Introduction
Pelvic floor prolapse is the herniation of the pelvic organs through the perineum. Depending on the pelvic organ involved, pelvic prolapse further categorizes into the anterior compartment containing urinary bladder(cystocele), the middle compartment containing uterine or vaginal prolapse (uterus or vagina), or the posterior compartment containing either the small bowel loops (enterocele) or rectum (rectocele). Pelvic prolapse is very common among multiparous women over 50, affecting approximately 50% of women over age 50.[1] The patients present with symptoms of stress fecal or urinary incontinence, uterine prolapse, constipation, or incomplete defecation. Besides, pelvic prolapse can negatively impact the patient's body image and sexuality. Pelvic prolapse treatments range from non-surgical approaches like Kegel exercise and pessary to various surgical procedures.[2] Treatments of pelvic prolapse significantly contribute to the healthcare cost in the United States, estimated at approximately $300 million from 2005 to 2006.[3]
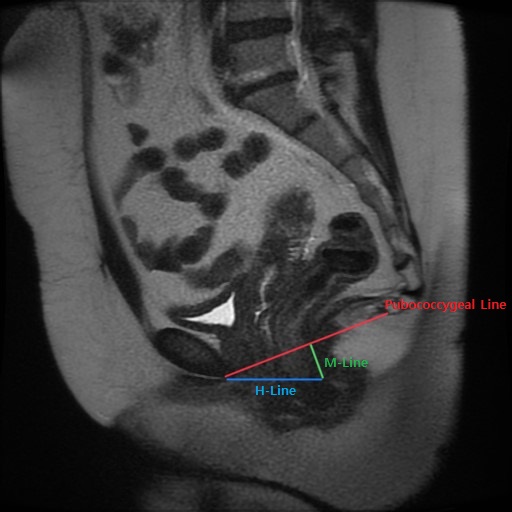
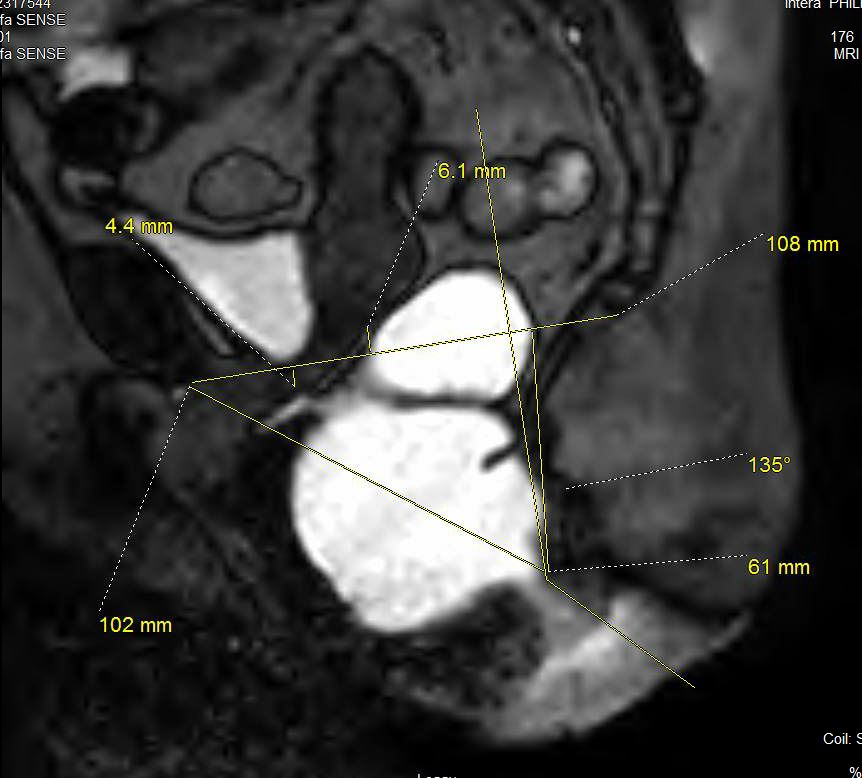
Pelvic floor prolapse is most often clinically diagnosed through physical exams and medical history. Imaging plays a limited role in evaluating mild cases of pelvic prolapse that involve a single pelvic compartment and organ. Nonetheless, translabial ultrasound and dynamic pelvic MRI (MR defecography) serve as valuable tools in diagnosing pelvic prolapse in complex cases involving multiple compartments and multiple pelvic organs. Also, pelvic MRI provides pre-operative planning for complex cases. The article will discuss translabial ultrasound and dynamic pelvic MRI in the evaluation of pelvic prolapse.[4]