Continuing Education Activity
Toxic megacolon is a rare, but potentially deadly complication of colonic inflammation. It is defined as a nonobstructive dilation of the colon, which can be total or segmental and is usually associated with systemic toxicity. This activity outlines the evaluation, diagnosis, treatment, and management of toxic megacolon. It also includes essential information about patients at risk for toxic megacolon and when surgical intervention might be necessary. Furthermore, it discusses the role of the interprofessional team in managing and caring for patients with this condition.
Objectives:
- Identify the etiology of toxic megacolon.
- Review the evaluation process for toxic megacolon.
- Outline the treatment and management options available for toxic megacolon.
- Summarize interprofessional team strategies for improving care coordination and communication to advance toxic megacolon and improve outcomes.
Introduction
Toxic megacolon is a rare but potentially deadly complication of colonic inflammation. Its definition is a nonobstructive dilation of the colon, which can be total or segmental and is usually associated with systemic toxicity.[1][2] It is most commonly associated with inflammatory bowel disease, especially ulcerative colitis, yet any condition that leads to inflammation of the colon can potentially cause toxic megacolon.[3]
Etiology
Toxic megacolon can be a potential complication of any disease-causing infectious colitis. The common causes include [2][4]:
Inflammatory Causes
-
Ulcerative colitis
-
Crohn disease
Infectious Causes
Ischemia
Of note, Cytomegalovirus is the leading cause of toxic megacolon in HIV and AIDS patients, especially in those who have disseminated cytomegalovirus.[4] Whereas Entamoeba is the least common cause [2].
Factors that can precipitate toxic megacolon include, but are not limited to [5]:
- Hypokalemia
-
Medications (antimotility agents, opiates, anticholinergics, antidepressants)
-
Barium enema
-
Colonoscopy & bowel preparations
Epidemiology
The incidence of toxic megacolon in the general population is unknown. Toxic megacolon can occur in males and females of all ages. Nevertheless, people at most risk are those with inflammatory bowel disease, especially in the early phase of the disease.[1] Involvement during early disease can be seen more often in Crohn disease before fibrotic colon damage. Once severe fibrosis occurs, the colon cannot dilate.[6][5] However, the incidence in people with inflammatory bowel disease has been a topic of study, and the results are somewhat conflicting; some studies show higher incidence in patients with ulcerative colitis versus Crohn disease (8 to 10% vs. 2.3%), whereas others show higher incidence in Crohn disease (1 to 2.5% vs. 4.4 to 6.3%).[3][2][6]
Clostridium difficile infection can be asymptomatic or can lead to severe disease with toxic megacolon.[7][8][9] Over the past few years, the number of C. difficile colitis related toxic megacolon cases has been increasing. Before 1990 there was an increase from 0.4% to 3%, and after 1990 to 4.3% in proportion to its prevalence.[3][2] Asymptomatic C. difficile infection occurs in about 20% of hospitalized patients, and symptomatic C. difficile infection presents in 1% of hospitalized patients.[5][10][11][12]
Pathophysiology
The pathogenesis of toxic megacolon is not entirely known. Nevertheless, one of the possible mechanisms proposed suggests that mucosal inflammation initiates the process. It releases inflammatory mediators, bacterial products and increases the production of inducible nitric oxide synthase, which in turn increases nitric oxide, and thus causes dilation of the colon. A study showed that patients with toxic megacolon have significantly high levels of inducible nitric oxide synthase in the muscularis propria, which could support this proposed mechanism.[13] Additionally, toxic megacolon leads to inflammation of the smooth muscle of the colon, which causes its paralysis and eventually dilation.[14]
Histopathology
Dilation of the colon, thinning of the colonic wall, and deep ulcers are gross features that toxic megacolon shares with ulcerative colitis and Crohn’s disease. However, the hallmark of toxic megacolon is acute transmural inflammation of the colon with necrosis and granulation tissue, filled with inflammatory cells, such as neutrophils and lymphocytes. The muscle fibers are usually shortened and rounded with collections of eosinophilic cytoplasm.
A key feature that distinguishes toxic megacolon from the neuropathic process is the presence of submucosal and myenteric plexi within the colon.[5]
History and Physical
A thorough history of the patient is critical. Knowing the patient’s medical history ahead of time, HIV/AIDS status, medications, or exposures can help point physicians towards the right diagnosis. It is imperative to review the patient's medication as some (like steroids) can mask the full picture of toxic megacolon, and others can aggravate it (anticholinergics or opioids, for example).[5] Patients presenting with diarrhea and abdominal pain or distension should increase the suspicion index of toxic megacolon.
