Continuing Education Activity
This activity for healthcare professionals delves into the intricate aspects of lateral collateral ligament (LCL) knee injuries, thoroughly exploring their anatomy, evaluation, and treatment modalities. As a crucial knee joint stabilizer, the LCL's role in preventing excess varus stress and posterolateral rotation is pivotal. The course begins with an in-depth anatomical examination detailing the LCL's origin on the lateral femoral epicondyle and its insertion on the fibular head. Participants gain insights into the LCL's unique characteristics, distinguishing it from the medial collateral ligament, focusing on its cord-like structure and absence of meniscal or joint capsule attachment.
Moving beyond anatomy, this activity explores the LCL's biomechanics, elucidating the ligament's primary role in stabilizing varus stress across various knee flexion angles. Participants also gain a nuanced understanding of the LCL's contribution to posterolateral stability and restraint of external tibial and knee rotation. This activity equips healthcare professionals with the knowledge necessary to evaluate and manage LCL knee injuries effectively. The interdisciplinary nature of care is emphasized, highlighting the collaborative efforts of an interprofessional team in optimizing patient outcomes.
Objectives:
Identify the signs and symptoms suggestive of a lateral collateral ligament injury.
Create appropriate evaluation strategies for suspected lateral collateral ligament injuries.
Compare the management options available for lateral collateral ligament knee injuries.
Develop effective interprofessional collaborative strategies when determining short- and long-term treatment plans for patients with lateral collateral ligament injuries.
Introduction
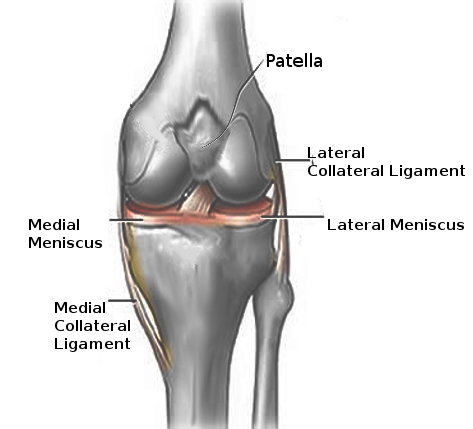
The lateral collateral ligament (LCL), also known as the fibular ligament, is one of the knee joint's key stabilizers (see Image. Left Knee Ligaments). This fibrous structure originates from the lateral femoral epicondyle and inserts on the fibular head. The LCL is part of the knee's "posterolateral corner" (PLC) along with the biceps femoris tendon and fibular collateral, fabellofibular, popliteofibular (PFL), and arcuate ligaments, though this region's anatomy is variable. The LCL primarily prevents excess varus stress and posterolateral knee rotation. LCL and PLC injuries are the least frequent of all knee injuries but still warrant high suspicion during knee exams.
Anatomy
The LCL's origin is located 1.4 mm proximal and 3.1 mm posterior to the lateral epicondyle of the femur. The LCL inserts anteriorly on the fibular head, 28.4 mm distal to the fibular styloid tip, covering nearly 38% of the fibular head.[1] The common fibular nerve innervates the LCL. The ligament's blood supply arises from the popliteal artery, primarily from the anterior tibial recurrent arteries and branches of the superior and inferior lateral genicular arteries.[2][3]
Unlike the MCL, which is fan-like, the LCL has a cord-like shape. Additionally, the LCL lacks the meniscal and joint capsule attachments the MCL has. The LCL has a thickness of 2 to 3 mm, a width of 4 to 5 mm, and a length of 69.9 mm.[4]
Deep to the LCL lies the popliteus tendon (PLT), which originates 18.5 mm anterior and distal to the LCL and measures 55 mm long on average. Superficial to the LCL is the superficial layer of the iliotibial band (ITB), which inserts along the knee's anterolateral portion at Gerdy's tubercle.[5] However, the LCL is exposed in its distal quarter anteriorly and laterally in a location often serving as a surgical entry window.
