[1]
Timmis A, Townsend N, Gale CP, Torbica A, Lettino M, Petersen SE, Mossialos EA, Maggioni AP, Kazakiewicz D, May HT, De Smedt D, Flather M, Zuhlke L, Beltrame JF, Huculeci R, Tavazzi L, Hindricks G, Bax J, Casadei B, Achenbach S, Wright L, Vardas P, European Society of Cardiology. European Society of Cardiology: Cardiovascular Disease Statistics 2019. European heart journal. 2020 Jan 1:41(1):12-85. doi: 10.1093/eurheartj/ehz859. Epub
[PubMed PMID: 31820000]
[2]
Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S, Hindricks G, Kastrati A, Lenzen MJ, Prescott E, Roffi M, Valgimigli M, Varenhorst C, Vranckx P, Widimský P, ESC Scientific Document Group. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). European heart journal. 2018 Jan 7:39(2):119-177. doi: 10.1093/eurheartj/ehx393. Epub
[PubMed PMID: 28886621]
[3]
O'Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Ou N, Radford MJ, Tamis-Holland JE, Tommaso CL, Tracy CM, Woo YJ, Zhao DX. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Journal of the American College of Cardiology. 2013 Jan 29:61(4):e78-e140. doi: 10.1016/j.jacc.2012.11.019. Epub 2012 Dec 17
[PubMed PMID: 23256914]
Level 3 (low-level) evidence
[4]
Byrne RA, Rossello X, Coughlan JJ, Barbato E, Berry C, Chieffo A, Claeys MJ, Dan GA, Dweck MR, Galbraith M, Gilard M, Hinterbuchner L, Jankowska EA, Jüni P, Kimura T, Kunadian V, Leosdottir M, Lorusso R, Pedretti RFE, Rigopoulos AG, Rubini Gimenez M, Thiele H, Vranckx P, Wassmann S, Wenger NK, Ibanez B, ESC Scientific Document Group. 2023 ESC Guidelines for the management of acute coronary syndromes. European heart journal. 2023 Oct 12:44(38):3720-3826. doi: 10.1093/eurheartj/ehad191. Epub
[PubMed PMID: 37622654]
[5]
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, White HD, Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction. Fourth Universal Definition of Myocardial Infarction (2018). Journal of the American College of Cardiology. 2018 Oct 30:72(18):2231-2264. doi: 10.1016/j.jacc.2018.08.1038. Epub 2018 Aug 25
[PubMed PMID: 30153967]
[6]
Vilela EM, Sampaio F, Dias T, Barbosa AR, Primo J, Caeiro D, Fonseca M, Ribeiro VG. A critical electrocardiographic pattern in the age of cardiac biomarkers. Annals of translational medicine. 2018 Apr:6(7):133. doi: 10.21037/atm.2018.02.13. Epub
[PubMed PMID: 29955593]
[7]
Sanaani A, Yandrapalli S, Jolly G, Paudel R, Cooper HA, Aronow WS. Correlation between electrocardiographic changes and coronary findings in patients with acute myocardial infarction and single-vessel disease. Annals of translational medicine. 2017 Sep:5(17):347. doi: 10.21037/atm.2017.06.33. Epub
[PubMed PMID: 28936441]
[8]
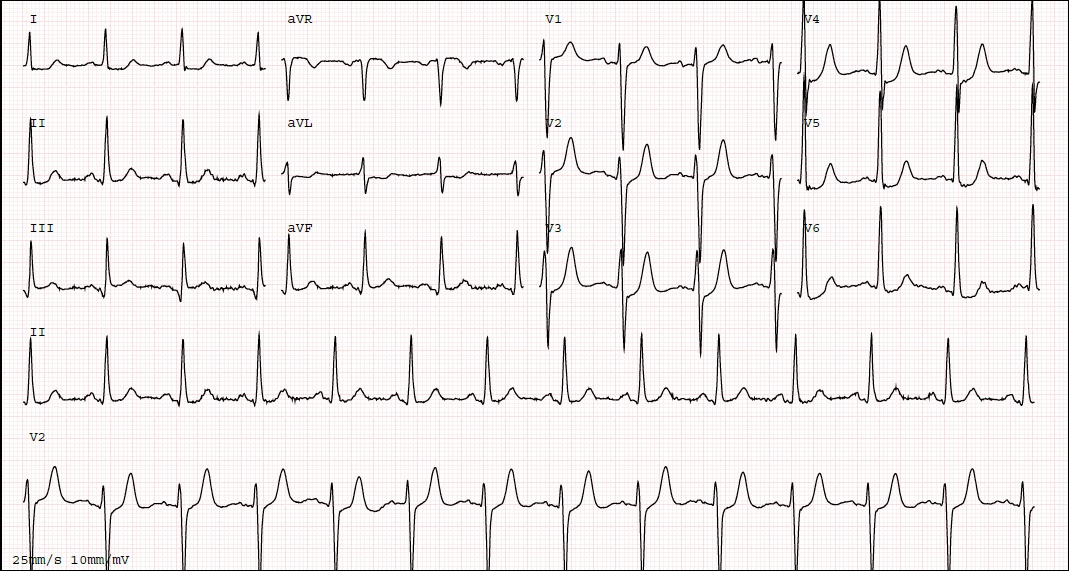
de Winter RJ, Verouden NJ, Wellens HJ, Wilde AA, Interventional Cardiology Group of the Academic Medical Center. A new ECG sign of proximal LAD occlusion. The New England journal of medicine. 2008 Nov 6:359(19):2071-3. doi: 10.1056/NEJMc0804737. Epub
