[5]
Kiecker C,Bates T,Bell E, Molecular specification of germ layers in vertebrate embryos. Cellular and molecular life sciences : CMLS. 2016 Mar;
[PubMed PMID: 26667903]
[6]
Hall BK, Germ layers, the neural crest and emergent organization in development and evolution. Genesis (New York, N.Y. : 2000). 2018 Jun;
[PubMed PMID: 29637683]
[7]
Gole RA,Meshram PM,Hattangdi SS, Anencephaly and its associated malformations. Journal of clinical and diagnostic research : JCDR. 2014 Sep;
[PubMed PMID: 25386414]
[8]
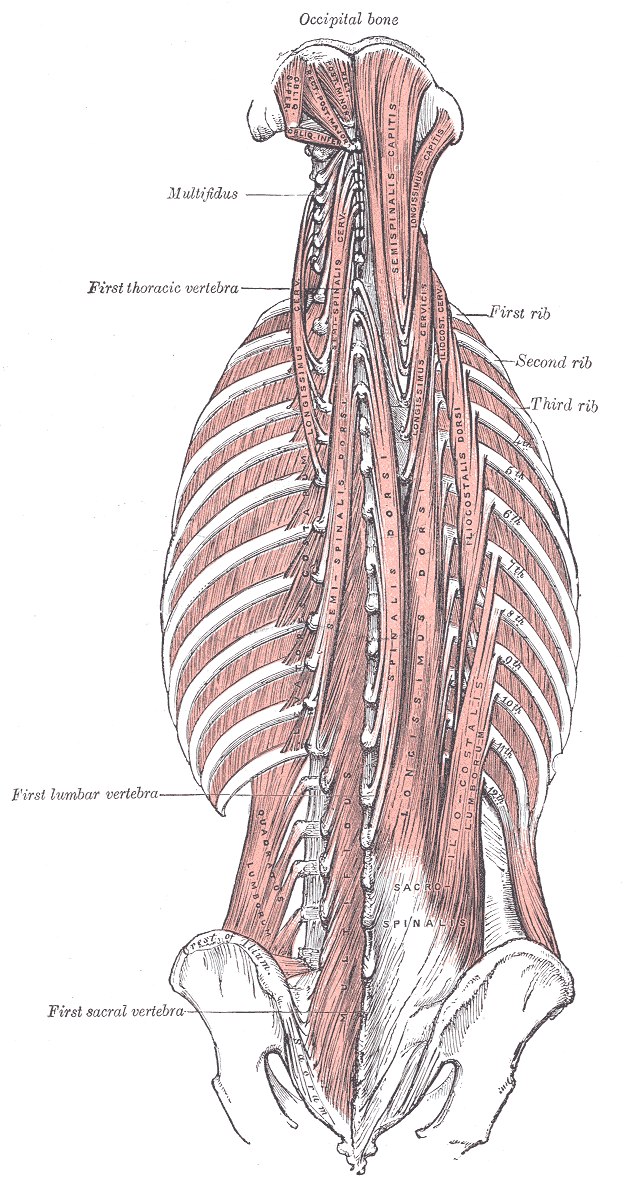
Sato T, Koizumi M, Kim JH, Kim JH, Wang BJ, Murakami G, Cho BH. Fetal development of deep back muscles in the human thoracic region with a focus on transversospinalis muscles and the medial branch of the spinal nerve posterior ramus. Journal of anatomy. 2011 Dec:219(6):756-65. doi: 10.1111/j.1469-7580.2011.01430.x. Epub 2011 Sep 29
[PubMed PMID: 21954879]
[9]
Kocbek L,Rakuša M, Common trunk of the posterior intercostal arteries from the thoracic aorta: anatomical variation, frequency, and importance in individuals. Surgical and radiologic anatomy : SRA. 2018 Apr;
[PubMed PMID: 29532168]
[10]
Dewhurst C,O'Neill S,O'Regan K,Maher M, Demonstration of the course of the posterior intercostal artery on CT angiography: relevance to interventional radiology procedures in the chest. Diagnostic and interventional radiology (Ankara, Turkey). 2012 Mar-Apr;
[PubMed PMID: 22125216]
[11]
Choi S,Trieu J,Ridley L, Radiological review of intercostal artery: Anatomical considerations when performing procedures via intercostal space. Journal of medical imaging and radiation oncology. 2010 Aug;
[PubMed PMID: 20718909]
[12]
Bley TA,Duffek CC,François CJ,Schiebler ML,Acher CW,Mell M,Grist TM,Reeder SB, Presurgical localization of the artery of Adamkiewicz with time-resolved 3.0-T MR angiography. Radiology. 2010 Jun
[PubMed PMID: 20501724]
[18]
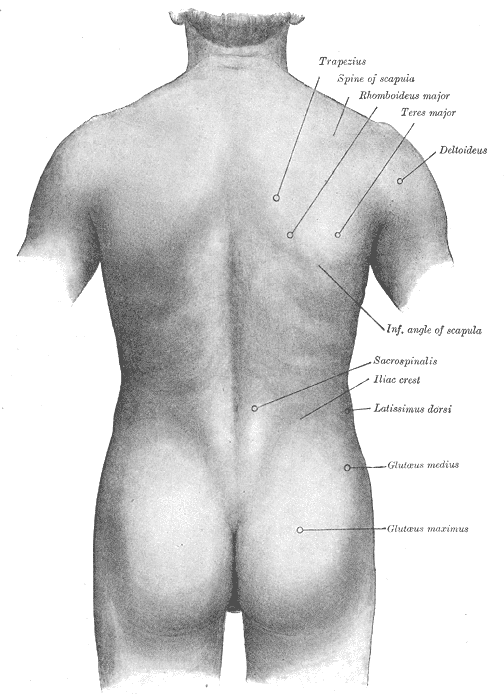
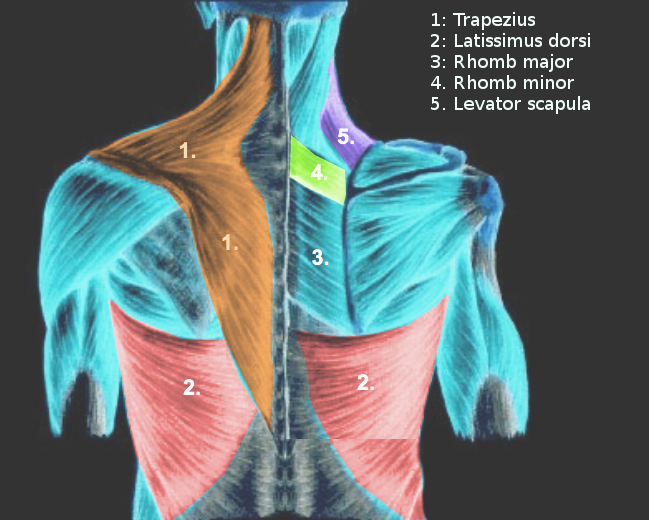
Ranade AV,Rai R,Rai AR,Dass PM,Pai MM,Vadgaonkar R, Variants of latissimus dorsi with a perspective on tendon transfer surgery: an anatomic study. Journal of shoulder and elbow surgery. 2018 Jan
[PubMed PMID: 28939333]
Level 3 (low-level) evidence
[19]
Sugiura K,Morimoto M,Higashino K,Takeuchi M,Manabe A,Takao S,Maeda T,Sairyo K, Transitional vertebrae and numerical variants of the spine : prevalence and relationship to low back pain or degenerative spondylolisthesis. The bone & joint journal. 2021 Jul
[PubMed PMID: 34192932]
[20]
Asil K,Yaldiz M, Conus Medullaris Levels on Ultrasonography in Term Newborns : Normal Levels and Dermatological Findings. Journal of Korean Neurosurgical Society. 2018 Nov;
[PubMed PMID: 30396246]
[22]
