Introduction
The word "thenar" means fleshy mounds. In human anatomy, the word thenar is associated with the two fleshy mounds located in the palmar surface of the hand. These thenar mounds are called the thenar eminence and the hypothenar eminence. The thenar eminence is the fleshy mound at the base of the thumb. The hypothenar eminence is the mound located at the base of the fifth digit (little finger).
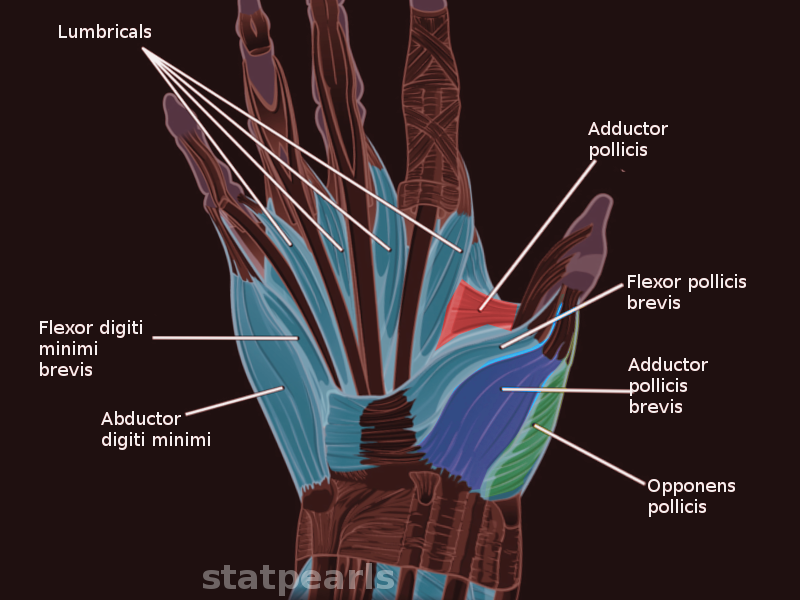
The eminences at either side of the hand are made up of muscles. The muscles located in the thenar eminence function primarily to control the thumb. The muscles in the hypothenar eminence will contract and manifest motion through the little finger.
The hypothenar eminence is made up of 4 muscles, but there are only three primary muscles. The 4 muscles are the abductor digiti minimi muscle, the flexor digiti minimi brevis muscle, the opponens digiti minimi muscle, and the palmaris brevis muscle. All these muscles contract and create specific movements of the little finger. The palmaris brevis is primarily concerned with cupping the skin of the palm.
Structure and Function
The hypothenar eminence is on the medial side of the hand. This group of muscles are intrinsic muscles of the hand because they arise and insert in the hand. The hypothenar eminence is formed from the abductor digiti minimi muscle, the flexor digiti minimi brevis muscle, the opponens digiti minimi muscle, and the palmaris brevis muscle. The abductor digiti minimi muscle causes the little finger to abduct away from the hand (moves the little finger medially) when it contracts. The opponens digiti minimi muscle moves the little finger to allow the opposition of the hand in which the pad of the thumb touches the pad of the little finger. This is a critical test in clinical neurology. The motion created by the opponens digiti minimi muscle is a combination of palmar rotation, flexion, and abduction of the little finger. The flexor digiti minimi brevis muscle will flex the little finger at the metacarpophalangeal joint. The palmaris brevis muscle serves a minor function within the hypothenar eminence. The palmaris brevis muscle increases grip strength and protects the ulnar nerve as it enters the hand.[1][2]
The origins and attachments of the hypothenar muscles vary slightly, but they have one thing in common. They cause movement of the little finger. The abductor digiti minimi muscle derives its origin from the pisiform carpal bone, dorsal aponeurosis, and the tendon of the flexor carpal ulnaris muscle. The abductor digiti minimi muscle attaches to the little finger at the base of the proximal phalanx. The flexor digiti minimi brevis muscle originates from the hamate carpal bone and the transverse carpal ligament (flexor retinaculum). The flexor digiti minimi brevis muscle also attaches at the proximal phalanx of the little finger. The opponens digiti minimi muscle also originates from the hamate carpal bone and the transverse carpal ligament, similar to the origin of the flexor digiti minimi brevis muscle. But the opponens digiti minimi muscle attaches to the medial side of the proximal phalanx. The palmaris brevis muscle originates from the transverse carpal ligament and inserts into the skin on the ulnar side of the palm.[2]
Embryology
The thenar eminence will develop mainly from the ectoderm and mesoderm germ layers. The overlying skin and nerve innervation derive from the ectoderm layer. The neural crest cells from the ectodermal layer will form the ulnar nerve. The development of the hypothenar muscles is similar to the development of most muscles. The mesenchymal tissue from the mesodermal germ layer will differentiate into the muscles. The mesenchymal tissue will also form the blood vessels that perfuse the hypothenar eminence. The mesenchyme will form the ulnar artery and its branches to perfuse the hypothenar eminence.
