Continuing Education Activity
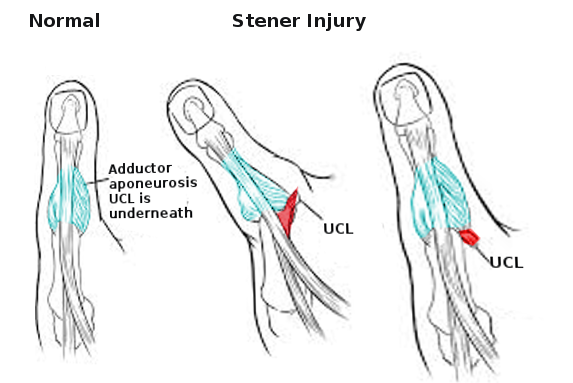
A Stener lesion occurs when a complete distal, thumb ulnar collateral ligament tear results in the interposition of the aponeurosis of the adductor pollicis muscle between the metacarpophalangeal joint and torn ligament. Patients with this lesion present with ecchymosis, soft tissue swelling, and focal tenderness of the ulnar aspect of the thumb metacarpophalangeal joint. This activity outlines the evaluation and management of the Stener lesion and explains the role of the interprofessional team in improving care for those with this condition.
Objectives:
- Describe the regional anatomy and pathoanatomy involved in a Stener lesion.
- Describe several conditions that may mimic a Stener lesion.
- Explain the imaging studies needed to identify a Stener lesion.
- Identify the importance of cooperation among the members of the interprofessional team in prompt diagnosis of this condition to prevent complications such as chronic thumb pain, osteoarthritis, and instability.
Introduction
Ulnar collateral injuries of the thumb are common. These injuries can range from a mild sprain, partial to complete ligamentous tear. Avulsed fragments from the proximal phalanx can also be present.[1]
Full-thickness ruptures are further characterized as being non-displaced or displaced.
This distinction is important because the relationship of the displaced torn UCL ligament to the aponeurosis of the adductor pollicis muscle has clinical implications.[1] This concept first gained recognition by Bertil Stener, a Swedish surgeon who in 1962, described the anatomy and treatment of displacement of the ulnar collateral ligament (UCL) of the metacarpophalangeal (MCP) joint; thus, the eponymously named Stener lesion.[2]
The primary function of the UCL of the thumb is to create ulnar stability of the MCP joint and acts as a counterbalance to any force directed radially during a forceful grasp. The UCL is made up of the proper collateral ligament (PCL) and the accessory collateral ligament.[3]
A stener lesion occurs when there is forceful abduction of the thumb, leading to avulsion of the distal ulnar collateral ligament from its insertion at the base of the proximal phalanx of the thumb. The severed end of the tendon then become entangled in the adductor aponeurosis and unable to return to its normal anatomical position. This leads to an unstable thumb that is often seen in skiers and gamekeepers.
Etiology
Compromise of the UCL comes from sufficient force enough to hyperabduct and hyperextend the first MCP joint.[1] This injury was first described among Scottish gamekeepers who sustained thumb injuries from killing wounded rabbits by holding the head in one hand and the lower limbs in the other and applying a strong pull. After repetitive episodes, the strain exerted to the thumb-forefinger cleft causes a valgus force on the thumb, resulting in chronic, thumb instability due to the insufficiency of the UCL of the MCP joint, aptly called the gamekeepers thumb. Similar injuries are seen today, acutely, from a fall onto the ground with an abducted thumb with a ski pole in hand.[3][4] Historically, clinicians have used gamekeepers thumb, and skiers thumb interchangeably. The former however denotes a chronic UCL injury while the latter is an acute hyperabduction of the UCL.[5]
Injuries thru the same mechanism also occur from sports such as hockey, soccer, handball, basketball, and volleyball.[3] Recently, a Stener lesion was diagnosed in a patient who injured his hand while performing a handstand.[5]
