Introduction
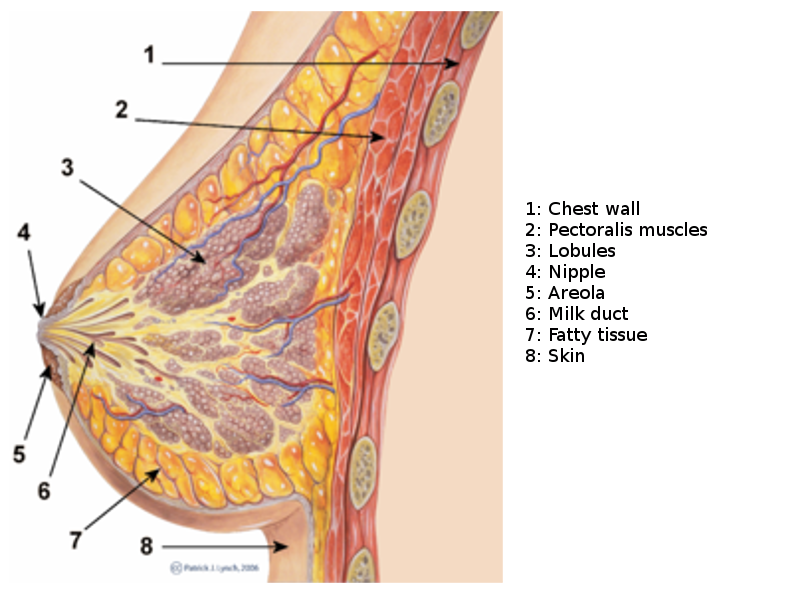
The anatomy of the breast must be well understood to understand the disorders that affect this organ and develop a plan for breast surgery. When examined, some degree of asymmetry is noted in most breasts. Other deformities include kyphosis, scoliosis, or some type of pectus deformity.
The majority of the breast consists of glandular (milk-producing) and fatty tissues. However, the ratio of the glandular to fatty tissue varies among individuals. The breast is heavily influenced by the sex hormone estrogen. As menopause approaches, the levels of estrogen declines which also decreases the glandular tissues.
The pectoralis major muscle forms the base of the breast, which extends from the second to sixth rib early in life but may extend to below the sixth rib as the breast matures and sags. The breast is anchored to the pectoralis major fascia by the Cooper ligaments. However, these ligaments are flexible and allow for movements in the breast. In most women, the Cooper ligaments become stretched with time and age, eventually resulting in a ptotic breast. Because of gravity, the lower pole of the breast is fuller than the upper pole. At the lateral edges of the breast, the tail of Spence extends in the axilla.
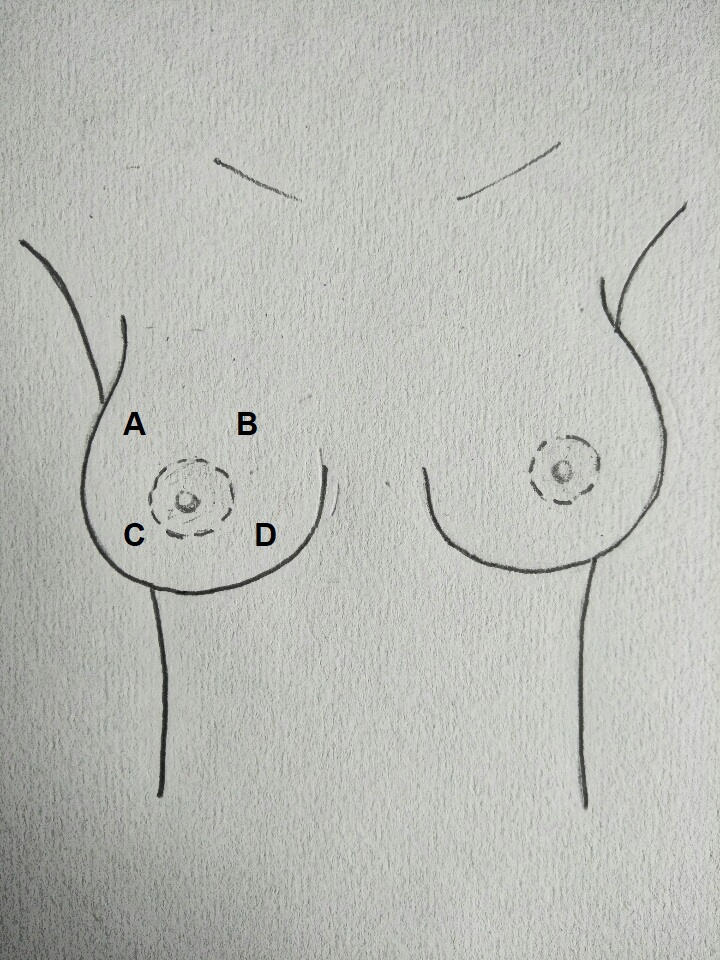
The nipple is usually located just superior to the inframammary crease and is consistently found level along the midclavicular line and the fourth rib.[1][2][3]
Glands
The underlying breast is made of glandular (milk-producing) and fatty tissue. The ratio of fat versus glandular varies depending on age, post-menopausal, post-partum, or pregnancy status. At the onset of menopause, a decline in the levels of estrogen results in a decrease in glandular tissue and an increase in fatty tissue.
