Continuing Education Activity
As the most common cause of clinic visits due to nerve entrapment, carpal tunnel syndrome affects a significant portion of the population. Often, history and physical exam may be inadequate to evaluate the severity fully or to confirm the diagnosis. This activity describes the invaluable electrodiagnostic findings of nerve conduction tests and needle electromyography studies and highlights the role of the interprofessional team in evaluating patients with carpal tunnel syndrome.
Objectives:
- Identify the indications for electrodiagnostic testing in patients suspected of carpal tunnel syndrome.
- Describe the nerve conduction study findings in a patient with carpal tunnel syndrome.
- Review the electromyographic findings in a patient with carpal tunnel syndrome.
- Outline the importance of communication among the interprofessional team to enhance the delivery of care for patients with carpal tunnel syndrome.
Introduction
Carpal tunnel syndrome (CTS) accounts for approximately 90% of all focal entrapment neuropathy, making it a frequent electrodiagnostic consultation. It is present in about 3.8% of the general population. It is more common in women than in men, and while it occurs in all age groups, incidence generally reaches a peak within the age of 40 to 60 years.[1] Hypothyroidism, diabetes mellitus, rheumatoid arthritis, gout, peripheral edema, acromegaly, tumors, trauma, and pregnancy are risk factors that predispose patients to develop CTS. Furthermore, patients whose occupations rely on the hands' repetitive movements and those with forceful hand movements are also prone to developing CTS.[2]
The clinical presentation typically reveals numbness, weakness, and paresthesias within the thumb, index, middle, and radial side of the ring finger.[3] The thenar area has normal sensation as the palmar cutaneous sensory branch innervates it, which does not pass through the carpal tunnel. However, the recurrent thenar motor branch does pass through the carpal tunnel and gives innervation to the opponens pollicis, abductor pollicis brevis, and superficial head of the flexor pollicis brevis. Patients' symptoms tend to worsen at night or during the hand's repetitive movements, especially those requiring prolonged wrist flexion.[2]
Depending on the severity of the patient's symptoms, they can categorize into three stages. Stage 1 presents with frequent awakenings at night due to tingling in their hands and fingers, which may last through the morning with associated stiffness. Stage 2 shows symptoms that are also present during the day. Motor deficits may also be apparent with patients reporting dropping objects from their hands. Stage 3, the final stage, demonstrates atrophy of the thenar muscles and may respond poorly to surgical decompression.[1]
Anatomy and Physiology
The carpal tunnel is a defined space with a bony canal containing nine tendons (flexor digitorum superficialis, flexor digitorum profundus, flexor pollicis longus) and the median nerve. The carpal bones border the dorsal surface, and the volar surface is the transverse carpal ligament (flexor retinaculum). Sensory branches of the median nerve supply innervation to the first three and a half fingers.[1][2] When the space within the tunnel becomes restricted, the nerve can become compressed, leading to CTS symptoms and signs. Sensory fibers are usually affected first before the motor fibers. Several mechanisms appear to contribute to the development of CTS.[1]
- Prolonged compression can cause nerve injury through demyelination.
- Injury to the nerve through persistent scarring of the outer layer (mesoneurium) leads to fibrosis.
- Abnormalities in synovial tissue increase the canal's volume and cause pressure over the median nerve.
- Inflammation results from increased expression of prostaglandin E2 and vascular endothelial growth factor.