Biomechanics
The LCL is the primary stabilizer of varus stress in all degrees of knee flexion, with the PLT, ITB, cruciate ligaments, and biceps and lateral gastrocnemius tendons acting as secondary varus stabilizers.[6][7] The LCL combines with the fabellofibular, popliteofibular, and arcuate ligaments to become the static PLC stabilizer. The LCL also secures the knee posterolaterally, preventing medial tibial translation.[8]
The LCL helps restrain external tibial rotation and posterior tibial displacement in 0° to 30° of knee flexion. Typically, the PFL resists external tibial rotation as knee flexion increases past 60°. Beyond 60° of flexion, the LCL contributes to limiting knee external rotation but to a lesser degree than the PFL.[9]
Studies show that the LCL and PLC structures play minor roles in stabilizing anterior and posterior tibial translation when the cruciate ligaments are torn.[10]
Etiology
The most common LCL injury mechanism is a high-energy blow to the anteromedial knee, combining hyperextension and extreme varus force.[1] Noncontact hyperextension and varus stressors have also been reported to cause LCL injuries.
Epidemiology
Frequency of LCL Injuries
Due to this ligament's close association with the PLC and posterior (PCL) and anterior (ACL) cruciate ligaments, the LCL is injured in isolation in less than 2% of knee injury cases. However, this ligament is damaged alongside other structures in 7% to 16% of all knee ligamentous injuries. Studies show that isolated LCL injury is the second least common knee injury in high school athletes, with an incidence of 7.9%. PCL injuries are the least common at 2.4%.[11] Contact sports cause 40% of PLC and LCL injuries. Other possible causes of LCL damage are non-sports-related trauma, such as motor vehicular crashes and falls.
Risk Factors
Although there have been few studies completed on isolated LCL injuries, reports show that the female gender, high-contact sports, and athletic activities requiring high-velocity pivoting and jumping increase the likelihood of injury. Soccer is the most likely to cause knee injury overall, but tennis and gymnastics are the most specific for isolated LCL injuries. A United States military study has shown that prior knee, ankle, or hip injury predisposes soldiers to increased lateral knee injury rates.[12]
History and Physical
History
Patients often present with a history of an acute medial blow to the fully extended knee or extreme noncontact-varus bending. Sudden lateral knee pain, swelling, and ecchymosis usually occur postinjury. The patient may also describe a thrust gait or the ipsilateral foot kicking in midstance.[13] Patients may complain of lateral lower extremity paresthesias and weakness or a foot drop.
A complete personal medical history must be obtained, including but not limited to clotting disorders, previous surgeries, occupation, gait, ambulation-assisted device use, and living situations, such as stair-climbing at home.
Physical Exam
A comprehensive full range-of-motion knee exam is crucial for all patients. The most common exam finding is lateral knee tenderness on palpation. Pain may also be evident along the infrapatellar bursa, Gerdy's tubercle, and the patellar tendon attachment. Ecchymosis, swelling, and warmth may be present. Gait should be examined for the classical "varus thrust" finding.
Special Testing
Special tests help localize the damage and rule out other conditions. The results of these tests can aid in the accurate diagnosis and localization of PLC injuries when performed in conjunction with thorough history-taking and appropriate imaging studies.
Varus stress test
Studies show this is the most helpful test for assessing LCL injury. The test is performed with the examiner's hand stabilizing the femur and monitoring the lateral joint line while placing a varus force on the ankle. The test is first performed at 30°. Any lateral-compartment gaping is a positive indicator of LCL and potential PLC injury.
The test is then done in full knee extension. Improved stability on knee extension signifies an isolated LCL injury. However, the persistence of instability in full knee extension indicates injuries to both the LCL and PLC.[14]
External rotation recurvatum test
This test assesses the knee's posterolateral rotary stability. The patient lies in the supine position. The examiner then places a downward force through the suprapatellar region while lifting the big toe off the table and externally rotating the tibia with the other hand. Excess hyperextension compared to the uninjured knee is a positive exam result and indicates an LCL injury. Notably, this exam is less than 10% accurate in identifying PLC injuries but more reliable in diagnosing associated ACL injuries.
Posterolateral drawer test
Like the posterior drawer test, the patient lies prone with the knee flexed to 90° and externally rotated by 15°. The examiner grips the femoral condyles and directs a posterior force on the knee. Any excess posterolateral translation on the injured leg suggests a PLC injury.[15]
Reverse pivot shift
This test is performed in the same position as the posterolateral drawer test. The examiner monitors the lateral joint line and slowly extends the knee while applying a valgus and external rotating force to the joint. At 30°, the ITB transitions from a flexion to an extension vector, reducing the previously subluxated lateral tibial plateau at 90°. The test is positive if an audible click is heard at 30°, indicating the presence of posterolateral rotatory instability from combined ACL and PCL injuries. Results must be compared bilaterally, as a large percentage of noninjured knees may show false-positive results.[16][17]
Dial test
This test assesses external femoral rotation and is useful in confirming PLC injury. The patient lies prone. The examiner then stabilizes the thigh with one hand and uses the other hand to rotate the ankle and leg externally. This test is performed bilaterally at 30° and 90° knee flexion. External rotation on the injured leg of 10° or more confirms PLC injury.[18][19][20][21]
Knee examinations should be thorough and include all articular structures to avoid missing associated ligamentous, meniscal, or soft tissue injuries, which are highly likely in trauma cases. Anterior and posterior drawer tests are necessary to rule out possible ACL or PCL injuries. Patellar assessment helps detect accompanying subluxation or dislocation.
