[1]
Jung J, Ahn HK, Huh Y. Clinical and functional anatomy of the urethral sphincter. International neurourology journal. 2012 Sep:16(3):102-6. doi: 10.5213/inj.2012.16.3.102. Epub 2012 Sep 30
[PubMed PMID: 23094214]
[2]
Heesakkers JP, Gerretsen RR. Urinary incontinence: sphincter functioning from a urological perspective. Digestion. 2004:69(2):93-101
[PubMed PMID: 15087576]
Level 3 (low-level) evidence
[6]
Merrill SB, Boorjian SA, Thompson RH, Psutka SP, Cheville JC, Thapa P, Tollefson MK, Frank I. Oncologic surveillance following radical cystectomy: an individualized risk-based approach. World journal of urology. 2017 Dec:35(12):1863-1869. doi: 10.1007/s00345-017-2068-7. Epub 2017 Jul 6
[PubMed PMID: 28685181]
[7]
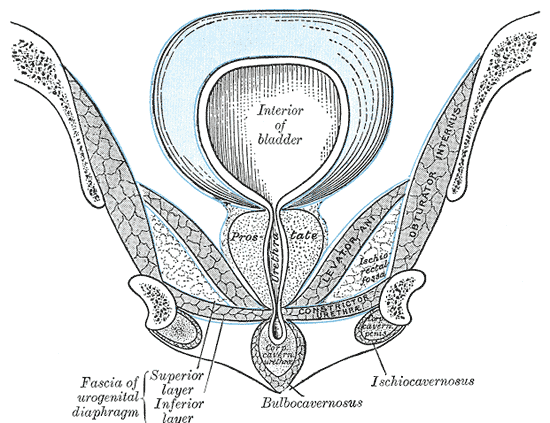
Bolla SR, Hoare BS, Varacallo M. Anatomy, Abdomen and Pelvis: Deep Perineal Space. StatPearls. 2023 Jan:():
[PubMed PMID: 30855860]
[8]
Aanestad O, Flink R. Urinary stress incontinence. A urodynamic and quantitative electromyographic study of the perineal muscles. Acta obstetricia et gynecologica Scandinavica. 1999 Mar:78(3):245-53
[PubMed PMID: 10078588]
[9]
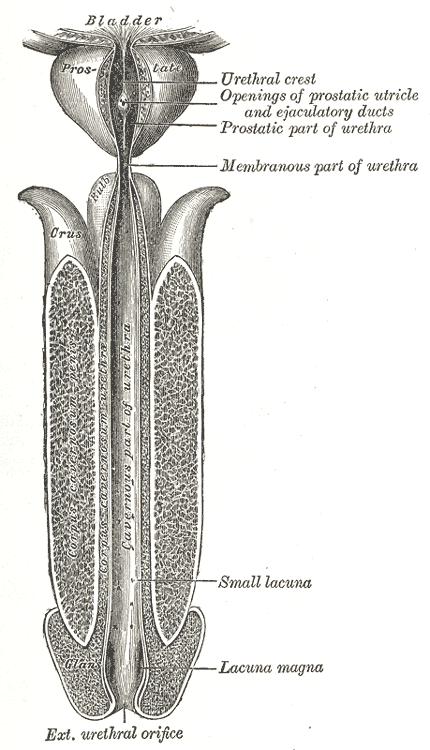
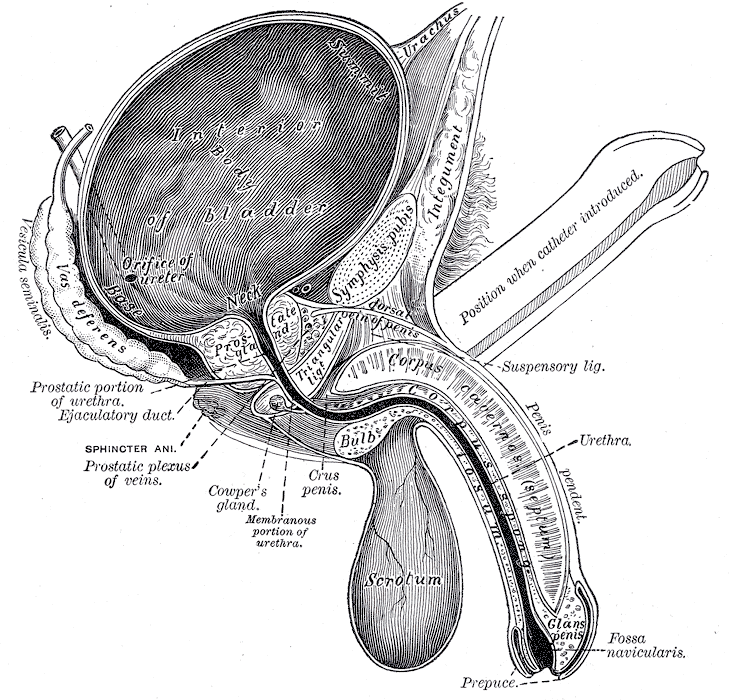
Kohler TS, Yadven M, Manvar A, Liu N, Monga M. The length of the male urethra. International braz j urol : official journal of the Brazilian Society of Urology. 2008 Jul-Aug:34(4):451-4; discussion 455-6
[PubMed PMID: 18778496]
[10]
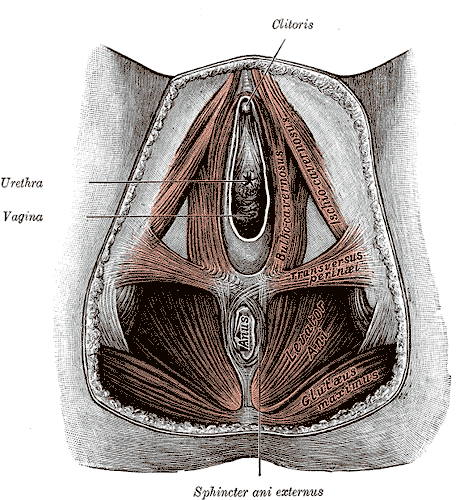
Oelrich TM. The striated urogenital sphincter muscle in the female. The Anatomical record. 1983 Feb:205(2):223-32
[PubMed PMID: 6846873]
[11]
Koraitim MM. The male urethral sphincter complex revisited: an anatomical concept and its physiological correlate. The Journal of urology. 2008 May:179(5):1683-9. doi: 10.1016/j.juro.2008.01.010. Epub 2008 Mar 17
[PubMed PMID: 18343449]
[12]
Brooks JD, Chao WM, Kerr J. Male pelvic anatomy reconstructed from the visible human data set. The Journal of urology. 1998 Mar:159(3):868-72
[PubMed PMID: 9474171]
[17]
Juenemann KP, Lue TF, Schmidt RA, Tanagho EA. Clinical significance of sacral and pudendal nerve anatomy. The Journal of urology. 1988 Jan:139(1):74-80
[PubMed PMID: 3275803]
[18]
Zvara P, Carrier S, Kour NW, Tanagho EA. The detailed neuroanatomy of the human striated urethral sphincter. British journal of urology. 1994 Aug:74(2):182-7