Structure and Function
The nipple plays an important role in breastfeeding. The minimal nipple length required for successful breastfeeding is about seven millimeters. However, the nipple shows great variation in topography; it can be flat, short, and even inverted, which can hamper breastfeeding in some women.
Embryology
Breast development or mastogenesis starts around the sixth week of gestation. The milk line, which is a distinct linear elevation, appears around the seventh week. At the end of the eighth week, the rudimentary breast forms from the thickened white line and will eventually become the mature breast. Throughout embryogenesis, there is a proliferation of basal cells. At about 30 weeks of gestation, occlusion of the papillary bag results in the formation of the nipple areolar complex. The final nipple will appear at about 38 to 40 weeks.
Blood Supply and Lymphatics
The breast skin receives its blood supply from the subdermal plexus; these tiny blood vessels, in turn, communicate with deep underlying arterioles which supply the breast parenchyma. Blood is supplied to the breast from the following vessels:
- The thoracoacromial artery
- Internal mammary perforators (second to fifth)
- Lateral thoracic artery
- Thoracodorsal artery
- Terminal branches of the intercostal perforators (third to eighth)
Overall, at least 60% of the blood supply is from the superomedial perforators which come off the internal mammary artery.
The breast also has profuse venous drainage divided into the superficial and deep veins. The superficial veins are found along the anterior surface of the fascia; these veins follow the areola path under the nipple areolar complex, often referred to as the venous plexus of Haller. Deep inside the breast are many large veins which drain into the chest wall veins.
Lymphatic Drainage
The breast also has extensive lymphatic drainage that runs both superficially and deep within the breast. The superficial lymphatics are the areolar and subareolar plexus. The latter also receives lymphatics from glandular tissues. The superficial lymphatics continue posteriorly and medially and eventually reach the axillary lymph nodes.
Nerves
Sensory innervation to the breast is derived from branches of the intercostal nerves T3-T5. Other nerves that supply sensory innervation include the lower cervical plexus. Sensation to the nipple is derived from the lateral cutaneous branch of T4.
Muscles
On the lateral and medial wall of the chest, the base of the breast sits over the serratus anterior and external oblique muscles.
- The pectoralis major is a broad, fan-like muscle that originates from the lateral sternum and clavicle and inserts at the humeral head. The muscle receives most of its blood from branches of the internal mammary and thoracoacromial arteries. The breasts lie over the pectoralis muscle and uppermost portion of the rectus abdominis muscle between the second and sixth ribs. The breast is anchored to the pectoralis major by suspensory ligaments of Cooper, which traverse throughout the breast tissue from the dermis of the skin all the way down to the pectoralis fascia. Cooper ligaments are not taut and help the breasts maintain their natural mobility. With advancing age, there is a loss of tension in the ligaments, which results in breast ptosis. The pectoralis muscle is frequently utilized in reconstructive plastic surgery as it can provide good muscle coverage for a breast implant.
- The serratus anterior is another fan-shaped muscle that runs along the lateral wall of the chest wall. The serratus anterior is supplied by branches of the thoracodorsal and lateral thoracic arteries. The muscle is innervated by the long thoracic nerve. If the long thoracic nerve is damaged during axillary dissection, it can result in winging of the scapula.
- The rectus abdominis demarcates the inferior border of the breast. The muscle is supplied by the inferior and superior epigastric vessels. In women who have surgery for breast cancer, the rectus abdominis muscle flap (TRAM) based on the superior epigastric flap is sometimes utilized.
