Introduction
The glenohumeral joint is structurally a ball-and-socket joint and functionally is considered a diarthrodial, multiaxial, joint.[1] The glenohumeral articulation involves the humeral head with the glenoid cavity of the scapula, and it represents the major articulation of the shoulder girdle.[2] The latter also includes minor articulations of the sternoclavicular (SC), acromioclavicular (AC), and scapulothoracic joints.[3][1][4] The glenohumeral joint ranks as the most mobile joint of the human body.[2][5] The static and dynamic stabilizing structures allow for extreme degrees of motion in multiple planes of the body that predisposes the joint to instability events.
Structure and Function
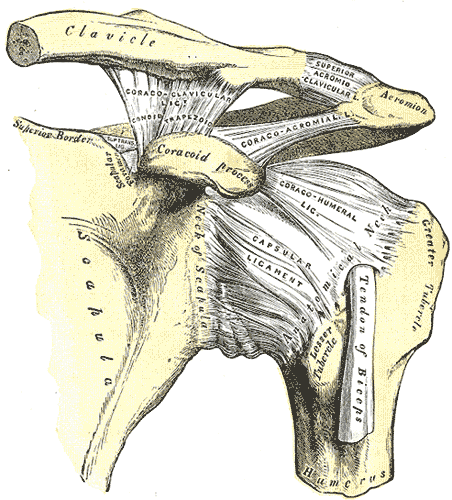
The glenohumeral joint is a ball and socket joint that includes a complex, dynamic, articulation between the glenoid of the scapula and the proximal humerus. Specifically, it is the head of the humerus that contacts the glenoid cavity (or fossa) of the scapula. The articulating surfaces of both have a lining of articular cartilage. The glenoid cavity is a shallow osseous element that is structurally deepened by a fibrocartilagenous rim, the glenoid labrum, that spans the osseous periphery of the vault. The labrum is continuous with the tendon of the biceps brachii at its superior aspect.[1]
Due to the loose joint capsule, and the relative size of the humeral head compared to the shallow glenoid fossa (4:1 ratio in surface area), it is one of the most mobile joints in the human body. This increased mobility contributes to it being the most commonly dislocated joint.[5]
The glenohumeral joint is enclosed by a joint capsule that encapsulates the structures of the joint in a fibrous sheath. Structurally the joint capsule wraps around the anatomic neck of the humerus to the rim of the glenoid fossa. While the joint capsule itself is a contiguous supportive structure surrounding the articulating elements, the capsulolabral complexes include important characteristic thickened bands that constitute the glenohumeral ligaments. First described in 1829, the glenohumeral ligaments do not act as traditional ligaments that carry a pure tensile force along their length, but rather, the glenohumeral ligaments become taut at varying positions of abduction and humeral rotation.[6][7] A synovial membrane forms the lining of the inner surface of the joint capsule. This membrane produces synovial fluid to reduce friction between the articular surfaces.[8]
In addition to the synovial fluid reducing friction within the joint, there are multiple synovial bursae present as well. These bursae functionally act as a cushion between joint structures, such as tendons. The most clinically significant are the subacromial and subscapular bursae. There are numerous, including:
- Subacromial/subdeltoid bursa - This structure lies between the deltoid muscle and joint capsule in the superolateral aspect of the joint. It is superficial to the supraspinatus tendon. This bursa reduces friction underneath the deltoid muscle, allowing an increased range of motion. This bursa, excluding anatomic variants, does not usually communicate with the shoulder joint itself.
- Subcoracoid bursa - This bursa is between the coracoid process and the subscapularis.
- Subscapular bursa - is located between the tendon of the subscapularis muscle and the capsule. It functions to reduces frictional damage to the subscapularis muscle during movement of the glenohumeral joint, particularly during internal rotation.
Static stabilizing structures include the osseous articular anatomy and joint congruity, the glenoid labrum, the glenohumeral ligaments, joint capsule, and negative intraarticular pressure [9]:
- Glenohumeral ligaments- Composed of a superior, middle, and inferior ligament, these three ligaments combine to form the glenohumeral joint capsule connecting the glenoid fossa to the humerus. Due to their location, they protect the shoulder and prevent it from dislocating anteriorly — this group of ligaments functions as the primary stabilizers of the joint.
- Coracoclavicular ligament – This ligament is composed of the conoid and trapezoid ligaments and spans from the coracoid process to the clavicle. It functions to maintain the position of the clavicle in conjunction with the acromioclavicular ligament. Strong forces can rupture these ligaments during acromioclavicular joint injuries.
- Coracohumeral ligament – This ligament supports the superior aspect of the joint capsule. It is a dense fibrous structure connecting the base of the coracoid process to the greater and lesser tuberosities. At its origin, the ligament is thin and broad, measuring about 2 cm in diameter at the base of the coracoid. Laterally, the CHL separates into two distinct bands that envelope the Long Head Biceps tendon at the proximal extent of the bicipital groove.