Evaluation
Plain Radiography
Plain anteroposterior and lateral knee radiographs will not reveal any LCL changes. However, x-rays are necessary to rule out associated structural injuries. Frequently seen radiographical changes include fibular head fractures or avulsions (arcuate sign), tibial spine avulsions, and lateral tibial plateau (Segond fracture). The arcuate sign and Segond fracture are pathognomonic for PLC injury, warranting further workup for LCL injury. Plain radiographs can help rule out underlying arthritic changes in older individuals with chronic lateral knee pain.
Varus and kneeling posterior-stress radiographs are also necessary. Both can show LCL and PLC injury severity and have high user reliability.[22]
Magnetic Resonance Imaging
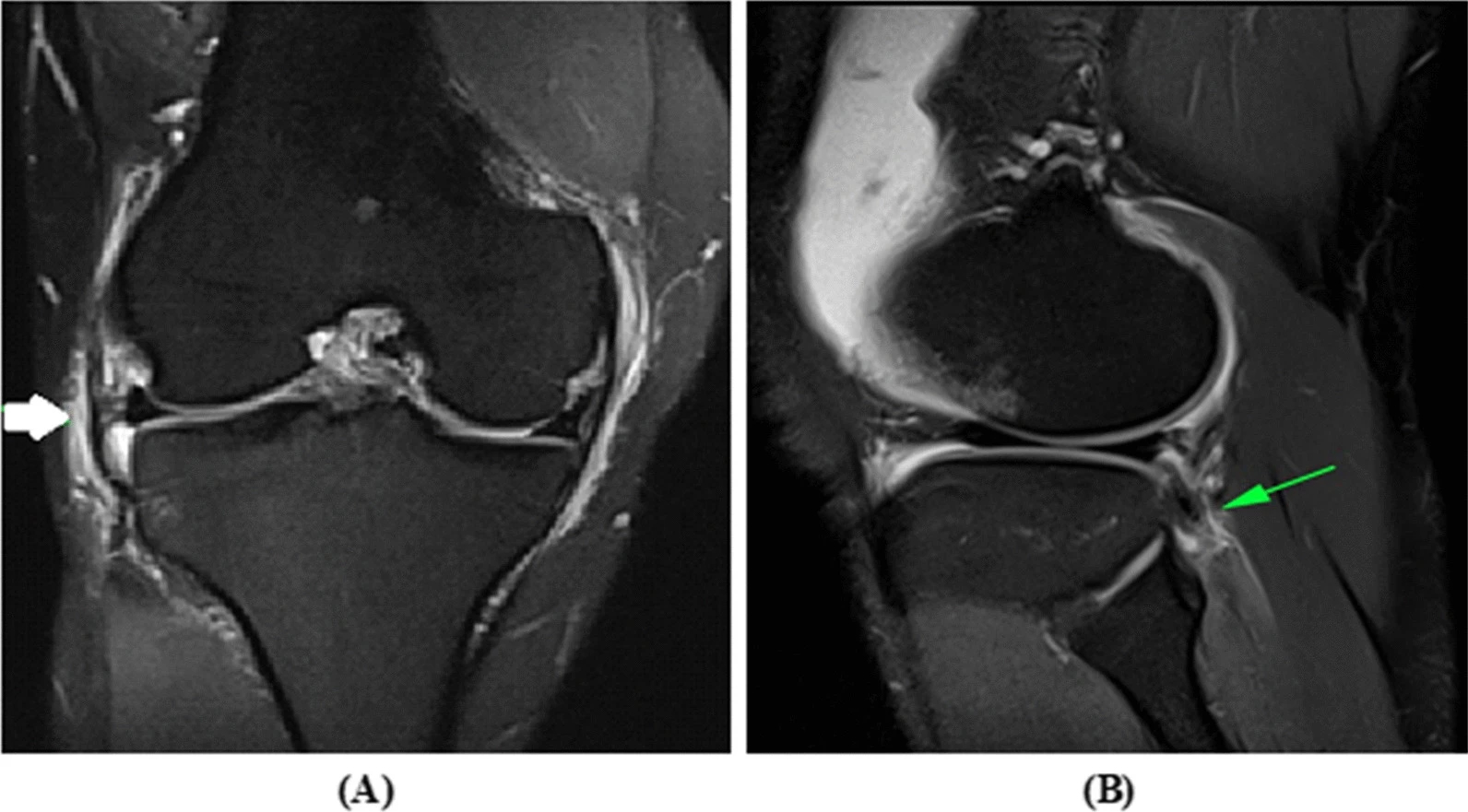
Magnetic resonance imaging (MRI) is the gold standard for diagnosing structural LCL and PLC injuries (see Image. Lateral Collateral Ligament and Popliteotendinous Complex Injuries on MRI). Coronal and sagittal T1- and T2-weighted series have the highest sensitivity and specificity for LCL injury at approximately 90%. However, MRI findings alone are insufficient to determine the need for surgery, as radiographs and proper physical examination are still required.[23][24]
Musculoskeletal ultrasound can help quickly identify LCL injuries. Damage signs include LCL thickening and hypoechogenicity. A complete tear may show edema, dynamic laxity, or lack of LCL fiber continuity.
Classification of LCL Injuries
LCL injuries are classified into 3 grades depending on severity.
- Grade 1 or a mild sprain is diagnosed in the presence of localized lateral knee tenderness. No instability or mechanical symptoms are present.
- Grade 2 or a partial tear is diagnosed in the presence of severe, localized lateral and posterolateral knee pain and swelling. The ligament has a fixed endpoint, but 5 to 10 mm of laxity may be observed.
- Grade 3 or a complete tear causes variable pain and swelling. This condition usually involves the PLC and neighboring structures. Mechanical symptoms and more than 10 mm of laxity are noted.
LCL injury grading is a significant consideration when determining the appropriate treatment strategy.
Treatment / Management
LCL tears do not self-heal, as opposed to MCL tears. Thus, surgeons should have a low threshold for operative management of these injuries. LCL injury grading and damage to other knee structures are critical determinants of the need for surgical management. Early operative management is favorable in the presence of concomitant knee injuries.[25]
Acute Management of LCL Tears