Blood Supply and Lymphatics
The blood supply to the hypothenar eminence originates from the ulnar artery. The ulnar artery enters the hand and forms the superficial palmar arterial arch. This arch will be responsible for supplying the main blood supply to the hypothenar eminence. The radial artery also provides collateral blood flow to the hypothenar eminence through the deep palmar arterial arch of the hand. The deep palmar arterial arch anastomoses with the superficial palmar arterial arch or the ulnar artery. These anastomoses will provide collateral blood flow to the hypothenar eminence if the blood flow of the ulnar artery is insufficient.[3]
The lymphatic drainage of the thenar eminence will drain toward the cubital fossa. The cubital fossa contains cubital lymph nodes. Then the lymph fluid will drain toward the axilla and eventually return to either the right lymphatic duct or the thoracic duct. The right lymphatic duct will drain the right hypothenar eminence, while the thoracic duct will drain the left eminence.
Nerves
The innervation of the hypothenar eminence is entirely via the ulnar nerve (C8 and T1 spinal roots). The ulnar will travel in the Guyon canal (formed between the hook of the hamate and the pisiform). The ulnar nerve will travel superficially to the transverse carpal ligament but under the palmaris brevis muscle. The palmaris brevis muscle protects the ulnar nerve as the nerve enters the hand.
Muscles
Muscles in the hypothenar eminence:
- Flexor digiti minimi muscle
- Abductor digiti minimi muscle
- Opponens digiti minimi muscles
- Palmaris brevis muscle
All these muscles in the hypothenar eminence contribute to the movements of the little finger and the mound-like structure on the palmar side of the hand.
Physiologic Variants
The origins and attachments of the hypothenar muscles may vary slightly, but the hypothenar eminence itself is consistent. The hypothenar eminence may consist of three or four muscles depending on the individual. Some individuals lack the palmaris brevis muscle. The attachment of the palmaris brevis muscle can vary also. The most common attachment for the palmaris brevis muscle is the skin on the ulnar side of the hand. The palmaris brevis muscle can sometimes be found attached to the pisiform bone.[4]
Surgical Considerations
It is essential to comprehend the anatomy of the hypothenar eminence when performing hand surgery in this region. Knowing the relationship between the nerves, blood vessels, muscles, and bones allows for a safe and optimal approach during hand surgery.
When hand reconstruction involves the ulnar artery, the collateral blood supply should be evaluated for sufficiency — the modified Allen test may be used to determine the collateral blood to the hypothenar eminence. Collateral blood flow should be assessed because if the hypothenar eminence is left with inadequate perfusion post-operatively, the muscles, nerves, and tissues of the region may undergo ischemic necrosis.