[PubMed PMID: 7921935]
[19]
Rajaofetra N, Passagia JG, Marlier L, Poulat P, Pellas F, Sandillon F, Verschuere B, Gouy D, Geffard M, Privat A. Serotoninergic, noradrenergic, and peptidergic innervation of Onuf's nucleus of normal and transected spinal cords of baboons (Papio papio). The Journal of comparative neurology. 1992 Apr 1:318(1):1-17
[PubMed PMID: 1374763]
Level 2 (mid-level) evidence
[21]
Sam P, Nassereddin A, LaGrange CA. Anatomy, Abdomen and Pelvis: Bladder Detrusor Muscle. StatPearls. 2023 Jan:():
[PubMed PMID: 29489195]
[22]
Ahmed DG, Mohamed MF, Mohamed SA. Superior hypogastric plexus combined with ganglion impar neurolytic blocks for pelvic and/or perineal cancer pain relief. Pain physician. 2015 Jan-Feb:18(1):E49-56
[PubMed PMID: 25675070]
[23]
Tong XK, Huo RJ. The anatomical basis and prevention of neurogenic voiding dysfunction following radical hysterectomy. Surgical and radiologic anatomy : SRA. 1991:13(2):145-8
[PubMed PMID: 1925917]
[26]
Hudson CN, Sohaib SA, Shulver HM, Reznek RH. The anatomy of the perineal membrane: its relationship to injury in childbirth and episiotomy. The Australian & New Zealand journal of obstetrics & gynaecology. 2002 May:42(2):193-6
[PubMed PMID: 12069149]
[27]
Schiøtz HA. Periurethral injection therapy in women with stress incontinence. Tidsskrift for den Norske laegeforening : tidsskrift for praktisk medicin, ny raekke. 2019 Jan 29:139(2):. doi: 10.4045/tidsskr.18.0185. Epub 2019 Jan 24
[PubMed PMID: 30698387]
[28]
Dumoulin C, Pazzoto Cacciari L, Mercier J. Keeping the pelvic floor healthy. Climacteric : the journal of the International Menopause Society. 2019 Jun:22(3):257-262. doi: 10.1080/13697137.2018.1552934. Epub 2019 Jan 17
[PubMed PMID: 30653374]
[29]
Nalbant İ, Tuygun C, Öztürk U, Göktuğ HNG, Karakoyunlu AN, Selmi V, İmamoğlu MA. Do the etiological factors in artificial urinary sphincter reimplantation cases affect success and complications? Turkish journal of medical sciences. 2018 Dec 12:48(6):1263-1267. doi: 10.3906/sag-1805-150. Epub 2018 Dec 12
[PubMed PMID: 30541256]
Level 3 (low-level) evidence
[30]
Tunn R, Goldammer K, Neymeyer J, Gauruder-Burmester A, Hamm B, Beyersdorff D. MRI morphology of the levator ani muscle, endopelvic fascia, and urethra in women with stress urinary incontinence. European journal of obstetrics, gynecology, and reproductive biology. 2006 Jun 1:126(2):239-45