[PubMed PMID: 18987380]
[9]
Morris NP, Body R. The De Winter ECG pattern: morphology and accuracy for diagnosing acute coronary occlusion: systematic review. European journal of emergency medicine : official journal of the European Society for Emergency Medicine. 2017 Aug:24(4):236-242. doi: 10.1097/MEJ.0000000000000463. Epub
[PubMed PMID: 28362646]
Level 1 (high-level) evidence
[10]
de Winter RW, Adams R, Amoroso G, Appelman Y, Ten Brinke L, Huybrechts B, van Exter P, de Winter RJ. Prevalence of junctional ST-depression with tall symmetrical T-waves in a pre-hospital field triage system for STEMI patients. Journal of electrocardiology. 2019 Jan-Feb:52():1-5. doi: 10.1016/j.jelectrocard.2018.10.092. Epub 2018 Oct 18
[PubMed PMID: 30476631]
[11]
Tsutsumi K, Tsukahara K. Is The Diagnosis ST-Segment Elevation or Non-ST-Segment Elevation Myocardial Infarction? Circulation. 2018 Dec 4:138(23):2715-2717. doi: 10.1161/CIRCULATIONAHA.118.037818. Epub
[PubMed PMID: 30571261]
[12]
Chen S, Wang H, Huang L. The presence of De Winter electrocardiogram pattern following elective percutaneous coronary intervention in a patient without coronary artery occlusion: A case report. Medicine. 2020 Jan:99(5):e18656. doi: 10.1097/MD.0000000000018656. Epub
[PubMed PMID: 32000371]
Level 3 (low-level) evidence
[13]
Alahmad Y, Sardar S, Swehli H. De Winter T-wave Electrocardiogram Pattern Due to Thromboembolic Event: A Rare Phenomenon. Heart views : the official journal of the Gulf Heart Association. 2020 Jan-Mar:21(1):40-44. doi: 10.4103/HEARTVIEWS.HEARTVIEWS_90_19. Epub 2020 Jan 23
[PubMed PMID: 32082500]
[14]
Xu J, Wang A, Liu L, Chen Z. The de winter electrocardiogram pattern is a transient electrocardiographic phenomenon that presents at the early stage of ST-segment elevation myocardial infarction. Clinical cardiology. 2018 Sep:41(9):1177-1184. doi: 10.1002/clc.23002. Epub 2018 Sep 22
[PubMed PMID: 29934946]
[15]
Verouden NJ, Koch KT, Peters RJ, Henriques JP, Baan J, van der Schaaf RJ, Vis MM, Tijssen JG, Piek JJ, Wellens HJ, Wilde AA, de Winter RJ. Persistent precordial "hyperacute" T-waves signify proximal left anterior descending artery occlusion. Heart (British Cardiac Society). 2009 Oct:95(20):1701-6. doi: 10.1136/hrt.2009.174557. Epub 2009 Jul 19
[PubMed PMID: 19620137]
[16]
Vilela EM, Caeiro D, Primo J, Braga P. A pivotal electrocardiographic presentation: reading between the lines. The Netherlands journal of medicine. 2019 Oct:77(8):297
[PubMed PMID: 31814579]
[17]
Gorgels AP. Explanation for the electrocardiogram in subendocardial ischemia of the anterior wall of the left ventricle. Journal of electrocardiology. 2009 May-Jun:42(3):248-9. doi: 10.1016/j.jelectrocard.2009.01.002. Epub 2009 Mar 5
[PubMed PMID: 19264324]
[18]
