[1]
Priddis H, Dahlen HG, Schmied V, Sneddon A, Kettle C, Brown C, Thornton C. Risk of recurrence, subsequent mode of birth and morbidity for women who experienced severe perineal trauma in a first birth in New South Wales between 2000-2008: a population based data linkage study. BMC pregnancy and childbirth. 2013 Apr 8:13():89. doi: 10.1186/1471-2393-13-89. Epub 2013 Apr 8
[PubMed PMID: 23565655]
[2]
Goh R, Goh D, Ellepola H. Perineal tears - A review. Australian journal of general practice. 2018 Jan-Feb:47(1-2):35-38. doi: 10.31128/AFP-09-17-4333. Epub
[PubMed PMID: 29429318]
[3]
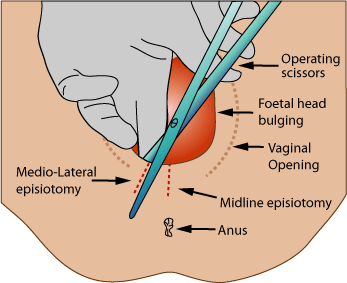
Kalis V, Laine K, de Leeuw JW, Ismail KM, Tincello DG. Classification of episiotomy: towards a standardisation of terminology. BJOG : an international journal of obstetrics and gynaecology. 2012 Apr:119(5):522-6. doi: 10.1111/j.1471-0528.2011.03268.x. Epub 2012 Feb 3
[PubMed PMID: 22304364]
[4]
Melo I, Katz L, Coutinho I, Amorim MM. Selective episiotomy vs. implementation of a non episiotomy protocol: a randomized clinical trial. Reproductive health. 2014 Aug 14:11():66. doi: 10.1186/1742-4755-11-66. Epub 2014 Aug 14
[PubMed PMID: 25124938]
Level 1 (high-level) evidence
[5]
Shmueli A, Gabbay Benziv R, Hiersch L, Ashwal E, Aviram R, Yogev Y, Aviram A. Episiotomy - risk factors and outcomes(). The journal of maternal-fetal & neonatal medicine : the official journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the International Society of Perinatal Obstetricians. 2017 Feb:30(3):251-256
[PubMed PMID: 27018243]
[6]
American College of Obstetricians-Gynecologists. ACOG Practice Bulletin. Episiotomy. Clinical Management Guidelines for Obstetrician-Gynecologists. Number 71, April 2006. Obstetrics and gynecology. 2006 Apr:107(4):957-62
[PubMed PMID: 16582142]
[7]
Frohlich J, Kettle C. Perineal care. BMJ clinical evidence. 2015 Mar 10:2015():. pii: 1401. Epub 2015 Mar 10
[PubMed PMID: 25752310]
[8]
Jiang H, Qian X, Carroli G, Garner P. Selective versus routine use of episiotomy for vaginal birth. The Cochrane database of systematic reviews. 2017 Feb 8:2(2):CD000081. doi: 10.1002/14651858.CD000081.pub3. Epub 2017 Feb 8
[PubMed PMID: 28176333]
Level 2 (mid-level) evidence
[9]
Helewa ME. Episiotomy and severe perineal trauma. Of science and fiction. CMAJ : Canadian Medical Association journal = journal de l'Association medicale canadienne. 1997 Mar 15:156(6):811-3
[PubMed PMID: 9084387]
[10]
Sultan AH, Thakar R, Ismail KM, Kalis V, Laine K, Räisänen SH, de Leeuw JW. The role of mediolateral episiotomy during operative vaginal delivery. European journal of obstetrics, gynecology, and reproductive biology. 2019 Sep:240():192-196. doi: 10.1016/j.ejogrb.2019.07.005. Epub 2019 Jul 9
[PubMed PMID: 31310920]
[11]
Marty N, Verspyck E. [Perineal tears and episiotomy: Surgical procedure - CNGOF perineal prevention and protection in obstetrics guidelines]. Gynecologie, obstetrique, fertilite & senologie. 2018 Dec:46(12):948-967. doi: 10.1016/j.gofs.2018.10.024. Epub 2018 Nov 2
[PubMed PMID: 30392991]
[12]
Kettle C, Dowswell T, Ismail KM. Continuous and interrupted suturing techniques for repair of episiotomy or second-degree tears. The Cochrane database of systematic reviews. 2012 Nov 14:11(11):CD000947. doi: 10.1002/14651858.CD000947.pub3. Epub 2012 Nov 14
[PubMed PMID: 23152204]
Level 1 (high-level) evidence
[13]
Eogan M, Daly L, O'Connell PR, O'Herlihy C. Does the angle of episiotomy affect the incidence of anal sphincter injury? BJOG : an international journal of obstetrics and gynaecology. 2006 Feb:113(2):190-4
[PubMed PMID: 16411997]
[14]
Kalis V, Landsmanova J, Bednarova B, Karbanova J, Laine K, Rokyta Z. Evaluation of the incision angle of mediolateral episiotomy at 60 degrees. International journal of gynaecology and obstetrics: the official organ of the International Federation of Gynaecology and Obstetrics. 2011 Mar:112(3):220-4. doi: 10.1016/j.ijgo.2010.09.015. Epub 2011 Jan 17
[PubMed PMID: 21247571]
[15]
May JL. Modified median episiotomy minimizes the risk of third-degree tears. Obstetrics and gynecology. 1994 Jan:83(1):156-7
[PubMed PMID: 8272298]
[16]
Alexander JW, Karantanis E, Turner RM, Faasse K, Watt C. Patient attitude and acceptance towards episiotomy during pregnancy before and after information provision: a questionnaire. International urogynecology journal. 2020 Mar:31(3):521-528. doi: 10.1007/s00192-019-04003-x. Epub 2019 Jun 26
[PubMed PMID: 31243496]
[17]
Carroli G, Mignini L. Episiotomy for vaginal birth. The Cochrane database of systematic reviews. 2009 Jan 21:(1):CD000081. doi: 10.1002/14651858.CD000081.pub2. Epub 2009 Jan 21
[PubMed PMID: 19160176]
Level 1 (high-level) evidence