Introduction
The femoral head is the most proximal portion of the femur and is supported by the femoral neck. It articulates with the acetabulum of the pelvis. The femoral head is nearly spherical (two-thirds) but has a medial depression known as the fovea capitis femoris that serves as an attachment point for the ligamentum teres. This structure has clinical significance as there is a major concern for avascular necrosis to the femoral head associated with hip fractures and dislocations.
Structure and Function
The femoral head serves as the “ball” in the hip joint allowing for a high degree of motion in the hip. It is covered by articular cartilage and articulates with the lunate surface of the acetabulum. Along with the proximal femur, the femoral head comprises several trabecular orientations of bone that are strong enough to support the rest of the body. The architecture of this bone is formed by Wolff’s law [1]. The primary compressive group is vertically oriented trabeculae from the superior femoral head to the medial neck. The primary tensile group runs from the inferior femoral head to the lateral cortex. The secondary compressive group is oriented along the lines of stress in the proximal femur. The secondary tensile group is oriented along the lines of stress in the lateral proximal femur. The greater trochanteric group is oriented along the lines of stress within the greater trochanter. There is also an area within these trabecular patterns that has relatively few trabecular known as Ward’s triangle. This is not to be confused with Babcock’s triangle which is a radiolucent region of the subcapital region that is a common site for tuberculosis of the hip joint to occur [2].
Embryology
The femur, like most long bones, is formed via endochondral ossification. The head of the femur ossifies at age 1 and fuses at age 18.
Blood Supply and Lymphatics
The blood supply to the femoral head is variable. Three main arteries supply the femoral head. The lateral epiphyseal branch of the medial femoral circumflex and the ascending branch of the lateral femoral circumflex both ascend from the deep femoral artery. This leaves the femoral head vulnerable to avascular necrosis in the presence of a femoral neck fracture since these vessels are easily ruptured with this injury. The ligamentum teres artery descends from the posterior branch of the obturator artery and attaches at the fovea. This artery is commonly disrupted with dislocations. It is the main blood supply to the femoral head in children. As an anatomical variant, the inferior gluteal artery is the main blood supply to the femoral head in a small portion of patients [3].
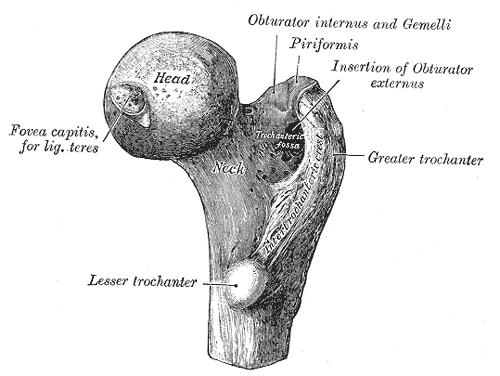
Muscles
No muscles attach directly to the femoral head, but many muscles cross the hip joint to allow flexion, extension, abduction, adduction, internal rotation, and external rotation of the thigh. The psoas major, iliacus, sartorius (also aids in abduction and internal rotation), rectus femoris, and pectineus allow for flexion. The gluteus maximus and hamstring muscles (semimembranosus, semitendinosus, and biceps femoris) allow for extension. The gluteus medius, gluteus minimus, and tensor fascia latae allow for abduction and external rotation. The adductors (adductor longus/brevis/magnus) gracilis, and pectineus allow for adduction. The obturator muscles, gemellus, quadratus femoris, gluteus maximus, and piriformis allow for internal rotation.
Surgical Considerations
Since the femoral head is highly vulnerable to avascular necrosis, it is often deemed easier to replace it with an artificial construct rather than to salvage what is left, especially in the elderly population. Total hip arthroplasty and hemiarthroplasty are both plausible options when avascular necrosis is of high certainty. Open reduction internal fixation can also be utilized with a femoral head fracture with headless compression screws as they do not alter the spherical shape of the femoral head. Small diameter drilling decompression can delay the need for arthroplasty [4].
