Continuing Education Activity
Myofascial trigger points are focal "knots" located in a taut band of skeletal muscle first described by Dr. Janet Travell in 1942. Trigger points may be formed after acute trauma or by repeated micro-trauma, leading to stress on muscle fibers. Trigger point injections are a therapeutic modality to treat myofascial trigger points, especially in symptomatic patients, and have been demonstrated effectiveness to inactivate trigger points. Treating pain with a multimodal approach is paramount in providing safe and effective results for patients. Trigger point injections can be wonderful adjunctive or primary therapy, alongside muscle relaxants, and other medications aimed at decreasing pain in the musculoskeletal system.
Objectives:
- Describe how to diagnose trigger points.
- Identify indications for trigger point injections.
- Outline the technique to perform trigger point injections.
- Summarize how an interprofessional team can work together to provide trigger point injections as an alternative treatment in patients suffering from musculoskeletal pain.
Introduction
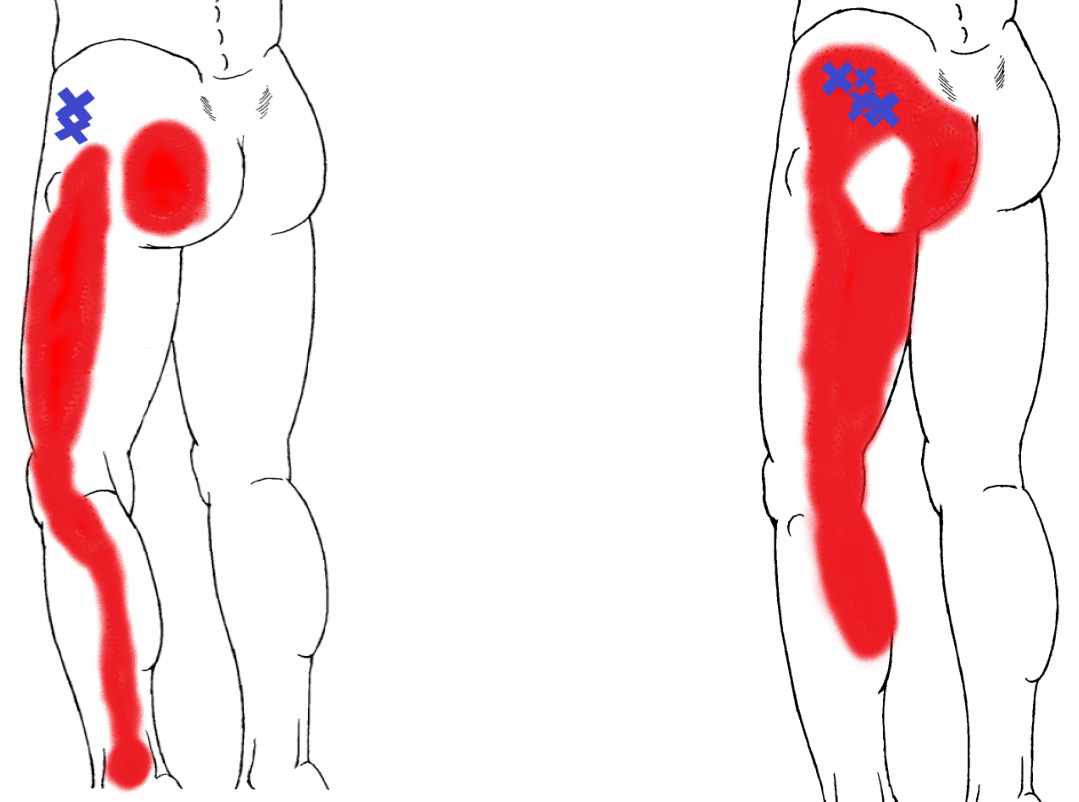
Myofascial trigger points are focal "knots" located in a taut band of skeletal muscle first described by Dr. Janet Travell in 1942. These points are usually palpable and produce a characteristic referred pain upon palpation, along with pain locally and occasionally a local twitch response. Trigger points may also cause stiffness and decreased range of motion, and can sometimes be associated with chronic disorders of the musculoskeletal system.[1] Trigger points may be formed after acute trauma or by repeated micro-trauma, leading to stress on muscle fibers.[2]
Trigger points are often confused with the term tender points. These are not synonymous, as tender points denote a focal nodule that produced pain directly under the area of palpation, but does not cause a referred pain.