Indications
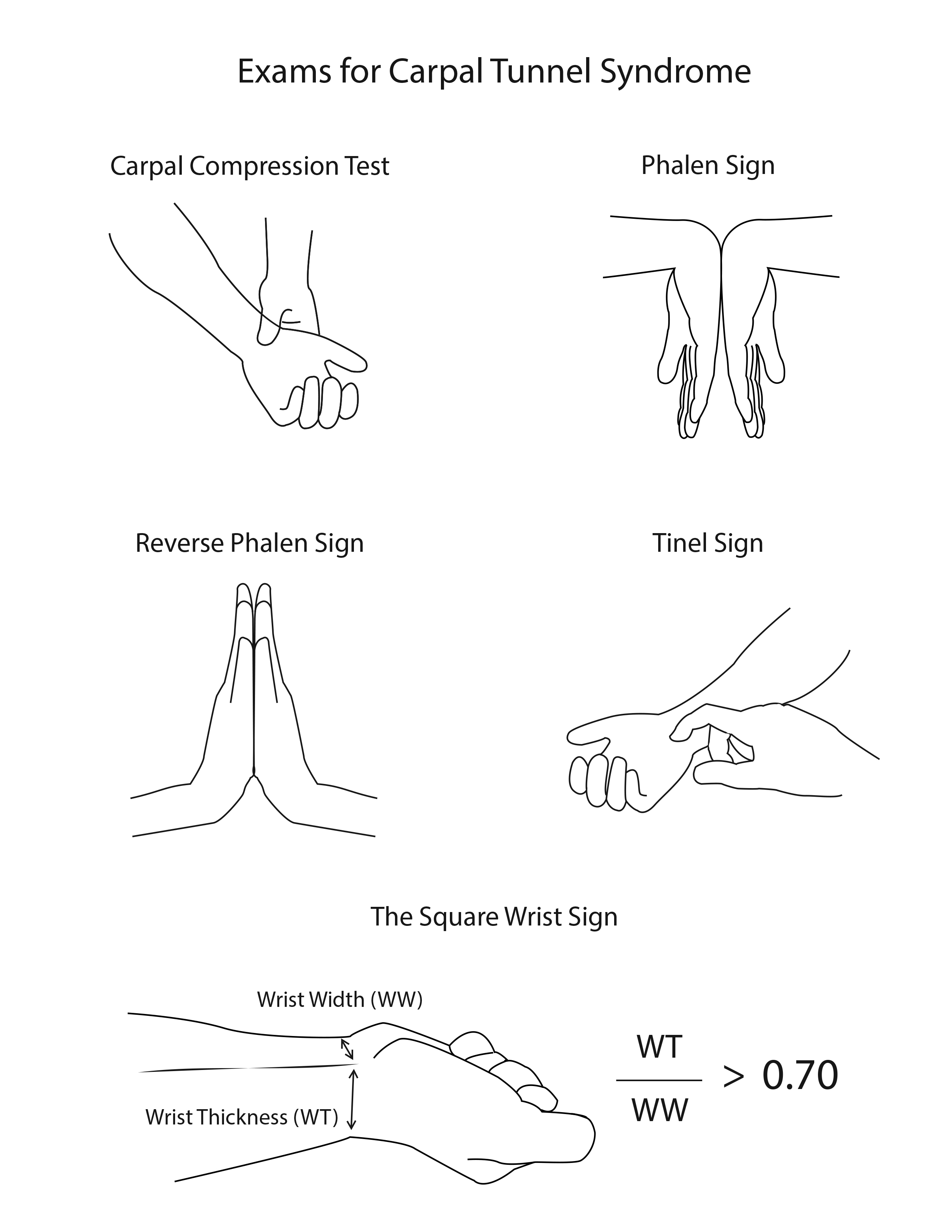
Typically, a clinician arrives at the diagnosis of CTS from a thorough history and physical exam. Provocative maneuvers such as Tinel's and Phalen's tests may elicit symptoms of CTS.[2] Diagnosis of CTS would not normally warrant further investigation when symptoms are mild, and no other differential can better explain the symptoms.[4][5] However, under the presence of severe symptoms such as weakness, sensory deficits, or limitations in activities of daily living, patients should undergo nerve conduction studies (NCS).[5]
It is considered a gold standard in diagnosing CTS as it provides objective, measurable information regarding the median nerve's physiologic health. However, performing electrodiagnostic studies in patients who have unlikely manifestations of CTS (i.e., lack of symptoms in the first three digits) is not helpful, regardless of the result of the NCS.[6][7] Concurrently, NCS is not perfect, as false positives and false negatives are well documented.[2][4]
Other studies used to diagnose CTS include ultrasound (to measure the cross-sectional area of the median nerve) and magnetic resonance imaging of the wrist (to demonstrate abnormal nerve signal).[1]
Contraindications
Performing electrodiagnostic studies in CTS patients has several relative contraindications. Needle electromyography (EMG) is relatively contraindicated in those with severe bleeding disorders or in those who have platelet counts <50,000 per microliter of blood. Some feel an international normalized ratio greater than 1.5 to 2.0 is a relative contraindication. Given that the incidence of significant hematomas while doing EMG for CTS, many feel it is safe unless the INR is higher than the therapeutic range.[8][9]
Needles should also not be inserted in areas of active soft tissue infection. NCS are generally safe for patients with implanted modern bipolar cardiac devices, though the recommendation is to avoid NCS in those with external pacing wires.[8] In a patient with a pacemaker, the electrical stimulation should not be performed directly or near the device itself.