[PubMed PMID: 16298035]
[31]
Shek KL, Dietz HP. Intrapartum risk factors for levator trauma. BJOG : an international journal of obstetrics and gynaecology. 2010 Nov:117(12):1485-92. doi: 10.1111/j.1471-0528.2010.02704.x. Epub 2010 Aug 25
[PubMed PMID: 20735379]
[32]
Caudwell-Hall J, Kamisan Atan I, Martin A, Guzman Rojas R, Langer S, Shek K, Dietz HP. Intrapartum predictors of maternal levator ani injury. Acta obstetricia et gynecologica Scandinavica. 2017 Apr:96(4):426-431. doi: 10.1111/aogs.13103. Epub 2017 Mar 10
[PubMed PMID: 28117880]
[33]
Memon HU, Blomquist JL, Dietz HP, Pierce CB, Weinstein MM, Handa VL. Comparison of levator ani muscle avulsion injury after forceps-assisted and vacuum-assisted vaginal childbirth. Obstetrics and gynecology. 2015 May:125(5):1080-1087. doi: 10.1097/AOG.0000000000000825. Epub
[PubMed PMID: 25932835]
[34]
Shek KL, Pirpiris A, Dietz HP. Does levator avulsion increase urethral mobility? European journal of obstetrics, gynecology, and reproductive biology. 2010 Dec:153(2):215-9. doi: 10.1016/j.ejogrb.2010.07.036. Epub
[PubMed PMID: 20810202]
[35]
DeLancey JO. The pathophysiology of stress urinary incontinence in women and its implications for surgical treatment. World journal of urology. 1997:15(5):268-74
[PubMed PMID: 9372577]
[36]
Snooks SJ,Swash M,Henry MM,Setchell M, Risk factors in childbirth causing damage to the pelvic floor innervation. International journal of colorectal disease. 1986 Jan;
[PubMed PMID: 3598309]
[37]
Parks AG. Royal Society of Medicine, Section of Proctology; Meeting 27 November 1974. President's Address. Anorectal incontinence. Proceedings of the Royal Society of Medicine. 1975 Nov:68(11):681-90
[PubMed PMID: 1197295]
[38]
van Geelen H, Sand PK. The female urethra: urethral function throughout a woman's lifetime. International urogynecology journal. 2023 Jun:34(6):1175-1186. doi: 10.1007/s00192-023-05469-6. Epub 2023 Feb 9
[PubMed PMID: 36757487]
[43]
Sandvik H, Hunskaar S, Vanvik A, Bratt H, Seim A, Hermstad R. Diagnostic classification of female urinary incontinence: an epidemiological survey corrected for validity. Journal of clinical epidemiology. 1995 Mar:48(3):339-43
[PubMed PMID: 7897455]
Level 2 (mid-level) evidence