Knezevic NN,Candido KD,Vlaeyen JWS,Van Zundert J,Cohen SP, Low back pain. Lancet (London, England). 2021 Jul 3;
[PubMed PMID: 34115979]
[24]
Robinson WA,Nassr AN,Sebastian AS, Thoracic disc herniation, avoidance, and management of the surgical complications. International orthopaedics. 2019 Jan 21;
[PubMed PMID: 30666348]
[25]
Hsieh PC,Lee ST,Chen JF, Lower thoracic degenerative spondylithesis with concomitant lumbar spondylosis. Clinical neurology and neurosurgery. 2014 Mar;
[PubMed PMID: 24529224]
[26]
Gong Z,Li D,Zou F,Liu S,Wang H,Ma X, Low lumbar multifidus muscle status and bone mineral density are important risk factors for adjacent segment disease after lumbar fusion: a case-control study. Journal of orthopaedic surgery and research. 2022 Nov 16;
[PubMed PMID: 36384537]
Level 2 (mid-level) evidence
[27]
Petersen EA,Schatman ME,Sayed D,Deer T, Persistent Spinal Pain Syndrome: New Terminology for a New Era. Journal of pain research. 2021;
[PubMed PMID: 34135626]
[30]
Uçar İ,Karartı C,Cüce İ,Veziroğlu E,Özüdoğru A,Koçak FA,Dadalı Y, The relationship between muscle size, obesity, body fat ratio, pain and disability in individuals with and without nonspecific low back pain. Clinical anatomy (New York, N.Y.). 2021 Nov;
[PubMed PMID: 34378252]
[31]
Willard FH, Vleeming A, Schuenke MD, Danneels L, Schleip R. The thoracolumbar fascia: anatomy, function and clinical considerations. Journal of anatomy. 2012 Dec:221(6):507-36. doi: 10.1111/j.1469-7580.2012.01511.x. Epub 2012 May 27
[PubMed PMID: 22630613]
[32]
Abe H,Hayashi S,Kim JH,Murakami G,Rodríguez-Vázquez JF,Jin ZW, Fetal development of the thoracolumbar fascia with special reference to the fascial connection with the transversus abdominis, latissimus dorsi, and serratus posterior inferior muscles. Surgical and radiologic anatomy : SRA. 2021 Jun
[PubMed PMID: 33438110]
[33]
Sinhorim L,Amorim MDS,Ortiz ME,Bittencourt EB,Bianco G,da Silva FC,Horewicz VV,Schleip R,Reed WR,Mazzardo-Martins L,Martins DF, Potential Nociceptive Role of the Thoracolumbar Fascia: A Scope Review Involving In Vivo and Ex Vivo Studies. Journal of clinical medicine. 2021 Sep 24
[PubMed PMID: 34640360]
[35]
Wilke J, Schleip R, Klingler W, Stecco C. The Lumbodorsal Fascia as a Potential Source of Low Back Pain: A Narrative Review. BioMed research international. 2017:2017():5349620. doi: 10.1155/2017/5349620. Epub 2017 May 11
[PubMed PMID: 28584816]
Level 3 (low-level) evidence
[37]
Prakash S, Kalra P, Khan Y, Dhal A. Ventral scapular osteochondroma excision through 'triangle of auscultation': A case series. Journal of orthopaedic surgery (Hong Kong). 2020 Jan-Apr:28(1):2309499019892848. doi: 10.1177/2309499019892848. Epub
[PubMed PMID: 31916491]
Level 2 (mid-level) evidence