Acute management involves rest, compression, intake of nonsteroidal anti-inflammatory drugs (NSAIDs), and ice. Ice should not be applied for longer than 15 minutes at a time to the lateral knee to avoid cold injury to the common peroneal nerve.
Conservative Management of LCL Tears
Nonoperative management is indicated for isolated grade 1 or 2 injuries with no instability at 0°.[26][27] Patients should be non-weight-bearing and use crutches for 1 week for better pain control. The patient should be placed in a hinged knee brace for 3 to 6 weeks to stabilize the knee medially and laterally during functional rehabilitation. Limited immobilization and early progressive rehabilitation are key to recovery. Patients usually return to sports in 6 to 8 weeks. The affected knee must be assessed thoroughly during follow-up to avoid missing PLC injuries that may result in progressive varus and hyperextension laxity.
Bushnell et al reported a rapid return to play at the professional level following nonoperative management of MRI-documented isolated grade 3 LCL injuries in national football league athletes.[28] However, operative management remains the standard of care in most grade 3 LCL tears.
Surgical repair is indicated for an isolated acute (ie, ≤ 2 weeks postinjury) grade 3 LCL tear with an avulsed ligament from its attachment site when anatomic reduction with full knee extension is achievable. The technique involves a mid-ITB lateral incision, common peroneal nerve dissection, biceps femoris bursal incision, LCL identification, and ligamentous reapproximation with a stay suture. Primary repair achievability and integrity of the LCL's proximal femoral origin are assessed afterward.[29] The ITB is then dissected proximally from the lateral epicondyle and distally from Gerdy's tubercle. If the femoral attachment is avulsed, a suture anchor is used to reattach the LCL to the femoral footprint. A high failure rate of up to 40% has been reported with surgical LCL repair.[30]
Surgical reconstruction of isolated grade 3 LCL tears is indicated in subacute or chronic cases (ie, >2 weeks since injury) or acute complete midsubstance tears. These conditions often have persistent varus instability.[31] Another indication is acute LCL avulsion with unachievable anatomic reduction, as in cases of significant trauma to surrounding structures. Concomitant knee injuries should be managed during the same reconstruction procedure.[32]
LCL Reconstruction Approaches
LCL reconstruction approaches are classified as either isometric, nonanatomic, or anatomic. The choice between nonanatomic, isometric, and anatomic reconstruction depends on various factors, including the injury's specific characteristics, the patient's functional requirements, and the surgeon's expertise.