Patients with a diagnosis of toxic megacolon will look toxic. Those patients are critically ill and usually present with abdominal pain and distention, nausea, vomiting, diarrhea (may or may not be bloody), and altered sensorium. On physical exam, abdominal tenderness and decreased bowel sounds are usually present.[5][11] In a study that focused on patients with C. difficile infection and toxic megacolon, the three most commonly seen complaints were diarrhea, malaise, and abdominal pain/distension.[11]
Comorbidities are frequently seen in those patients, as well. Clinicians can expect to find fluid and electrolyte imbalance, hypotension, anemia, weight loss, uncomplicated diabetes, and renal failure.[15]
Peritonitis symptoms (fever, abdominal pain, tenderness, altered mental status, hypotension) could indicate bowel perforation. Patients who have received steroids may not show this picture as steroids can mask some of those symptoms. Nevertheless, if the patient continues to have a fever for 2 or 3 days while being treated with steroids, the clinician should consider the possibility of a perforated bowel.[2]
Evaluation
The diagnostic basis is the patient’s systemic symptoms and greater than 6 cm dilation of the colon seen on radiographic images.[2] Below are the most commonly used diagnostic criteria for toxic megacolon (by Jalan et al.) [1][2]:
Vital Signs and Laboratory
Vital signs and laboratory results will show fever, tachycardia, anemia, and leukocytosis with a left shift. Increase inflammatory markers, such as erythrocyte sedimentation rate, and C-reactive protein, are also commonly seen. Patients who present with severe diarrhea and volume loss can present with hypokalemia and hypoalbuminemia; this generally indicates poor prognosis.[2]
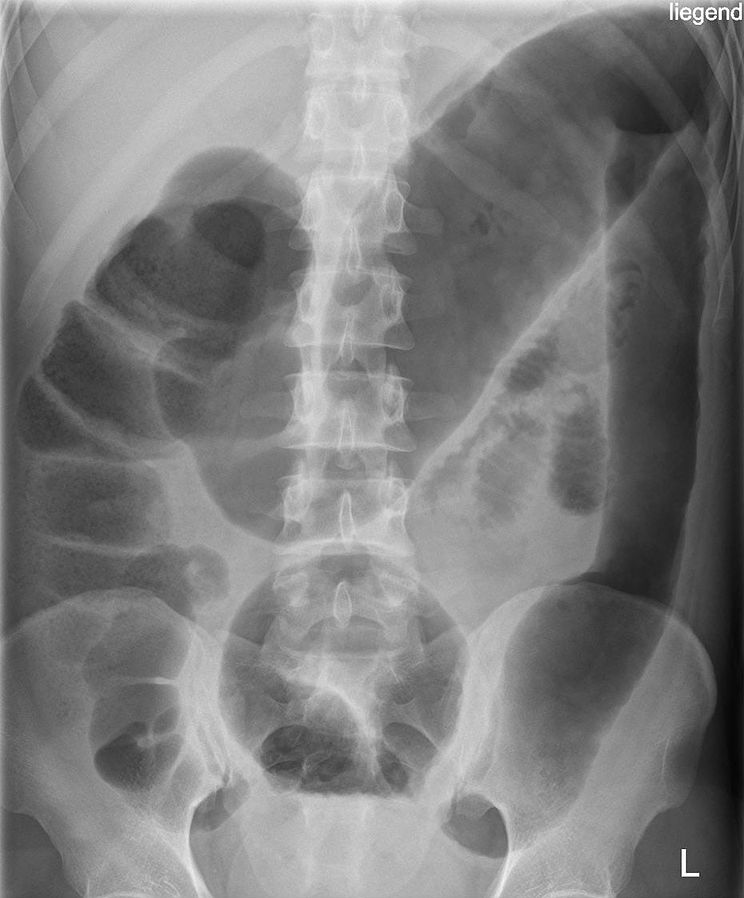
Radiography
Plain abdominal imaging is still the most frequently utilized modality; however, computed tomography (CT) is seeing increasing use, especially because it can provide more reliable information about the severity of the disease. CT is commonly used to assess possible complications of toxic megacolon, which include abscess, perforation, or ascending pylephlebitis.
Key features visible on CT include colonic wall thickening, pericolic stranding, bands of high and low intensity stretching over thickened submucosal folds (accordion sign), and multilayers appearance due to alternating densities of edematous submucosa and hyperemic mucosa (target sign).
