Continuing Education Activity
A radial nerve block will provide anesthesia and/or analgesia to the hand, specifically the dorsal radial side. This includes anesthesia dorsally to the thumb, index and middle fingers, and the lateral aspect of the ring finger. It can be useful as a stand-alone or adjunctive therapy for interventions of the hands and fingers, palliation of acute pain involving the radial nerve's distribution, diagnosis and treatment of radial tunnel syndrome, and a diagnostic prognostication procedure in instances of injury to the radial nerve. This activity illustrates the technique of a radial nerve block, its indication, contraindications, and complication.
Objectives:
- Identify the anatomy of the radial nerve.
- Describe the technique of a radial nerve block.
- Outline the indications for a radial nerve block.
- Review the importance of enhancing care and improving outcomes in patients undergoing a radial nerve block.
Introduction
Radial nerve anesthesia rests upon disrupting impulse conduction in the nerve with drugs such as local anesthetics that can be given locally to block specific nerves and can be reversed as needed. Disrupting nerve impulse conduction can be done in any region of the body where nerves are easily accessible for visualization and injection. A radial nerve block will provide anesthesia and/or analgesia to the hand, specifically the dorsal radial side. This includes anesthesia dorsally to the thumb, index and middle fingers, and the lateral aspect of the ring finger.[1] It can be useful as a stand-alone or adjunctive therapy for interventions of the hands and fingers, palliation of acute pain involving the radial nerve's distribution, diagnosis and treatment of radial tunnel syndrome, and a diagnostic prognostication procedure in instances of injury to the radial nerve. This block is especially useful for the clinician as an alternative to procedural sedation and escalating opioid analgesic requirements for acutely painful conditions such as fractures, lacerations, and burns.
Anatomy and Physiology
The radial nerve, along with the axillary artery, originates as a branch of the brachial plexus, specifically from the posterior cord of the plexus. The nerve is comprised of fibers from C5-T1 spinal roots. Proximally, the radial nerve is found posterior and inferior to the axillary artery. Once it exits the axilla, the nerve descends into the arm by passing anterior to the latissimus dorsi muscle insertion and then passes between the medial and long heads of the triceps muscle to eventually lie on the posterior surface of the humerus. The radial nerve has multiple branches, including the sensory posterior cutaneous branch of the forearm and the superficial radial nerve, as well as the motor deep radial nerve. The posterior cutaneous branch divides from the radial nerve proximal to the humeral lateral epicondyle, providing sensation to the elbow and the posterior forearm. Continuing distally, the radial nerve courses over the humeral spiral groove and emerges close to the lateral epicondyle. It subsequently pierces the lateral intermuscular septum to arrive at the anterior compartment of the arm, lying in-between the brachialis and brachioradialis muscles. Here, at the level of the antecubital fossa, it divides into its two terminal branches, the superficial and deep branches. The superficial branch is close to the radial artery, responsible for afferent innervation. This is a sensory branch, innervating the geographical area of the wrist dorsally and part of the thumb and index and middle fingers proximal to the DIP dorsally. The deep branch is responsible for motor innervation to the extensors of the forearm.[2][3]