Isometric tenodesis
As per the Clancy technique, isometric tenodesis (biceps femoris tenodesis) is performed through posterolateral knee incision, with a hole drilled just anterior to the LCL's femoral attachment. A 6.5 mm screw with a spiked washer is inserted until 0.5 inches is prominent.[33] The biceps tendon is moved to a position anteromedial to the ITB through a split in the posterior intermuscular septum.
The knee is flexed to 90°. With gradual knee extension, the tendon is then levered over the screw post. On reaching full extension, the screw with the washer is secured. The ITB is then closed. The range of motion should be serially assessed during the procedure to detect any tendon subluxation or ITB snapping.
Isometric LCL reconstruction
A nonanatomic technique was described using patellar tendon allograft. The proximal fibula is cleared of all soft tissues. A tunnel is then drilled and gradually enlarged with reaming. The femur is exposed through a midline incision in the ITB, and a tunnel is drilled 6 mm anterior to the center of the LCL femoral insertion. The tunnel should be directed proximal and anterior to the medial femoral epicondyle. The surgeon can confirm isometry using a small K-wire and a looped suture.
The graft is fashioned and secured to the fibula with an interference screw and then passed through the femoral tunnel. The graft should be tensioned with the knee in 20° to 30° of flexion and valgus stress applied, then fixed with another interference screw. Several other isometric LCL reconstruction techniques have been reported in the literature with various grafts, such as the Achilles tendon graft.[34]
Anatomic LCL reconstruction
Isolated reconstruction using a semitendinosus graft was reported to reinstitute precise knee biomechanics and was validated in a biomechanical study. Laprade described the anatomic approach using a semitendinosus graft.[35]
A tunnel is drilled at the site of fibular LCL insertion. Then, another tunnel is drilled at the femoral attachment site through a split in the ITB. With 20° of knee flexion and valgus stress applied, the graft is secured into both tunnels with an interference screw. The graft is then assessed for verification of function and secured fixation. Finally, the graft is sutured to itself for an augmented fixation.
Differential Diagnosis
Lateral knee injuries should be examined closely due to their many differentials, including the following:
- ACL and PCL tears are often confused with LCL injury due to shared nonspecific features like swelling, acute-onset pain, and knee instability. The anterior or posterior drawer tests should help differentiate the injuries.
- Lateral meniscus tears are often mistaken for an LCL tear due to their common nonspecific features, such as swelling, bucking, and lateral joint line pain. A positive McMurray test, which is not seen in LCL tears, can differentiate a lateral meniscus tear.
- Popliteal injury, specifically tendinopathy, commonly presents as posterolateral knee pain distal to lateral femoral epicondyle worsened by downhill walking. A positive Garrick test can help determine the source of popliteal pain. This test is performed by flexing the knee and externally rotating the tibia as the patient resists. Pain is absent in LCL injury with this maneuver.
- Bone contusion may present as LCL tears. Palpating the lateral joint line and stressing the knee can help detect the contusion. Varus stress will not affect lateral bone contusion pain.
- ITB syndrome presents with chronically developing pain at the lateral distal femoral epicondyle. Pain should not be reproducible via varus stress.
A thorough clinical examination and appropriate imaging can help distinguish these conditions from LCL tears.
Prognosis
Depending on the severity, LCL injuries are manageable operatively or nonoperatively. The prognosis for LCL and PLC injuries is good with appropriate treatment. However, recovery from high-grade injuries may exceed 4 months.[36][37]
Complications
Undiagnosed LCL and PLC injuries often have long-term complications, the most common being knee instability and chronic pain. Reports also show that approximately 35% of PLC injuries have an associated peroneal nerve palsy, likely due to the nerve's proximity to the LCL. Patients may develop long-term foot drop, lower extremity weakness, and decreased sensation on the dorsal and lateral foot surfaces. Meanwhile, common postoperative complications in patients treated with surgical intervention include hardware irritation and stiffness.