An abdominal ultrasound is also an option, but it provides nonspecific findings that might not always help with diagnosis.[16][2]
Colonoscopy
Colonoscopy is not necessary for diagnosis. Therefore, colonoscopy is discouraged due to the high risk of perforation.[2]
Treatment / Management
The treatment focuses on medical management and supportive care to decompress the colon to avoid perforation. The treatment of the underlying cause, correction of any electrolyte disturbances (ex. hypokalemia), symptom management, and prevention of further complications are also important components of a good treatment plan.[15]
Medical Management
Initial treatment involves supportive therapy and medical management. This approach is usually successful in about half of the patients. Patients should obtain admission to the intensive care unit in case of unexpected deterioration. Initially, checking complete blood count, abdominal films, and electrolytes should take place every 12 hours. Once patients improve, images and labs can scale back to once daily. All the medications which can aggravate the megacolon, such as opioids, anticholinergics, etc., should be stopped. Patients should be started on IV fluids to provide adequate hydration.[17] Due to the high risk of perforation, patients are frequently placed on antibiotics, especially if an infectious cause is suspected. The most commonly used antibiotics are metronidazole or vancomycin.[18][19] If cytomegalovirus is the suspected cause, then gancyclovir should be given.[2] Antibiotics of choice for C. difficile are oral vancomycin or oral fidaxomicin. If those are not available, oral metronidazole is an alternative.[7]
Patients with ulcerative colitis should also be given steroids as soon as possible. Generally, the recommendation is hydrocortisone 100 mg over 6 hours (400 mg daily) or methylprednisone 60 mg daily for 5 days. Higher doses did not show significant benefits.[18] Several studies have shown the benefits of using cyclosporine and infliximab in patients with ulcerative colitis. However, those studies did not use patients who presented with toxic megacolon; thus, they are generally not recommended as part of the treatment.[2]
Lastly, patients must be on bowel rest. A nasogastric tube can be inserted to help decompress the stomach, but it will not decompress the colon. As the patient continues to improve, they can gradually start eating to promote gut healing.[2]
Surgical Management
A surgeon should be involved in the patient's care from day 1, in case intervention might be necessary. The current surgical treatment of choice in acute toxic megacolon is subtotal colectomy with ileostomy and either a Hartmann pouch, sigmoidostomy, or rectostomy. Previously there were two additional surgical methods used: total proctocolectomy and the Turnbull method. Turnbull's method was essentially a colon decompression technique that served to prepare a patient for a colectomy. However, studies showed that this method was associated with increased bleeding and high mortality (71%) versus those with subtotal colectomy with ileostomy (8%). Studies conducted with patients treated with total proctocolectomy showed a mortality of 21%.[3][2]
The exact time of surgery in toxic megacolon patients is still unclear. If there is perforation, bleeding, or clinical deterioration of a patient, surgical intervention is unavoidable. Nevertheless, some studies conclude favorable outcomes in patients where surgical intervention is done soon after making the diagnosis of toxic megacolon, whereas other studies show an increase in mortality, especially in patients older than 65.[20] Therefore, surgeons and hospitalists need to work together and assess the patient on a daily basis.[2] This collaboration is essential because colon perforation correlates with a worse prognosis, and it increases mortality by 3 to 5 times.[3][15]
Differential Diagnosis
Differential diagnosis includes [21][2][22]:
- Hirschsprung disease
- Acquired megacolon
- Colonic pseudo-obstruction (Ogilvie syndrome)
- Diffuse gastrointestinal dysmotility
Prognosis
For patients with inflammatory bowel disease, the mortality rates are around 0 to 2%; this is attributable to multiple factors, such as early intervention and better treatment.[23] Colon perforation correlates with a worse prognosis, and it increases mortality by 3 to 5 times.[3][15] However, according to one study, if the patient has surgery earlier, it can decrease the mortality from 22% to 1.2%, whereas other studies show an increase in mortality, especially in patients older than 65.[24][20]
Complications
If toxic megacolon does not receive proper treatment, it has a risk of rupture. Bowel perforation, peritonitis, abscess, and abdominal compartment syndrome are severe complications that warrant immediate surgical intervention.[2]
Deterrence and Patient Education
Although toxic megacolon is a relatively rare disease, patients should receive education about this condition, especially those with inflammatory bowel disease. Since those patients are at an increased risk of developing toxic megacolon, they should understand the precipitating factors as well as potential symptoms. Early diagnosis and treatment can increase the chances of survival.
Enhancing Healthcare Team Outcomes
Toxic megacolon is a medical emergency that demands urgent attention. Failure to recognize the disorder is associated with high mortality and morbidity. Thus, optimal disorder management is best by an interprofessional team. Assistance from a radiologist is vital to make the diagnosis. These patients need ICU care with close monitoring. Nurses should be aware of the potential complications of the disorder and communicate with the surgeon if the patient has signs of peritonitis. Aggressive hydration, replacement of electrolytes, and antibiotics are essential. The pharmacist should check the patient's medication record to ensure that they are on no medications that cause ileus and is on appropriate antibiotics. While most patients do recover with medical therapy, some may require surgery.
The surgical group should be involved early in the process in case initial therapy fails and surgery is unavoidable. High risk of colon perforation and abdominal compartment syndrome are situations where surgery is necessary to avoid further complications.[2] Medical and surgical teams should evaluate patients daily and determine if they would benefit more from surgery than medical management. Surgical and/or gastroenterology specialty-trained nursing staff can assist in the surgery, monitoring the patient (in surgical and non-surgical cases, respectively), and being aware of possible adverse drug effects. They can also check that treatment is trending positively and alert the treating clinician or surgeon of any relapse. Close communication between interprofessional team members is vital if one wants to improve outcomes. Level III
Disclaimer: This research was supported (in whole or part) by HCA Healthcare and/or an HCA Healthcare affiliated entity. The views expressed in this publication represent those of the author(s) and do not necessarily represent the official views of HCA Healthcare or any of its affiliated entities.