A torn UCL can get caught over the aponeurosis of adductor pollicis creating a “lesion” initially described by Stener.[6]
Epidemiology
About 200000 cases of UCL thumb injuries occur yearly.[1][2] Stener lesions occur in 64% to 87% of all complete UCL ruptures.[7] As high as 32% of all ski injuries may involve the thumb. UCL ruptures are rare in the pediatric population.[8]
Pathophysiology
Appreciation of the regional anatomy and close structural relationship between the adductor pollicis aponeurosis and the UCL is central to the understanding of a Stener lesion pathophysiology. Hung et al. described the anatomy as “ The PCL originates from the dorsal third of the metacarpal head and inserts on the volar aspect of the proximal phalanx. The ACL originates palmar to the PCL and runs continuously with the PCL to insert on the volar plate. The PCL is taut in flexion, while the ACL is taut in extension. Both ligaments ensure the ulnar stability of the MCP joint. The Adductor pollicis inserts on the proximal phalanx, functioning as a dynamic stabilizer of the MCP joint. It lies superficial to the UCL.”[3]
The UCL lies deep to the adductor pollicies tendon. A Stener lesion occurs when a complete distal, thumb UCL tear results in the interposition of the aponeurosis of the adductor pollicis muscle between the MCP of the joint and torn ligament.[4]
This interposition results in the adductor aponeurosis acting as a barrier separating the ruptured ends of the ligaments preventing healing.[1][4] In short, a Stener lesion is UCL that is torn, displaced and entrapped.[5]
History and Physical
Patients with UCL injuries may present with soft tissue swelling, ecchymosis, and focal tenderness at the ulnar aspect of the thumb MCP joint.[3][4][5][9] Instability of the thumb, and grip and pincer grasp weakness may also be evident, especially in patients who delayed presentation.[4][9] A mass may be palpated proximal to the MCP joint suggestive of a Stener lesion, but this is not pathognomonic.[3]
Valgus stress testing during a physical exam does not distinguish between displaced and non-displaced UCL injuries, even if it demonstrates MCP joint instability. Caution is also advisable during valgus stress testing as it may inadvertently convert a non-displaced tear into a displaced one, which is also the reason why abduction stress view radiography is no longer a recommendation.[1][10] Complicating the clinical picture are several conditions that mimic UCL/MCP joint pain, making accurate diagnosis difficult, without the aid of diagnostic imaging.[1]
Classification of acute UCL based on imaging:
- Type 1: Nondisplaced avulsion injury
- Type 2: There is a displaced fracture at the ulnar region of the base of the proximal phalanx
- Type 3: There is straining of the ligament
- Type 4: The UCL is completely torn
- Type 5: The is no injury to the UCL but avulsion of the volar plate is present
Evaluation
Plain film X-ray is the most common initial imaging modality to evaluate hand injuries and associated fractures and MCP joint instabilities. UCL distal end injury is suspected if an avulsed bony fragment in the proximal phalanx is present. A displacement greater than 1 mm indicates a displaced UCL tear.[3] Plain radiographs, however, can be normal despite the presence of gamekeeper injury. Further imaging, therefore, is often indicated if the clinical suspicion is high especially if a Stener lesion is also under consideration.