It is important to understand the anatomical path of the radial nerve as it has significant implications when attempting to achieve an anesthetic block along its course. The ideal locations of the anesthetic block described in the literature include locations above, at, and below the elbow. Above the elbow (above the bifurcation of the radial nerve into its terminal branches), the block can be done at a location 4 inches above the humeral lateral epicondyle between the brachialis and brachioradialis muscles. Additionally, the nerve can also be blocked at the level of the elbow in the antecubital fossa before the division into its terminal branches. Lastly, the superficial radial nerve can be anesthetized below the elbow at the level of the proximal third of the forearm.[2]
Indications
Indications for radial nerve block include:
- Multiple lacerations along the distribution of the radial nerve requiring repair
- Forearm and hand surgical procedures including excision of skin lesions, incision, and drainage, foreign body removal, finger amputation
- Standalone or adjunctive analgesia for acute painful injuries and burns
- Metacarpal and phalangeal fractures and dislocation
- Rescue analgesia for failed/inadequate regional blocks
- Supplemental to the median nerve block
- Radial tunnel syndrome
- Recalcitrant lateral epicondylalgia
- Post-operative pain following arthrolysis and tenolysis[4]
Contraindications
Contraindications to the radial nerve block include:
- Lack of informed consent/patient refusal
- Infection/abscess/cellulitis over the site of injection
- Allergy to the local anesthetic class
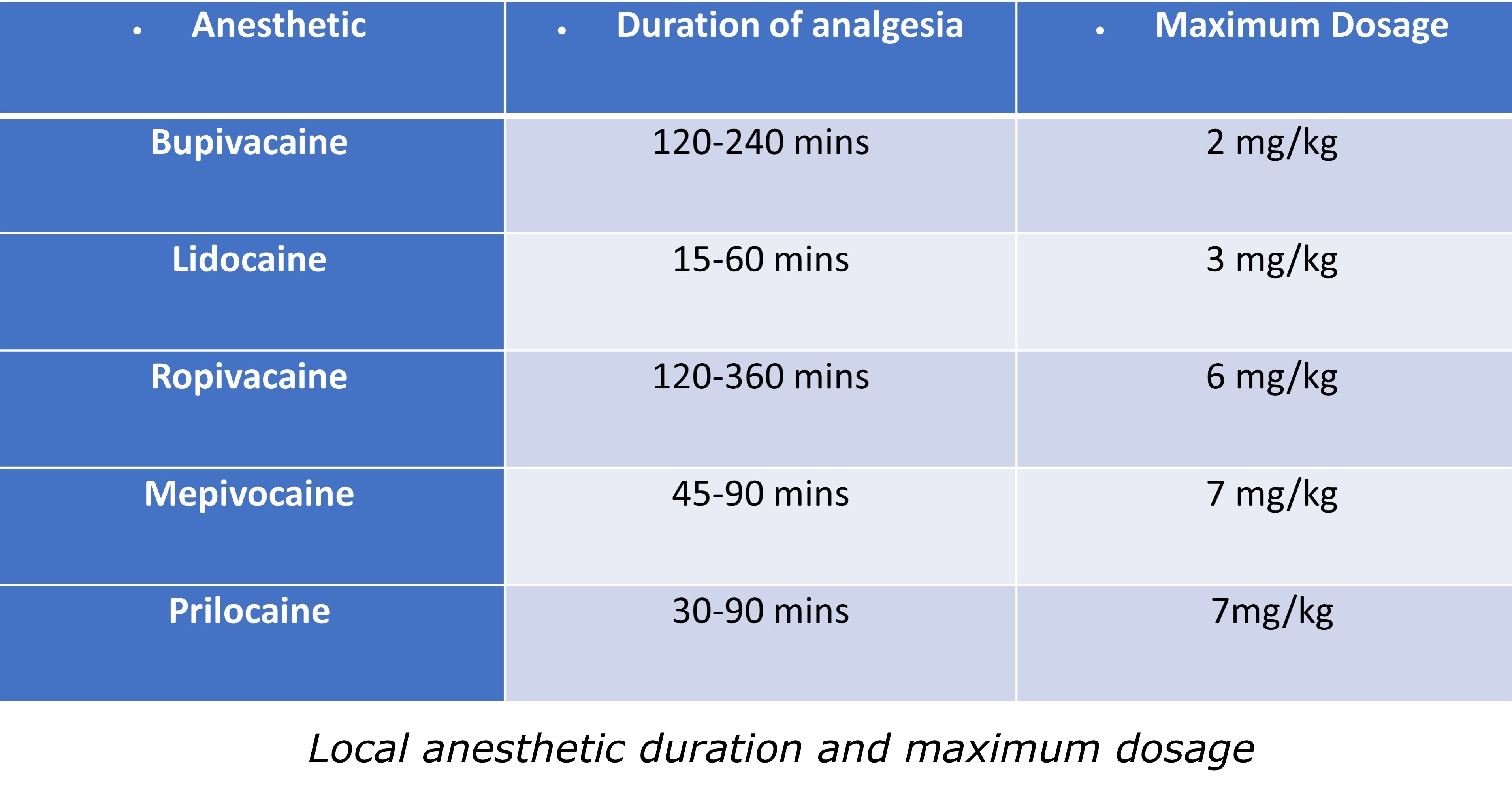
- Potential for local anesthetic systemic toxicity in regards to administering near-toxic threshold doses. Refer to Table 1 for a detailed review of anesthetic pharmacokinetics.[4]
Equipment
For an ultrasound-guided radial nerve block, the practitioner will need the following:
- Ultrasound machine with a high-frequency linear array transducer (10 to 15 MHz).
- Ultrasound probe cover (sterile) or appropriate Tegaderm dressing.
- Ultrasound gel (sterile).
- Skin preparation (sterile) (2% chlorhexidine or appropriate disinfectant).
- A 22-G to 25-G, 38-mm to 50-mm, short-bevel block needle.
- Appropriate sterile gloves.
- Local anesthetic: A volume of 3 to 5 ml suffices for each nerve. The goal is a circumferential spread of anesthetic around the nerve sheath. The use of anesthetic concentration versus duration must be made before starting the procedure to choose the most suitable anesthetic for the block.
- Ergonomics: Recommendation is for the individual doing the anesthetic block to stand on the ipsilateral side as the block with the ultrasound on the contralateral side.[4][5]
Personnel
Properly trained personnel with experience using ultrasound-guided regional anesthesia should perform the procedure with adequate support staff.[4]
Preparation
After obtaining informed consent, position the patient depending on which approach to the radial nerve block is being attempted as outlined below in the technique section. Subsequently, either povidone-iodine or chlorhexidine 2% can be used to prepare the skin over the site of anesthetic injection. Next, applying a sterile probe cover to the ultrasound probe is recommended, followed by the application of sterile gel to the intended injection site. Lastly, a local anesthetic is drawn up into a syringe. Ensure appropriate monitoring and access to 20% lipid emulsion in cases of local anesthetic systemic toxicity.[4]
Technique or Treatment
There are 3 techniques with which to attempt an anesthetic block to the radial nerve.