Repairing the ulnar nerve in "handlebar palsy" requires the surgeon to know the relationship between the hook of the hamate and pisiform bones. The ulnar nerve will pass between the hook of the hamate and the pisiform bone (Guyon canal). During the repair, it is crucial to release the compression of the ulnar nerve without damaging it. If damage to the ulnar nerve occurs, there will be atrophy of the hypothenar eminence along with loss of sensory and motor function in the region innervated by the ulnar nerve.[5]
Clinical Significance
The ulnar nerve innervates the hypothenar region. If the ulnar is damaged or compromised, the muscles in the hypothenar eminence will atrophy. The atrophy of the hypothenar eminence can indicate a compromise of the ulnar nerve proximal to the hand.[6]
As the ulnar nerve passes between the hook of the hamate and the pisiform bone (the Guyon canal), it can become compressed. Individuals that apply direct pressure to the Guyon canal, such as cyclists, can damage the ulnar nerve. Damage to the ulnar nerve will manifest as atrophy, numbness, tingling, and pain in the hypothenar eminence along with the fourth and fifth digits. This condition is similar to "carpal tunnel syndrome," but it affects the ulnar nerve.[7]
Hypothenar Hammer Syndrome
Repetitive use of the hypothenar prominence as a hammer can lead to an aneurysm or thrombosis of the ulnar artery. This condition has been termed the hypothenar hammer syndrome.[8] The hypothenar hammer syndrome was described by von Rosen in 1934 and Conn in 1970.[9] This syndrome is likely to occur in middle-aged men with repetitive occupational motion injuries following using the hand, especially the hypothenar eminence as a hammer.[9][10]
This condition can also occur in workers who use hammers and similar tools repetitively. However, a case of a 79-year-old woman who developed hypothenar hammer syndrome without a history of trauma has been reported.[8] If the blood supply becomes compromised, there will be necrosis of the hypothenar eminence.[11][12] A case of a patient who had both hypothenar hammer syndrome and thenar hammer syndrome combined with Reynaud syndrome has been reported.[13]
Compression of the ulnar artery against the hook of the hamate bone just distal to the Guyon canal results in thrombosis.[8] Patients with hypothenar hammer syndrome present with pain and pallor, especially involving the little finger and the medial half of the ring finger.[10] This is the ulnar nerve distribution. The condition may also affect other fingers, as these are supplied from the superficial palmar arterial arch from the ulnar artery. Other findings include cyanosis and sensitivity to cold. The condition is usually diagnosed by angiography.
The mechanism of hypothenar hammer syndrome is as follows. Repetitive tunica intima trauma stimulates vasospasm and platelet aggregation resulting in intimal hyperplasia, leading to thrombosis in adjacent vascular branches of the ulnar artery. Medial and intimal wall degeneration can involve fibromuscular dysplasia that underlies the tendency of the tunica intima towards hyperplasia and thrombosis.[10] Aneurysms or pseudoaneurysms may occur. If an aneurysm forms, it may compress the adjacent ulnar nerve, resulting in paresthesias and pain.[9]
Treatment begins with oral antiplatelets. Treatment involves cessation of smoking by the patient, modification of activities, pharmacological treatment, arterial coiling, and thrombin injection. More serious cases may require the removal of the affected vessel, especially when an aneurysm is present, or the condition is severe.[9] Arterial grafts have been used in the treatment of hypothenar hammer syndrome.[14]
Recurrence is a concern after surgical treatment.[8]
Other Issues
The ulnar artery predominantly perfuses the hypothenar eminence and receives innervation from the ulnar nerve. If there were to be any compromise to the nerve or artery proximally in the arm, the patient would present with symptoms of damage manifested through the resting and active presentation of the hand.[15]
The hypothenar eminence also corresponds to the dermatome level for C8, except that the C8 dermatome involves both sides of the ring and little fingers. Moreover, the C8 dermatome involves the medial forearm. The ulnar nerve does not cross the wrist. If there is a lesion of the ulnar nerve due to inadequate blood supply, paresthesias may result. These involve the loss of fine touch fibers and continuous hyperactivity of the pain fibers (feeling of pins and needles and/or paraesthesia). This neurological finding could indicate a lesion affecting the C8 spinal root on the ipsilateral side.[16]
Palmaris Brevis Syndrome
Palmaris brevis syndrome manifests as repeated involuntary contractions of the palmaris brevis.[17] Excessive repetitive use underlies the condition, as in a reported case involving repetitive use of pipettes or a computer mouse.[17]
Botulinum toxin can be used to selectively block the palmaris brevis without affecting the muscles of the hypothenar eminence. The condition has been postulated to involve the superficial branch of the ulnar nerve manifesting as the involvement of all the little finger and the medial half of the ring finger. Note the similarity of this pattern to the C8 dermatome/myotome.
The differential diagnosis includes radiculopathy involving the C8 or T1 spinal roots, ulnar neuropathy, myotonia, inflammatory arthritic disease, and Dupuytren contracture.[17]
Ulnar Nerve Involvement in Guyon Canal
The ulnar nerve has been reported to be compressed by a large hypothenar cyst in the Guyon canal.[18]