Clinical Significance
Legg-Calve-Perthes Disease [5]
This is idiopathic osteonecrosis of the proximal femoral epiphysis in children. The blood supply to the femoral head is disrupted followed by revascularization which takes approximately 2 to 5 years. History is typical of young caucasian males (males: females = 5:1) with lower socioeconomic class living in a higher latitude presenting with a painless limp with hip stiffness. It is bilateral in 12% of the cases and affects 1:10,000 children. Risk factors include positive family history, low birth weight, abnormal birth presentation, and second-hand smoke. Prognosis is good with an onset of less than 6 years of age, the sphericity of the femoral head, minimal lateral pillar involvement, and congruency of skeletal maturity. These patients are at an increased risk to develop premature osteoarthritis secondary to an abnormally shaped femoral head. Goals of treatment include resolution of symptoms with analgesics, traction, and crutches, to maintain/obtain the full range of motion through physical therapy and to contain the femoral head through bracing/surgery depending on the severity, so it maintains a good position within the acetabulum.
Slipped Capital Femoral Epiphysis (SCFE) [6]
A disorder of the proximal femoral epiphysis “slipping” through the proximal physis. History is typical for an obese non-caucasian male (male: female = 2:1.4) during a period of rapid growth (age 10-16) presenting with groin, and thigh pain decreased the range of motion of the hip, limp, and less commonly, knee pain for several months. It is the most common disorder affecting adolescent hips found in 10:100,000 children. Risk factors include obesity, endocrine disorders, acetabular retroversion, femoral retroversion, and radiation therapy. It is graded on the percent of epiphysis slippage:
- Grade I: 0% to 33%
- Grade II: 34% to 50%
- Grade III: Greater than 50%.
Treatment includes percutaneous in situ screw fixation for both stable and unstable slips. One cannulated screw is considered the gold standard. Two-screw constructs are more biomechanically stable but face a greater risk of screw-related complications. Contralateral hip prophylactic fixation is also considered for high-risk patients but remains controversial. Open epiphyseal reduction and fixation, osteochondroplasty, and proximal femoral osteotomy also remain viable options depending on the severity of the slippage.
Femoral Head Fractures [7]
This is a rare fracture pattern that is almost always associated with hip dislocations. History is typical of a patient experiencing impaction, avulsion, or shear forces including motor vehicle accidents, falls, and sports injuries are presenting with localized hip pain inability to bear weight. The physical exam is significant for a flexed, shortened lower limb with either adduction and internal rotation with a posterior dislocation or abduction and external rotation with an anterior dislocation. They are classified by the Pipkin classification [8]:
- Type I: Hip dislocation with fracture of femoral head inferior to the fovea (does not involve the weight-bearing portion of the femoral head)
- Type II: Hip dislocation with femoral head fracture superior to fovea (involves the weight-bearing portion of the femoral head)
- Type III: Type I or II + fracture of the femoral neck (high risk of avascular necrosis)
- Type IV: Type I or II + fracture of the acetabular rim
These patients are at high risk for femoral head osteonecrosis and posttraumatic arthritis (posterior wall fracture is most commonly associated).
Nonoperative treatment of femoral head fractures includes hip reduction within 6 hours to reduce the risk of neurovascular and soft tissue injury. In pipkin I or pipkin II with less than 1 mm step off, the patient can undergo conservative treatment of touch down weight bearing with restricted range of motion in adduction and internal rotation for 4 to 6 weeks. The patient is to undergo serial radiographs to ensure adequate healing and maintained reduction [9].
Operative treatment of open reduction internal fixation with headless compression screws is primarily considered with pipkin II with greater than 1 mm step off, type III, and type IV. Patients may also consider reconstruction plates and bioabsorbable screws [10]. Arthroplasty is reserved for older patients and fractures that are significantly displaced, osteoporotic, or comminuted.