Proximal Third of the Forearm
An anesthetic block can be performed in this location before the superficial radial nerve joins the lateral aspect of the radial artery proximal to its division into smaller branches.
- The patient can be supine or be sitting upright. Have the patient pronate their arm to facilitate placement of the needle with the operator standing on the lateral (cephalad) side of the arm-board.
- Here, the superficial radial nerve is covered by the brachioradialis muscle. Place the linear ultrasound transducer, preferably in an in-plane approach from the lateral side of the forearm. Use a 25-gauge needle, preferably 38 mm in length, for this procedure.
- Identify the radial nerve at an initial depth of 25 mm under the brachioradialis muscle using the ultrasound. Upon scanning, the radial nerve is seen as a hyperechoic structure underneath the brachioradialis muscle.
- Place the needle tip in an in-plane view from lateral to medial through the brachioradialis muscle adjacent to the superficial radial nerve.
- Confirm that there is no inadvertent entry into the vasculature via negative aspiration.
- Inject local anesthetic of choice and observe for layering of local anesthetic under the brachioradialis muscle and around the superficial radial nerve.[6]
At the Elbow in the Antecubital Fossa
An anesthetic block can be performed here at the antecubital fossa before the nerve divides into superficial (sensory) and deep (motor) branches.
- The patient can be supine or be sitting upright. Have the patient supinate their arm to facilitate placement of the needle with the operator standing on the lateral (cephalad) side of the arm-board.
- Place the ultrasound, using the linear transducer, preferably in an in-plane approach from the lateral side of the elbow. Use a 25-gauge needle, preferably 50 mm in length, for this procedure.
- Identify the radial nerve between the brachioradialis and the biceps muscle in this location. Our preferred approach is to start proximally above the elbow and identify the radial nerve as a triangular hyperechoic structure coming off the distal humerus. We suggest following this distally to the antecubital fossa, where the nerve will branch into its superficial and deep branches.
- After identification, choose a point of injection before the bifurcation of the radial nerve.
- Place the needle tip in an in-plane view from lateral to medial until you enter the fascial plane adjacent to the radial nerve.
- Confirm that the tip is not in a vascular space by negative aspiration
- Inject local anesthetic of choice and observe for layering of a local anesthetic around the radial nerve.[6]
Above the Elbow Just Distal to the Humeral Spiral Groove
An anesthetic block can be performed here at the level of the spiral groove on the posterolateral aspect of the humerus to block the deep and superficial branches of the radial nerve.
- The patient can be supine with the arm placed in shoulder adduction, and internal rotation with the elbow flexed and rested on the patient’s chest. The operator should be standing on the lateral (cephalad) side of the arm-board.
- Place the ultrasound, using the linear transducer, preferably in an in-plane approach on the spiral groove of the posterolateral humerus distally. Use a 25-gauge needle, preferably 50 mm in length, for this procedure.
- Identify the radial nerve as a triangular hyperechoic structure coming off the humerus at this location.
- Place the needle tip in an in-plane view from lateral to medial until it enters the fascial plane adjacent to the radial nerve.
- Confirm that the tip is not in a vascular space by negative aspiration
- Inject local anesthetic of choice and observe for layering of a local anesthetic around the radial nerve.[6]
Complications
Complications include:
- Nerve injury including neuropraxia or neurolysis
- Hematoma formation
- Myalgias
- Intravascular injections
- Systemic local anesthesia toxicity
- Infection
- Bleeding at the site of puncture
- Allergic reaction to a local anesthetic
- Myotoxicity and myonecrosis with frequent or prolonged injections
- Reflex sympathetic dystrophy[4]
Clinical Significance
The use of local peripheral nerve blocks for surgical anesthesia, post-operative pain, acute and chronic pain syndromes, as well as a multitude of other indications has significantly increased with the advent of ultrasound-guided techniques. Furthermore, the use of ultrasound has improved the overall success and efficiency of the peripheral nerve block while minimizing local anesthetic toxicity risk.[7]
Enhancing Healthcare Team Outcomes
The utilization of peripheral ultrasound-guided nerve blocks helps provide a viable alternative to procedural sedation, which has potential risks and is both labor and time-intensive to both patients and physicians. The use of ultrasound has been classified as Level 1b evidence for faster block onset and higher rates of block success by the American Society of Regional Anesthesia and Pain Medicine. An ultrasound-guided radial nerve block, alone or combined with other treatments, represents a therapeutic resource for treating multiple different types of pain and clinical entities.