Patients can have one or several trigger points throughout their musculoskeletal system. There are several approaches to the treatment of trigger points including ultrasonography, physical manipulation therapy, Spray and Stretch technique, and injections.[2]
Anatomy and Physiology
Pathogenesis of trigger points is thought to be related to abnormal motor end-plates within a muscle where the motor and nociceptive nerves co-exist, with a component of enhanced central sensitization in the spinal cord.[3][4] EMG studies have shown that trigger points exhibit spontaneous electrical activity, which suggests aberrant action potential generation.[5] This concept is supported by histological evidence through muscle biopsies showing evidence of muscle hyper-contracture consistent with continuous sarcoplasmic reticulum calcium release secondary to neural activation and action potential generation.[5][6] Patients may experience localized pain which can result in muscle tension and decreased range of motion in affected tissue.
The most common muscle groups treated using trigger point injections include the masseter, levator scapulae, gluteus medius, quadratus lumborum, trapezius, sternocleidomastoid, and temporalis muscles.[7] Trigger points affecting the trapezius muscle may clinically manifest as tension headaches, pain in the neck, shoulders, and proximal arms.[8] The Iliopsoas muscle is the primary muscle responsible for trigger points causing groin pain.[9]
Indications
Trigger point injections (TrPi) are a therapeutic modality to treat myofascial trigger points, especially in symptomatic patients, and have been demonstrated effectiveness to inactivate trigger points. They are believed to cause a temporary relaxation of the taut muscle cord, which in turn allows for improved perfusion, ATP replenishment to release the actin-myosin chains causing lengthening of the muscle fiber, along with removal of metabolite waste. These factors assist in breaking the pain-tension cycle. [4][11]
Indications for trigger point injections include identifiable palpable tender area that produces a referred pain pattern. Common concomitant symptoms include chronic or episodic headaches,[7] temporomandibular joint pain, back pain, decreased range of motion secondary to trigger points, and groin pain.
Contraindications
Contraindications to trigger point injections include the following[7]:
Absolute:
- Patient refusal
- Active infection over the site of trigger point
- Local open skull defect
- TrP not safely accessible by needle
Relative:
- Practice caution in patients taking anticoagulation, pregnant patient, and in patients where anatomical landmarks are indistinguishable.
- Avoid local anesthetics in those with known allergies
- Severe fibromyalgia
- History of keloid formation
- Poorly controlled psychiatric disorder
- Patient is highly anxious or needle-phobic
Equipment
Materials for trigger point injections include the following:
- 27- to 30-gauge 1.5-inch needle OR acupuncture needles for dry needling techniques
- A 3, 5 or 10-mL syringe
- Gloves, typically non-sterile
- Anesthetic agent (optional): Lidocaine or bupivacaine without epinephrine
- Consider sodium bicarbonate 5% to be added as a buffer to decrease discomfort
- May include a small amount of corticosteroid, such as triamcinolone
- Consider alternative prolotherapy solution such as D5W or sterile saline
- Topical anesthetic spray (optional), such as ethyl chloride
- Consider steroids such as triamcinolone or dexamethasone to possibly add to the local anesthetic mixture (optional)
- Skin cleaning agents such as alcohol pads or chlorhexidine 2%
- Pulse oximeter and blood pressure monitor
Personnel
Trained and skilled medical providers including physicians, physician assistants, and nurse practitioners can perform trigger point injections. It is recommended to have medical support staff available for preparation of the procedure.
Preparation
The patient should be informed about the risks and benefits of trigger point injections. Obtain written consent by the patient or guardian decision maker before the start of the procedure. Equipment should be ready at the bedside, and another medical staff member should be available for time-out prior to starting the procedure. Depending on the trigger point location, the patient may be sitting or laying down. Cleanse the area with alcohol pads or chlorhexidine 2%, allowing it to dry. Some providers prefer to mark each trigger point with a skin marker or retracted pen tip as a guide prior to starting the procedure. If using a topical anesthetic spray, make sure to anesthetize the trigger points before starting the procedure.
