Introduction
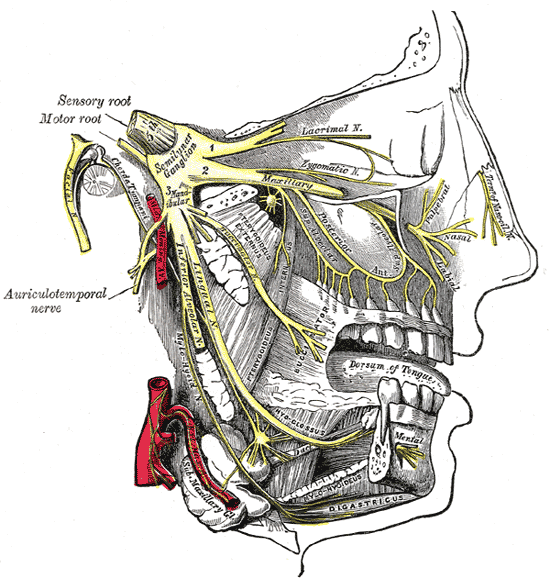
The fifth cranial nerve, known as the trigeminal nerve (V), is the largest of the twelve cranial nerves and carries both sensory and motor fibers.[1] It has three terminal branches, which in descending order are ophthalmic nerve (V1), maxillary nerve (V2), and mandibular nerve (V3). The ophthalmic and maxillary divisions carry only sensory fibers while the mandibular division carries both sensory and motor fibers. The intermediate division, maxillary nerve (V2), primarily supplies sensory innervation to the middle third of the face. It also carries postganglionic fibers from pterygopalatine ganglion which supply the lacrimal gland and mucous glands of the nasal mucosa.
Structure and Function
The maxillary nerve arises from the anterior convexity of trigeminal ganglion between ophthalmic and mandibular divisions of the trigeminal nerve. It is a medium-sized branch compared to the smaller ophthalmic nerve and the larger mandibular nerve. It courses forward embedded in the lateral wall of the cavernous sinus along with the oculomotor nerve, trochlear nerve, and ophthalmic division of the trigeminal nerve. It runs inferior and lateral to the ophthalmic nerve. It then leaves the middle cranial fossa through foramen rotundum and enters the superior part of the pterygopalatine fossa. The pterygopalatine fossa is a bilateral cone-shaped space posterior to the maxilla, where the maxillary nerve communicates with the parasympathetic pterygopalatine ganglion and gives off most of its branches.[2] The nerve then leaves the fossa and enters the floor of the orbit through inferior orbital fissure as the infraorbital nerve. The infraorbital nerve represents the terminal branch of the maxillary nerve. The infraorbital nerve courses forward, first through the infraorbital groove, and then through the infraorbital canal on the floor of the orbit. It finally emerges on the face through the infraorbital foramen, located near the inferior margin of orbit.
As stated previously, the maxillary nerve is exclusively sensory and carries pain, temperature, and tactile information from the region below the orbits and above mouth. This includes lower eyelid, skin that covers the side of the nose, cheek, maxillary sinus, nasopharynx, nasal cavity, palate, upper teeth, upper lip, and dura mater of the middle cranial fossa. The sensory information from these areas moves along axons whose cell bodies are located in the trigeminal ganglion, located within Meckel’s cave. The central processes of these nerve fibers form the large sensory nerve root of the trigeminal nerve, which enters the brainstem at the level of the pons. The sensory information travels in the sensory nerve root and is relayed through the main trigeminal nucleus and nuclei of thalamus before it is processed in the cerebral cortex.[3]
Embryology
At the beginning of the fourth week of gestation, the first pharyngeal arch, also known as the mandibular arch appears. It splits into a dorsal maxillary and ventral mandibular prominences and is innervated by the trigeminal nerve. Therefore, the terminal branches of the maxillary nerve provide sensory innervation to the derivatives of maxillary prominence of the first pharyngeal arch.[4]
Blood Supply and Lymphatics
The blood supply of the maxillary nerve varies along its course. At the level of the pons, proximally the nerve receives blood supply from the superolateral and inferolateral pontine arteries and the peduncular cerebellar branch of the anterior inferior cerebellar artery (AICA).[5] In the middle cranial fossa, it receives supply from the artery to the foramen rotundum, an anterolateral branch of the inferolateral trunk arising from the internal carotid artery. Also, the middle meningeal and accessory meningeal arteries also contribute to the blood supply. In the pterygopalatine fossa, it is perfused by branches of the maxillary artery, which is one of the terminal branches of the external carotid artery.