Dynamic stabilizing structures include the Long head biceps tendon, rotator cuff muscles, the rotator interval, and the periscapular muscles.
Soft tissue pulley system and Long head of the biceps tendon (LHBT) [10][11]
- The subscapularis has superficial and deep fibers that envelope the bicipital groove, creating the “roof” and “floor,” respectively. These fibers also coalesce with those from the supraspinatus and superior glenohumeral ligament/coracohumeral ligament complex. These structures attach intimately at the lesser tuberosity to create the proximal and medial aspect of the pulley system, with soft tissue extensions serving to further envelope the LHBT in the bicipital groove. Once the LHBT exits the groove, it takes a 30- to 40-degree turn as it heads toward the supraglenoid tubercle and glenoid labrum. Thus, the proximal soft tissue elements of the groove are especially critical for the overall stability of the entire biceps complex.
The glenohumeral joint possesses the capability of allowing an extreme range of motion in multiple planes.[12]
- Flexion – Defined as bringing the upper limb anterior in the sagittal plane. The usual range of motion is 180 degrees. The main flexors of the shoulder are the anterior deltoid, coracobrachialis, and pectoralis major. Biceps brachii also weakly assists in this action.
- Extension—Defined as bringing the upper limb posterior in a sagittal plane. The normal range of motion is 45 to 60 degrees. The main extensors of the shoulder are the posterior deltoid, latissimus dorsi, and teres major.
- Internal rotation—Defined as rotation toward the midline along a vertical axis. The normal range of motion is 70 to 90 degrees. The internal rotation muscles are the subscapularis, pectoralis major, latissimus dorsi, teres major, and the anterior aspect of the deltoid.
- External rotation - Defined as rotation away from the midline along a vertical axis. The normal range of motion is 90 degrees. Primarily infraspinatus and teres minor are responsible for the motion.
- Adduction – Defined as bringing the upper limb towards the midline in the coronal plane. Pectoralis major, latissimus dorsi, and teres major are the muscles primarily responsible for shoulder adduction.
- Abduction - Defined as bringing the upper limb away from the midline in the coronal plane. The normal range of motion is 150 degrees. Due to the ability to differentiate several pathologies by the range of motion of the glenohumeral joint in this plane of motion, it is essential to understand how different muscles contribute to this action.[12]
I. The supraspinatus is responsible for the first 0 to 15 degrees of abduction[13]
II. The middle fibers of the deltoid are responsible for approximately 15 to 90 degrees of abduction following[14]
III. Scapular rotation due to the actions of the trapezius and serratus anterior allow for abduction beyond 90 degrees
Embryology
The development of the skeletal shoulder consists of both forms of ossification processes. The clavicle undergoes intramembranous ossification, which is the direct laying down of bone into the mesenchyme. The rest of the bony structures of the shoulder form by endochondral ossification.[15] The mesoderm germ layer forms nearly all of the connective tissues of the musculoskeletal system, including the glenohumeral joint. Musculoskeletal and limb abnormalities, due to both environmental and genetic contributions, are one of the largest groups of congenital abnormalities.
Blood Supply and Lymphatics
The glenohumeral joint receives vascular supply via the posterior and anterior circumflex humeral arteries, both of which are branches of the axillary artery. The predominant arterial blood supply to the humeral head is via the posterior humeral circumflex artery.[4][16] The arcuate artery is the extension/continuation of the ascending branch of the anterior humeral circumflex. It enters the bicipital groove and supplies most of the humeral head. A branch of the thyrocervical trunk, the subscapular arteries, and its branches, also contribute to the blood supply of the shoulder.[17]
The majority of the lymph nodes in the upper extremity are located within the axilla. These can be divided based on location into five main groups: pectoral, subscapular, humeral, central, and apical. Efferent vessels coming from the apical axillary nodes travel through the cervico-axillary canal and then converge to form the subclavian lymphatic trunk. This trunk will either continue to enter the right venous angle or drain directly into the thoracic duct on the right and left, respectively. Removal and analysis of axillary lymph nodes is often an essential tool in the staging of breast cancers. The interruption of lymphatic drainage from the upper limb can, however, result in lymphoedema, a condition where accumulated lymph in the subcutaneous tissue leads to painful swelling of the upper limb.[18]
Nerves
Innervation of the glenohumeral joint is a function of the suprascapular, lateral pectoral, and axillary nerves. All of the nerves supplying the glenohumeral joint originate from the brachial plexus, which is a network of nerves formed by the ventral rami of the lower four cervical nerves and the first thoracic nerve (C5, C6, C7, C8, and T1). The anatomy of the axillary nerve is critical as it is close to the glenohumeral joint. The axillary nerve arises from the posterior cord of the brachial plexus, courses along the subscapularis to its inferior edge, and then passes closely along the inferior glenohumeral joint capsule. It then courses posterior to the humerus, wraps around the surgical neck of the humerus with the posterior circumflex artery, running in the deep deltoid fascia.
