 22287317]
Level 3 (low-level) evidence
[8]
Petersen NH,Ortega-Gutierrez S,Reccius A,Masurkar A,Huang A,Marshall RS, Comparison of non-invasive and invasive arterial blood pressure measurement for assessment of dynamic cerebral autoregulation. Neurocritical care. 2014 Feb;
[PubMed PMID: 24452959]
[9]
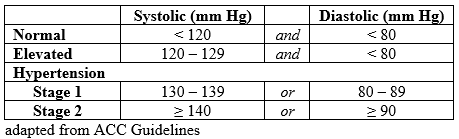
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr, Williamson JD, Wright JT Jr. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Journal of the American College of Cardiology. 2018 May 15:71(19):e127-e248. doi: 10.1016/j.jacc.2017.11.006. Epub 2017 Nov 13
[PubMed PMID: 29146535]
Level 1 (high-level) evidence
[11]
Pittman JA,Ping JS,Mark JB, Arterial and central venous pressure monitoring. International anesthesiology clinics. 2004 Winter;
[PubMed PMID: 14716195]
[12]
Wang KM,Sirich TL,Chang TI, Timing of blood pressure medications and intradialytic hypotension. Seminars in dialysis. 2019 Mar 5;
[PubMed PMID: 30836447]
[13]
Mühlbauer V,Dallmeier D,Brefka S,Bollig C,Voigt-Radloff S,Denkinger M, The Pharmacological Treatment of Arterial Hypertension in Frail, Older Patients. Deutsches Arzteblatt international. 2019 Jan 18;
[PubMed PMID: 30832759]
[14]
Leal J,Morrow LM,Kurshid W,Pagano E,Feenstra T, Decision models of prediabetes populations: a systematic review. Diabetes, obesity
[PubMed PMID: 30828927]
Level 1 (high-level) evidence
[15]
Phelps PK,Kelley EF,Walla DM,Ross JK,Simmons JJ,Bulock EK,Ayres A,Akre MK,Sprissler R,Olson TP,Snyder EM, Relationship between a Weighted Multi-Gene Algorithm and Blood Pressure Controlin Hypertension. Journal of clinical medicine. 2019 Feb 28;
[PubMed PMID: 30823438]
[16]
Di Bonito P,Valerio G,Pacifico L,Chiesa C,Invitti C,Morandi A,Licenziati MR,Manco M,Giudice EMD,Baroni MG,Loche S,Tornese G,Franco F,Maffeis C,de Simone G, Impact of the 2017 Blood Pressure Guidelines by the American Academy of Pediatrics in overweight/obese youth. Journal of hypertension. 2019 Apr;
[PubMed PMID: 30817454]