Nerves
The branches of the maxillary nerve subdivide into four groups according to their location of origin, as follows:
1) Cranium:
While coursing through the middle cranial fossa, the maxillary nerve gives rise to its smallest branch, the middle meningeal nerve near foramen rotundum. This branch supplies the dura mater of the middle cranial fossa.
2) Pterygopalatine fossa:
The pterygopalatine fossa holds the pterygopalatine ganglion, which is the largest of the four parasympathetic ganglia. It suspends near the sphenopalatine foramen, anterior to the pterygoid canal and medial and inferior to the maxillary nerve. It receives vidian nerve superomedially and ganglionic branches from the maxillary nerve superolaterally. The vidian nerve is formed by the junction of the greater petrosal nerve and deep petrosal nerve within the pterygoid canal.[2] The greater petrosal nerve brings parasympathetic fibers from the facial nerve at the level of the geniculate ganglion, and the deep petrosal nerve brings sympathetic fibers from the carotid plexus. Therefore, pterygopalatine ganglion contains postganglionic parasympathetic and sympathetic fibers along with general sensory fibers of the maxillary nerve. These three types of fibers leave the ganglion as orbital, palatine, nasal and pharyngeal branches.
These small branches travel through the inferior orbital fissure and contribute to the innervation of orbital wall, sphenoidal sinus, and ethmoidal sinus.
The greater and lesser palatine nerves originate from the inferior surface of pterygopalatine ganglion and pass through the palatine canal. The greater palatine nerve emerges on the oral surface of palate through the greater palatine foramen and travels forward within a groove on the inferior surface of the hard palate. It innervates the mucosa and glands of the hard palate, along with adjacent gingiva. It also communicates with the terminal filaments of the nasopalatine nerve. The lesser palatine nerve emerges on the oral surface through the lesser palatine foramen and travels posteriorly to supply the soft palate, tonsils, and uvula.
These branches travel medially from the pterygopalatine ganglion and enter the nasal cavity through the sphenopalatine foramen. They include medial and lateral posterior superior nasal nerves and nasopalatine nerve. The lateral posterior superior nasal branches run anteriorly to supply the mucosa of the lateral wall of the nasal cavity. While the medial posterior superior nasal branches pass across the nasal roof to supply the medial wall. The nasopalatine nerve, which is the longest among nasal branches, passes across the nasal roof and travels anteriorly down the nasal septum. It emerges on the roof of the oral cavity through the incisive canal and innervates the mucosa, gingiva, and glands adjacent to incisor teeth.[6] It also communicates with the greater palatine nerve.
It arises from the posterior aspect of the pterygopalatine ganglion, transverses the palatovaginal canal, and innervates the mucosa and glands of the nasopharynx.
Ganglionic branches are two in number and originate directly from the inferior surface of the maxillary nerve. They connect the maxillary nerve with pterygopalatine ganglion and carry postganglionic parasympathetic nerve fibers which later join zygomaticotemporal nerve and innervate lacrimal gland through a communicating branch.
- Posterior superior alveolar nerve:
Posterior superior alveolar nerve directly arises from the maxillary nerve and runs laterally out of the pterygopalatine fossa through the pterygomaxillary fissure to enter infratemporal fossa. It then travels laterally and inferiorly to pierce the infratemporal surface of the maxilla. After entering the maxillary sinus, it runs under the mucosa and supplies the mucous membrane. It then divides into branches and contributes to the superior dental plexus. It also provides vascular supply to the upper molar teeth and adjacent buccal gingivae.
Zygomatic branch, after directly originating from the maxillary nerve exits the pterygopalatine fossa through the inferior orbital fissure. It travels on the lateral wall of the orbit and divides into zygomaticotemporal and zygomaticofacial branches. Both the branches travel along the inferolateral angle of the orbit. The zygomaticotemporal branch transverses a bony canal within the zygomatic bone and enters temporal fossa through a foramen. It supplies the skin of the temporal area. It also gives off a communicating branch to the lacrimal nerve of ophthalmic division and conveys secretomotor fibers to the lacrimal gland. The zygomaticofacial nerve also transverses a bony canal and emerges on the face through multiple foramina in the zygomatic bone. It innervates skin on the cheek prominence.
3) The floor of the orbit:
After exiting the pterygopalatine fossa through the inferior orbital fissure, the maxillary nerve enters the orbit as infraorbital nerve which is its terminal branch. In the floor of orbit the infraorbital nerve gives off following two branches:
- Middle superior alveolar nerve:
The middle superior alveolar nerve arises in the infraorbital groove and runs down in the lateral wall of the maxillary sinus and supplies the mucous membrane. It gives off small branches to the superior dental plexus which supplies the upper premolar teeth.
