Definition/Introduction
The major drive for respiration originates in the central and peripheral chemoreceptors. The central chemoreceptors are located anterior medulla in the brainstem and predominantly responds to a decrease in pH from the accumulation of carbon dioxide in the cerebral spinal fluid. The blood-brain barrier protects the central nervous system from external stimuli. Carbon dioxide is lipid-soluble, which allows it to quickly diffuse across the protective barrier and influence the respiratory drive.
Unlike the central chemoreceptors, the peripheral chemoreceptors are more sensitive to changes in oxygen levels. The peripheral chemoreceptors consist of the carotid and aortic bodies. The aortic bodies are located at the aortic arch while the carotid bodies are situated at the common carotid artery bifurcation. Hypoxia stimulates cranial nerve IX to send signals to the nucleus tractus solarius which triggers ventilation. However, the central chemoreceptors normally override the peripheral receptors as it originates from the central control system of the body.[1]
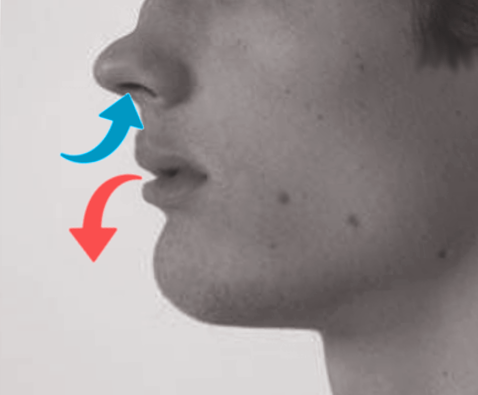
Purse-lip breathing is a technique that allows people to control their oxygenation and ventilation. The technique requires a person to inspire through the nose and exhale through the mouth at a slow controlled flow. The expiratory phase of respiration is going to prolonge when compared to inspiration to expiration ratio in normal breathing. The maneuver presents as a controlled breath directed through the nostril then exhalation directed through lips having a puckered or pursed appearance. This technique creates a back pressure producing a small amount of positive end-expiratory pressure (PEEP).
During exhalation, the forces cause the airways that lack cartilage to drag inward towards the lumen obstructing airflow by increasing airway resistance which could lead to carbon dioxide trapping.[2] When there is an increased in carbon dioxide levels the central chemoreceptors are triggered to immediately increase the rate of respiration in an attempt to bring the body’s pH back to a baseline range of roughly 7.4 in a normal individual.[3][4] While the increase in the rate of respiration is effective in clearing carbon dioxide, it can potentially cause more air trapping and fatigue of the respiratory muscles.[5] PEEP mitigates the increase in work by creating an artificial splint that supports the patency of the airways and alveoli, increasing surface area and recruiting more alveoli to participate in gas exchange.[6]
The positive pressure created opposes the forces exerted on the airways from the flow of exhalation. As a result, pursed-lip breathing helps support breathing by the opening of the airways during exhalation and increasing excretion of volatile acids in the form of carbon dioxide preventing or relieving hypercapnia. Through purse-lip breathing, people can have relief of shortness of breath, decrease the work of breathing, and improve gas exchange. They also regain a sense of control over their breathing while simultaneously increasing their relaxation.