Magnetic resonance ( MR ) arthrography is considered the gold standard when evaluating for UCL injuries.[1] Despite the reported sensitivity of 96% and specificity of 95%, MRI does come with a high cost and restricted availability.[3]
Recent literature has highlighted the growing advantage of ultrasound (US). In addition to being non-invasive, cost-effective, and less time consuming, ultrasound has been shown to have 100% sensitivity and specificity in discerning between non-displaced and displaced tears.[1] Others have reported that depending on the experience of the examiner, the accuracy of ultrasound in diagnosing a Stener lesion ranges from 81% to 100%.[3]
The real-time capability of the ultrasound can easily show the anatomic relationship of the UCL as it pertains to adductor aponeurosis.[1] Dynamic ultrasound imaging with the interphalangeal joint of the thumb in passive flexion can distinguish between a non-displaced UCL tear and a Stener lesion.[11][12] Ultrasound also affords quick comparative imaging of the uninjured side.[1]
The appearance of a Stener lesion on the ultrasound has been called the “tadpole sign” or “yo-yo on a string sign.” Ridley et al. note “The head of the tadpole is formed by the retracted proximal fragment of the UCL which displaces to be adjacent to the head of the metacarpal. The tail of the tadpole is formed by the adductor aponeurosis which is often thickened and lies deep to the retracted UCL fibers.”[13] The “yoyo on a string sign” appearance presents by the small mass displaced superficial to the adductor pollicis from the torn ligament fibers that retracted proximally. The “yoyo on a string sign” can also be seen in an MRI.[6]
Treatment / Management
The goals of treating any UCL injury are mitigation and eventual relief of pain, avoidance of instability, and prevention of osteoarthritis.[5] A majority of patients with gamekeepers' thumb are managed non-surgically with the use of long arm thumb spica splint. Immobilization may span several weeks. However, if a Stener lesion is present, operative treatment is indicated as healing will not occur due to the separation between the ruptured ends of the ligaments from the Stener lesion. A bone anchor is utilized to reinsert the torn ligament.[4]
Treatment strategy based on the classification of the injury:
- Type 1: Minimally displaced/partial UCL tears usually heal with immobilization alone
- Type 2: UCL tears that are displaced less than 3 mm can be healed with immobilization alone
- Type 3: UCL tears that are displaced more than 3 mm will usually fail immobilization and most patients with require surgery
- Type 4: Stener lesion will require surgery in all cases
Non-surgical therapy is effective for type 1,2 and some 3 lesions. The thumb is immobilized in thumb spica for 4 weeks.
Chronic UCL injuries are difficult to repair. If the patient has moderate to severe arthritis, arthrodesis of the MCP joint is an option. If arthritis is not present, then ligament reconstruction of tendon advancement are options.
Differential Diagnosis
Conditions that can mimic a UCL injury include[6]:
- Dorsal hood tear
- Thenar Muscle Injury
- Radial collateral ligament injuries
- De Quervain disease
- First carpometacarpal joint osteoarthrosis
- Vascular injury to the superficial branch of the radial artery
- Volar plate injury
- Extensor pollicis longus tear
- Trigger thumb
- Flexor carpi radialis tendon tendinosis
- Flexor pollicis longus tendon rupture
Prognosis
Ninety percent of patients with a complete rupture of the UCL treated with primary repair within 3 weeks have been reported to have good-to-excellent outcomes regardless of repair method.[8]
However, delayed presentation and or treatment often results in extensive surgery, with a poor overall result.
Complications
Delayed presentation and diagnosis of UCL injuries influence clinical outcome and impede timely return to activities.[8] Undiagnosed and untreated Stener lesions can lead to chronic thumb pain, instability, and osteoarthritis.[5] While surgical intervention is needed to repair a Stener lesion, there have been reports of radial nerve sensory neurapraxia, recurrent instability and stiffness of the IP and MCP joints after surgical correction.[8]
Postoperative and Rehabilitation Care
Post-surgical treatment includes 6 weeks of immobilization. Three months following surgery, the patient may return to activity without restrictions.[8] Others have advocated thumb spica for 1 to 4 weeks postoperatively, followed by flexion-extension exercises.[9]
Consultations
- Orthopedic surgery
- Radiology
- Sports medicine
Deterrence and Patient Education
UCL injuries can be missed by clinicians not having enough experience with testing the UCL. Additionally, patients also may delay seeking medical attention because the injury occurred during a vacation (e.g., skiing), initial X-rays were normal, or they waited to see their doctor once they returned home.[7]
Enhancing Healthcare Team Outcomes
Identification of a Stener lesion is important as the surgical correction is required to avoid chronic instability, pain, and osteoarthritis.[4][5] When patients with skin injuries to the thumb present in the emergency department, the primary care physician or nurse practitioner, should seek early consultation with an orthopedic specialist. Plain films, dynamic ultrasound, and MRI are often needed if the physical exam is unrevealing, yet the suspicion for a UCL tear and a Stener lesion is high.[5]
Patients treated non surgically may be followed by the primary care clinicians but all patients undergoing surgery must be followed by the surgeon, as complications are not uncommon.
Interprofessional communications between the treatment team consisting of the nurse practitioner, physician assistant, nursing, pharmacy, and physicians and the radiologist are therefore crucial to enhance timely diagnosis and successful treatment.