Equipment
- EMG machine
- Surface electrodes (disk or ring) – Active, reference, and ground electrodes
- Needle electrodes
- Amplifiers (magnifies the signal)
- Filters
- Alcohol pads (to clean the skin)
- Tape (to secure the electrodes)
Personnel
- Technician
- Physiatrist or other clinician
Technique or Treatment
Before performing any diagnostic study, a comprehensive review of the patient's history and clinical course, and a complete physical exam is necessary. The technician will inform the patient bedside of the indications and overview of the studies needed to diagnose CTS with electrodiagnostic testing properly. The technician must thoroughly explain the risks and benefits of the exam to the patient and get consent. One should ideally examine at least two extremities, performing both sensory and motor nerve conduction studies and EMG needle testing in both proximal and distal muscles for comparison.
The temperature of the patient's limbs should be kept warm at or above 32 degrees Celsius. Cold temperatures can cause mistakenly increased amplitudes, prolonged latencies, and slowed conduction velocities on NCS.[7] To minimize electrical interference, which can occur while doing the study bedside, a notch filter should be used. If possible, all unnecessary machines turned off, including unplugging the examination or hospital bed.
Complications
As with all electrodiagnostic studies in any setting and for any indication, the risk of complications is low. There is always a small risk of bleeding or introducing infection with needle studies.[8] Mild procedural pain and discomfort also require explanation, especially when performing needle EMG on muscles such as the abductor pollicis brevis.[4][8]
Clinical Significance
Sensory Nerve Conduction Studies
Sensory nerve action potentials (SNAPs) are often the first values that are affected in CTS. SNAPs are measured and recorded at the mid palm and past the carpal tunnel to evaluate the possible differences between the two. Median nerve conduction velocities measuring less than 50 meters per second across the carpal tunnel or a difference of the conduction velocity of the wrist-to-digit segment compared to the palm-to-digit segment greater than 10 meters per second indicate signs of CTS.
An amplitude difference of greater than 50% across the carpal tunnel also rates as significant. The test's sensitivity can be increased by obtaining the combined sensory index, which measures the SNAPs difference between the median, ulnar, and radial nerve at fingers one and four because both digits have dual innervation.[7] This approach to testing can help patients with an initial normal electrodiagnostic test of the median nerve but with CTS's clinical symptoms. The median nerve's fundamental difference compared to the ulnar nerve (paired median-versus-ulnar comparison) is that the former has to pass through the carpal tunnel; therefore, any slowing of the median nerve conduction velocity across the wrist is attributable to the carpal tunnel. Performing this median-versus-ulnar comparison increases the sensitivity of the test from 75% to 95%. Latency difference of 0.4 to 0.5 meters per second is considered abnormal and is significant for CTS diagnosis.
Motor Nerve Conduction Studies
Compound muscle action potential distal latency is measured during the assessment of the motor nerve. Distal latency of greater than 4.2 milliseconds may indicate CTS. As with sensory nerve studies, it is often compared to the ulnar nerve to rule out a generalized motor neuropathy. A decrease in amplitudes during motor nerve stimulation may indicate a lesion along the median nerve or even a conduction block across the carpal tunnel.[10]
Late Responses
F-waves and H-reflex (Hoffman's reflex) are late responses that are often not assessed. These are generally nonspecific, and motor and sensory studies provide a better evaluation of interest areas.
Electromyography
EMG is generally a diagnostic to determine and rule out evidence of axonal damage through the presence of fibrillation potentials or positive sharp waves.[10] The abductor pollicis brevis muscle is tested to look for these spontaneous activities. Should this be the case, other, more proximal median-nerve innervated muscles should be tested to exclude other neuropathy along the median nerve. A conduction block along the carpal tunnel may demonstrate the absence of fibrillation potentials and positive sharp waves but decreased recruitment of the abductor pollicis brevis.
Enhancing Healthcare Team Outcomes
CTS is a condition often seen in the outpatient setting. Patients frequently come with complaints of pain and paresthesias in the hands. Imaging studies, in addition to electrodiagnostic studies, can be routinely ordered. Physicians must be cautious, however, as imaging findings may not correlate with the patient's symptoms. Interprofessional care must use an evidence-based approach for evaluation and management. When CTS is left untreated, mild symptoms may subsequently lead to weakness and atrophy.[7]
Treatment of CTS generally involves the use of conservative management such as wrist splints and non-steroidal anti-inflammatory drugs. Should these fail, other more invasive options may include local corticosteroid injections and surgery involving carpal tunnel release.[3][7]
It is essential to take an interprofessional team including physiatrists, orthopedists, hand surgeons, neurosurgeons, physical/occupational therapists, and social workers who can work together to coordinate outpatient therapy, aggressive multifaceted rehabilitation, and ultimately, surgery to improve a patient's functional status.