Zorzi A, Perazzolo Marra M, Migliore F, Tarantini G, Iliceto S, Corrado D. Interpretation of acute myocardial infarction with persistent 'hyperacute T waves' by cardiac magnetic resonance. European heart journal. Acute cardiovascular care. 2012 Dec:1(4):344-8. doi: 10.1177/2048872612466537. Epub
[PubMed PMID: 24062926]
[19]
de Winter RW, Adams R, Verouden NJ, de Winter RJ. Precordial junctional ST-segment depression with tall symmetric T-waves signifying proximal LAD occlusion, case reports of STEMI equivalence. Journal of electrocardiology. 2016 Jan-Feb:49(1):76-80. doi: 10.1016/j.jelectrocard.2015.10.005. Epub 2015 Oct 13
[PubMed PMID: 26560436]
Level 3 (low-level) evidence
[20]
Hashmi KA, Adnan F, Ahmed O, Yaqeen SR, Ali J, Irfan M, Edhi MM, Hashmi AA. Risk Assessment of Patients After ST-Segment Elevation Myocardial Infarction by Killip Classification: An Institutional Experience. Cureus. 2020 Dec 21:12(12):e12209. doi: 10.7759/cureus.12209. Epub 2020 Dec 21
[PubMed PMID: 33489617]
[21]
Fiol Sala M, Bayés de Luna A, Carrillo López A, García-Niebla J. The "De Winter Pattern" Can Progress to ST-segment Elevation Acute Coronary Syndrome. Revista espanola de cardiologia (English ed.). 2015 Nov:68(11):1042-3. doi: 10.1016/j.rec.2015.07.006. Epub 2015 Sep 24
[PubMed PMID: 26410027]
[22]
Carrington M, Santos AR, Picarra BC, Pais JA. De Winter pattern: a forgotten pattern of acute LAD artery occlusion. BMJ case reports. 2018 Nov 8:2018():. pii: bcr-2018-226413. doi: 10.1136/bcr-2018-226413. Epub 2018 Nov 8
[PubMed PMID: 30413454]
Level 3 (low-level) evidence
[23]
Levis JT. ECG Diagnosis: Hyperacute T Waves. The Permanente journal. 2015 Summer:19(3):79. doi: 10.7812/TPP/14-243. Epub
[PubMed PMID: 26176573]
[24]
Galli M, Andreotti F, Sabouret P, Gragnano F. 2023 ESC Guidelines on ACS: what is new in antithrombotic therapy? European heart journal. Cardiovascular pharmacotherapy. 2023 Nov 2:9(7):595-596. doi: 10.1093/ehjcvp/pvad065. Epub
[PubMed PMID: 37738449]
[25]
Rafique Z, Chouihed T, Mebazaa A, Frank Peacock W. Current treatment and unmet needs of hyperkalaemia in the emergency department. European heart journal supplements : journal of the European Society of Cardiology. 2019 Feb:21(Suppl A):A12-A19. doi: 10.1093/eurheartj/suy029. Epub 2019 Feb 26
[PubMed PMID: 30837800]
[26]
Kontos MC, Gunderson MR, Zegre-Hemsey JK, Lange DC, French WJ, Henry TD, McCarthy JJ, Corbett C, Jacobs AK, Jollis JG, Manoukian SV, Suter RE, Travis DT, Garvey JL. Prehospital Activation of Hospital Resources (PreAct) ST-Segment-Elevation Myocardial Infarction (STEMI): A Standardized Approach to Prehospital Activation and Direct to the Catheterization Laboratory for STEMI Recommendations From the American Heart Association's Mission: Lifeline Program. Journal of the American Heart Association. 2020 Jan 21:9(2):e011963. doi: 10.1161/JAHA.119.011963. Epub 2020 Jan 20
[PubMed PMID: 31957530]