Technique or Treatment
Once a trigger point has been identified and the overlying skin cleansed, the clinician should use their non-dominant index finger and thumb to pinch the point between their fingers and stabilize the tissue. Once stabilized, using the dominant hand, the clinician will insert the needle attached to the 5 or 10mL syringe at a 30-degree angle into the trigger point and rhythmically continue needling the area by repeatedly inserting and retracting the needle without completely withdrawing the needle from the muscle. The clinician should continue this motion in multiple directions until muscle twitching has subsided, or until the muscle feels adequately relaxed. A "crunching" or "pulling" may be felt as the clinician inserts and retracts the needle within the tense muscle; this will likely decrease throughout the treatment. If dry-needling is the method, then treatment of that point is completed once the trigger point is relaxed. If an injection is the planned intervention, then the clinician should then aspirate to ensure the needle is not in a vascular structure and then inject 0.2 to 1 mL of selected solution into the point. A direct or fanning approach may be used. If treating multiple points then repeat the above steps. There are comparable results between dry needling and injection of local lidocaine; however, it has been shown that less post-needling soreness is associated with the injection of local anesthetic.[10] If available, and if the provider is trained, use of ultrasonography for guided injection may be considered to confirm desired structure and depth while avoiding neurovascular structures [11],[12].
Complications
Complications of trigger point injections include the following[13][7][14][15]:
- Pain
- Bleeding
- Infection
- Allergic reaction to the anesthetic agent
- Systemic anesthetic toxicity
- Formation of a hematoma
- Vascular injury
- Although rare, there are some reports of complications such as pneumothorax, especially when treating trigger points in the cervicothoracic region using a needling technique
- For trigger points along the thoracic cage, recommend use of a pincer grip to bring the affected tissue away from the intercostal spaces. A tangential rather than vertical vector may also decrease risk of entering the pleura
- Severe hypokalemic paralysis has also been reported in one case report
- Adverse effects connected to dry-needling technique include soreness after treatment, vasovagal and syncopal response, hemorrhages at the site of treatment, and acute cervical epidural hematoma
Clinical Significance
Musculoskeletal pain is a common complaint that many primary-care and pain providers diagnose and treat regularly. Treating pain with a multimodal approach is paramount in providing safe and effective results for patients. Trigger point injections can be an effective primary or adjunctive therapy aimed at decreasing pain in the musculoskeletal system. By targeting specific points of myofascial pain, clinicians can directly treat pathologic tissue, address a patient's pain generator, and break the pain cycle with little to no side effects. Patients can have significant improvement in range of motion and overall functionality, without the need for taking pain medications. Meaningful results can be provided with trigger point injections and should merit consideration as a treatment modality in the appropriate setting.
Enhancing Healthcare Team Outcomes
Patient safety is of the utmost importance. Trigger point injections can be a valuable adjunct to treating chronic pain conditions involving the musculoskeletal system. A detailed history and musculoskeletal physical exam are suffering in preventing adverse outcomes.
A team-based, interprofessional approach should be implemented to ensure patient safety and the appropriateness of the procedure. This team should include the physician or mid-level practitioner, as well as a nurse or healthcare technician to prepare the patient and assist during the procedure. If being performed as an inpatient procedure, the pharmacist may also be involved in preparing the injection and assure appropriate dosing and check for allergy risk. The designated staff member assisting should monitor the patient during the procedure, assist with patient education, and report changes in vital signs should they occur.
Communication with the patient throughout the procedure is essential to make sure the treatment is addressing an active trigger point. Healthcare professionals should always take caution when handling sharps as accidental needle sticks may occur. Universal precaution guidelines should be followed, and hazardous materials should be disposed of appropriately. Documentation post procedure should include the location of trigger points treated; muscles injected, amount of selected medications used (if any), patient position during treatment, and post-procedure plan.
An interprofessional approach involving the clinicians, nurses, and pharmacists will result in the best patient outcomes. [Level 5]