- Anterior superior alveolar nerve:
The anterior superior alveolar nerve branches off the infraorbital nerve just before it exits through the infraorbital foramen. It travels in the anterior wall of the maxillary sinus and supplies the mucous membrane. It gives off branches to the superior dental plexus which supplies the upper incisor and canine teeth. It also gives rise to a nasal branch, which travels through a canal in the lateral wall of inferior meatus to provide innervation to the mucous membrane of the lateral wall and floor of the nasal cavity.
4) On the face:
The infraorbital nerve, after emerging from the infraorbital foramen divides into three main terminal branches, which are as follows:
- Inferior palpebral branches:
They are usually two to three in number and ascend to supply the skin and conjunctiva of the lower eyelid. Near the lateral canthus of the eye, these nerves communicate with zygomaticofacial and facial nerves.
The external nasal branch supplies the skin of the lateral surface of the nose, and the internal branch supplies the nasal septum and vestibule of the nose. The nasal branches communicate with the external branches of the anterior ethmoidal nerve, which is a continuation of the nasociliary nerve, a branch of ophthalmic division.
- Superior labial branches:
These are numerous and supply the skin of the anterior part of the cheek, upper lip, oral mucosa, and labial glands. They form the infraorbital plexus along with the zygomatic branch of the facial nerve.
Physiologic Variants
Some anatomical variations in the course and branches of maxillary nerve exist, knowledge of which is necessary to reduce anesthetic and surgical complications. The maxillary nerve can be bifid in some cases. The posterior superior alveolar nerve can supply the region usually innervated by the buccal nerve. The zygomatic nerve can pass through the zygomatic bone before it divides into its branches. The area supplied by the zygomatic branch receives supply from the infraorbital nerve instead. Sometimes, the middle superior alveolar nerve may be absent, in which case the posterior superior alveolar nerve supplies the premolar teeth.
In some cases, the infraorbital foramen, usually single, can be two to three in number. This variation is particularly significant during the infraorbital nerve block, which is often used to induce regional anesthesia of face. The greater palatine nerve can sometimes give off branches to innervate upper molar and premolar teeth. This variation is adequate for superior alveolar nerve block. Similarly, the nasopalatine nerve, in some cases, innervates incisor teeth; thus, a nasopalatine nerve block is essential to complete anesthesia of incisor teeth.
Clinical Significance
Clinical Examination
As mentioned before, the maxillary nerve carries sensory information of touch, pain, and temperature from the face, along with the ophthalmic and mandibular divisions of the trigeminal nerve. To assess the ability to feel light touch, the patient is asked to shut eyes, and the practitioner uses a cotton wisp to lightly touch both sides of the three divisions of the trigeminal nerve and compares the sensation from both sides using the patient's feedback. Testing of the ophthalmic division is by touching the forehead maxillary division testing is by touching the cheeks, and testing the mandibular division is by touching the area around the jawline.[7] To assess pain and temperature, the examiner performs similar steps, but in place of the cotton wisp, a sharp pin and a cold tuning fork serve as testing implements, respectively.
Lesions Affecting the Maxillary Nerve and its Branches
The maxillary division of the trigeminal nerve can be affected by various pathologies, which include compromise of the sensory root of the trigeminal nerve, infections, iatrogenic injury, or trauma.
Trigeminal neuralgia is a clinical condition that affects the sensory root of the trigeminal nerve. The exact pathophysiology is still unknown but it may result from damage to the nerve from conditions like stroke, trauma, tumor, aneurysm, or multiple sclerosis. It is characterized by chronic pain in the areas supplied by the branches of the trigeminal nerve, including the maxillary division. The pain is severe, sharp, sudden in onset, and shock-like in character, lasting for a few seconds to minutes. It can be triggered by everyday activities like shaving, eating, or brushing teeth. It is unresponsive to normal analgesics. The first-line treatment includes medications like anticonvulsants but resistant cases can be treated by surgical destruction of the sensory root.[8]
Herpes zoster virus infects trigeminal ganglion and can cause severe pain in all sensory areas supplied by the trigeminal nerve, including the maxillary division. It usually affects elderly and immunocompromised patients. In severe cases, complete loss of sensation might result in affected regions.[9]
The maxillary nerve can also be involved in conditions affecting the cavernous sinus like infections, meningioma, or metastatic tumors. Lesions that affect infraorbital nerve in the infraorbital foramen, like the perineural spread of skin cancer, can cause numb cheek syndrome, which presents with numbness in cheek and upper lip. The upper incisor and canine teeth along with gingiva can also have involvement in this condition.[10] The branches of the infraorbital nerve like the superior labial nerve or anterior superior alveolar nerve suffer injury in musicians who play brass instruments. This condition is known as trumpet player neuropathy and presents with pain and numbness in the upper lip.[11]