Postoperative and Rehabilitation Care
Healing and protecting the ligaments are vital in all grades of injury. Recommendations include the following:
- For Grades 1 and 2 LCL injuries: Passive and active prone-knee flexion should be initiated in the immediate weeks following injury to help prevent stiffness or contracture. The hinged knee brace is removed around 6 weeks postinjury. The patient may begin physical therapy at this time. Patients may return to sports only when the range of motion is full, knee motion is painless, and ligamentous laxity and lateral knee tenderness have completely resolved. A safe return to sports can be achieved at approximately 4 weeks for grade 1 and 10 weeks for grade 2 injuries.
- For Grade 3 LCL injuries: Patients should be non-weight-bearing in a knee immobilizer for 6 weeks after surgical interventions. As in grade 1 and 2 injuries, quadriceps strengthening is imperative throughout recovery. Hamstring strengthening should be avoided for at least 4 months to prevent LCL reconstruction damage. Sport-specific therapy may commence after 4 months postoperatively.
Overall, a structured and progressive rehabilitation program tailored to the patient's needs and goals is essential for successful recovery following LCL treatment.
Deterrence and Patient Education
Preventing LCL injuries involves a combination of strategies to reduce the risk of knee trauma and enhance the joint's stability. Patients must be educated about the following measures:
- Incorporating a comprehensive strength and conditioning program that targets the muscles surrounding the knee joint. Strong muscles provide better knee support and stability, reducing the risk of ligament injuries.
- Maintaining good flexibility and mobility in the lower extremities to help improve knee range of motion and reduce the risk of muscle imbalances
- Performing proper warm-up exercises before engaging in physical activity or sports to prepare the muscles and joints for activity
- Practicing proper techniques for physical activities. Correct biomechanics help reduce excessive stress on the knee joint and ligaments, decreasing the risk of injury.
- Wearing the appropriate footwear for specific activities to help stabilize the foot and ankle complex
- Using protective gear, such as knee supports and braces, during high-risk activities or sports
- Avoiding dangerous behaviors that increase the risk of musculoskeletal trauma
The risk of LCL injuries can be minimized by implementing these preventive strategies.
Pearls and Other Issues
LCL injuries often occur due to a direct blow to the inside of the knee or from a force that pushes the knee outward, leading to excessive varus stress. Patients with LCL injuries may present with pain, swelling, and tenderness over the lateral knee joint. Knee instability may also be reported, especially with varus stress testing. Specific tests, such as varus stress, dial, and reverse pivot shift tests, can help assess the integrity and stability of the LCL and other PLC structures.
Knee MRI is the preferred imaging modality for evaluating knee injuries. MRI can provide valuable information about the extent of knee injury. Radiography can rule out concomitant injuries, such as fractures. Clinical examination and imaging findings, allowing proper LCL injury severity assessment, are the most important factors influencing the decision to treat surgically.
Grade 1 and some grade 2 LCL injuries may be managed conservatively. Surgical intervention may be considered for Grade 3 LCL tears, multiligamentous knee injuries, chronic instability, or failure of conservative management in low-grade injuries. Surgical approaches include isometric, nonanatomic, and anatomic techniques. A structured posttreatment rehabilitation program tailored to the patient's needs is essential for successful outcomes.
Enhancing Healthcare Team Outcomes
An interprofessional team that includes an emergency medicine physician, orthopedic surgeon, physical therapist, and orthopedic nurses is essential in diagnosing and managing LCL injuries. The emergency medicine physician provides the initial assessment and management of LCL injuries, particularly in the acute setting. The orthopedic surgeon specializes in evaluating and treating LCL injuries. These practitioners may prescribe conservative treatments for low-grade injuries or perform LCL repair or reconstruction in complex cases.
The physical therapist guides patients through therapeutic exercises, functional training, and manual therapy techniques to facilitate recovery and return to preinjury activities. Orthopedic nurses can assist the surgeon during procedures. In the wards, these professionals assist with patient education, wound care, pain management, and administration of medications as prescribed by the healthcare team. Orthopedic nurses play a crucial role in coordinating care, providing emotional support, and advocating for patients' needs throughout their treatment journey.
All interprofessional team members must maintain open communication channels as the patient progresses through treatment. Collaboration among team members ensures comprehensive care, individualized treatment plans, and optimal patient outcomes.