Muscles
The four muscles that constitute the rotator cuff are the supraspinatus, infraspinatus, subscapularis, and teres minor. The primary biomechanical role of the rotator cuff is stabilizing the glenohumeral joint by compressing the humeral head against the glenoid. The rotator cuff muscles thus act as dynamic stabilizers of the glenohumeral joint.[19][20] In addition to the rotator cuff, the LHBT has a controversial contribution and overall role in glenohumeral joint stability. The current consensus agreement is that the stabilizing role of the LHBT in regards to the glenohumeral joint becomes more important and/or relevant in the setting of rotator cuff dysfunction.[11][10][21]
The supraspinatus primarily abducts the shoulder and is responsible for the initial 15 degrees of abduction. The infraspinatus and teres minor aid in external rotation of the shoulder. The subscapularis muscle aids in internal rotation of the shoulder. The supraspinatus and infraspinatus muscles are innervated by the suprascapular nerve. The teres minor is innervated by the axillary nerve and subscapularis by the subscapular nerve.
Clinical Significance
Shoulder dislocations
The glenohumeral joint is by far the most commonly dislocated joint of the body, accounting for up to 45% of dislocations. Anterior dislocation accounts for 96% of cases and is often the result of a force directed to the shoulder joint while the arm is in abduction and external rotation. Posterior dislocation is the second most common direction of dislocation, accounting for 2% to 4% of cases. Posterior dislocations are usually due to indirect mechanisms such as electric shock or convulsions, causing contraction of the relatively stronger internal rotators of the shoulder (latissimus dorsi, pectoralis major, and subscapularis muscles).
Glenohumeral joint dislocation has an incidence of approximately 17 per 100,000 a year, with a peak incidence among males in the 21 to 30 year age range and females in the 61 to 80 year age range. Treatment typically involves analgesics and closed reduction, with some patients requiring subsequent surgical correction, especially those with concurrent soft tissue injuries resulting in recurrent shoulder dislocations.[22] The axillary nerve courses within close proximity of the glenohumeral joint and wrap around the neck of the humerus, and can incur damage during dislocation or subsequent attempts at reduction of the dislocated joint. Injury to the axillary nerves causes a loss of sensation over the lateral shoulder and paralysis of the deltoid. Hill-Sachs lesions (impaction fracture of the posterolateral humeral head against anteroinferior glenoid) and Bankart lesions (detachment of anteroinferior labrum with or without an avulsion fracture) can also occur following anterior dislocation. The recurrence rate of glenohumeral joint dislocation is approximately 50% on average; however, there is a significant increase in the risk of reoccurrence with a younger age of initial dislocation.[23]
Adhesive capsulitis
Adhesive capsulitis is a disorder of unclear cause in which the glenohumeral capsule becomes inflamed and stiff, significantly restricting motion and can cause chronic pain. The pain is usually constant, worse at night. Incidence is approximately 3% of the general population, with some controversy over this number due to concerns of over-diagnosis of this disorder. It occurs more commonly in women aged 40 to 70 years of age.[24] Risk factors for adhesive capsulitis include diabetes mellitus, connective tissue diseases, thyroid disease, and heart disease. It has associations as an adverse effect of specific highly active antiretroviral therapies as well.[25] Management consists of physical and occupational therapy, medication (analgesics/NSAIDs), intraarticular steroid injection, and, in rare cases, surgery. Manipulation under general anesthesia may also be an option, which disrupts the scar tissue and adhesions within the joint. Over time, most people regain approximately 90% of their shoulder range of motion.
Rotator cuff injuries [19]
The tendons of the rotator cuff are often under heavy strain as they function in stabilizing the glenohumeral joint. Therefore, the pathology of these rotator cuff tendons is relatively common. Rotator cuff conditions are the most common source of shoulder pain for primary care office visits.[26] A wide spectrum of pathology exists, including sub-acromial bursitis, rotator cuff tendinitis, shoulder impingement, and rotator cuff tears. Patients with impingements/subacromial bursitis will often complain of pain with overhead activity. Most patients will have a resolution of their symptoms with properly designed and performed physical therapy programs. If patients do not improve after a period of conservative management, however, evaluation by an orthopedic surgeon and/or sports medicine specialist is often necessary. Rotator cuff tendon tears can be chronic due to tendon degeneration or shoulder impingement, or it can be acute following an injury. It could be partial thickness tear or full-thickness tear.