[1]
Karepov Y,Kozyrev DA,Benifla M,Shapira V,Constantini S,Roth J, E-bike-related cranial injuries in pediatric population. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2019 Aug
[PubMed PMID: 30989331]
[2]
Harsh V,Vohra V,Kumar P,Kumar J,Sahay CB,Kumar A, Elevated Skull Fractures - Too Rare to Care for, Yet too Common to Ignore. Asian journal of neurosurgery. 2019 Jan-Mar
[PubMed PMID: 30937043]
[3]
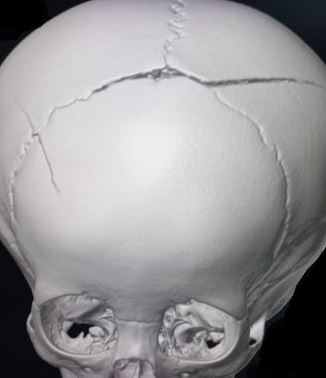
Campobasso CP,De Micco F,Bugelli V,Cavezza A,Rodriguez WC 3rd,Della Pietra B, Undetected traumatic diastasis of cranial sutures: a case of child abuse. Forensic science international. 2019 May
[PubMed PMID: 30925349]
Level 3 (low-level) evidence
[4]
Hoz SS,Dolachee AA,Abdali HA,Kasuya H, An enemy hides in the ceiling; pediatric traumatic brain injury caused by metallic ceiling fan: Case series and literature review. British journal of neurosurgery. 2019 Feb 18;
[PubMed PMID: 30773933]
Level 2 (mid-level) evidence
[6]
Donaldson K,Li X,Sartorelli KH,Weimersheimer P,Durham SR, Management of Isolated Skull Fractures in Pediatric Patients: A Systematic Review. Pediatric emergency care. 2019 Apr
[PubMed PMID: 30855424]
Level 1 (high-level) evidence
[7]
Poorman GW,Segreto FA,Beaubrun BM,Jalai CM,Horn SR,Bortz CA,Diebo BG,Vira S,Bono OJ,DE LA Garza-Ramos R,Moon JY,Wang C,Hirsch BP,Tishelman JC,Zhou PL,Gerling M,Passias PG, Traumatic Fracture of the Pediatric Cervical Spine: Etiology, Epidemiology, Concurrent Injuries, and an Analysis of Perioperative Outcomes Using the Kids' Inpatient Database. International journal of spine surgery. 2019 Jan;
[PubMed PMID: 30805288]
[8]
Oleck NC,Dobitsch AA,Liu FC,Halsey JN,Le TT,Hoppe IC,Lee ES,Granick MS, Traumatic Falls in the Pediatric Population: Facial Fracture Patterns Observed in a Leading Cause of Childhood Injury. Annals of plastic surgery. 2019 Apr
[PubMed PMID: 30730318]
[9]
Kommaraju K,Haynes JH,Ritter AM, Evaluating the Role of a Neurosurgery Consultation in Management of Pediatric Isolated Linear Skull Fractures. Pediatric neurosurgery. 2019;
[PubMed PMID: 30673671]
[10]
Harvell BJ,Helmer SD,Ward JG,Ablah E,Grundmeyer R,Haan JM, Head CT Guidelines Following Concussion among the Youngest Trauma Patients: Can We Limit Radiation Exposure Following Traumatic Brain Injury? Kansas journal of medicine. 2018 May;
[PubMed PMID: 29796153]
[11]
Tallapragada K,Peddada RS,Dexter M, Paediatric mild head injury: is routine admission to a tertiary trauma hospital necessary? ANZ journal of surgery. 2018 Mar
[PubMed PMID: 28922710]
[12]
Azim A,Jehan FS,Rhee P,O'Keeffe T,Tang A,Vercruysse G,Kulvatunyou N,Latifi R,Joseph B, Big for small: Validating brain injury guidelines in pediatric traumatic brain injury. The journal of trauma and acute care surgery. 2017 Dec;
[PubMed PMID: 28590352]
[13]
Talari HR,Hamidian Y,Moussavi N,Fakharian E,Abedzadeh-Kalahroudi M,Akbari H,Taher EB, The Prognostic Value of Rotterdam Computed Tomography Score in Predicting Early Outcomes Among Children with Traumatic Brain Injury. World neurosurgery. 2019 Jan 21;
[PubMed PMID: 30677579]
[14]
Orru' E,Huisman TAGM,Izbudak I, Prevalence, Patterns, and Clinical Relevance of Hypoxic-Ischemic Injuries in Children Exposed to Abusive Head Trauma. Journal of neuroimaging : official journal of the American Society of Neuroimaging. 2018 Nov
[PubMed PMID: 30125430]