- The external oblique is a fan-shaped muscle found on the anterolateral aspect of the thoracic wall. The muscle has a segmental blood supply which originates from the inferior intercostal vessels. The muscle borders the inferolateral wall of the breast.
- In young women, the location of the nipple is found just superior to the inframammary crease at the level of the fourth rib and just lateral to the midclavicular line.
Physiologic Variants
Several anomalies of the nipple have been recognized, including the following:[4]
- An accessory nipple is reported to occur in 1% to 4% of the population and has an equal incidence in both females and males. The accessory nipple is usually located in the inframammary area and is prone to the same medical disorders as the typical nipple. The accessory nipple can be excised if it causes anxiety, poor cosmesis, discomfort, or limits arm movement.
- Athelia or the congenital absence of the nipple areolar complex does occur in patients with Poland syndrome. The condition is also associated with an underdeveloped breast.
- Amastia is known as the complete absence of all breast tissue except for the nipple areolar complex.
- The inverted nipple is a common anomaly, where the nipple is retracted into the breast instead of pointing outwards. In some cases, the inverted nipple may alternatively protrude and retract. The inverted nipple can occur in men and women. The inverted nipple does make it difficult to breastfeed.
Surgical Considerations
In women with breast cancer, several types of surgical procedures are done including a lumpectomy and modified mastectomy. Unlike in the past, total or radical mastectomy is done less frequently. Several studies have shown that skin-sparing or modified radical mastectomies are effective in the treatment of breast cancer. However, there is a small risk of breast cancer recurrence.[5][6][7][8]
Clinical Significance
The breast is susceptible to many benign and malignant disorders, including the following:
- Puerperal mastitis
- Mastalgia
- Fibrocystic breast changes
- Fat necrosis
- Breast abscess
- Galactorrhea
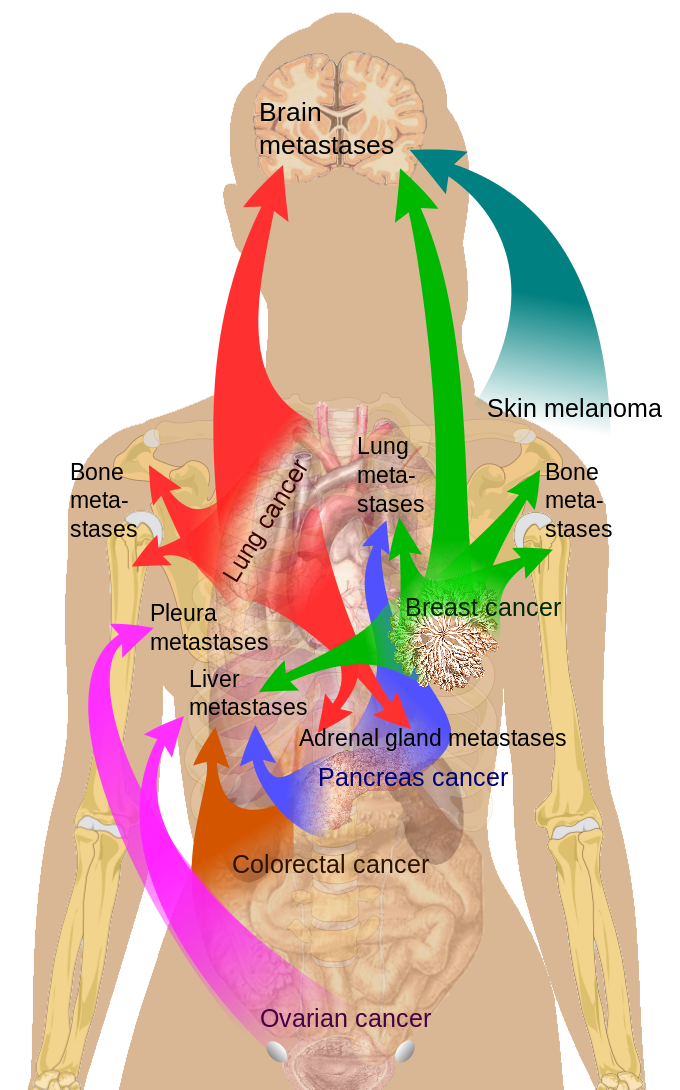
Breast Cancer
The leading cause of death in women is breast cancer. In addition, breast cancer is one of the most common malignancies of women worldwide. Many risk factors for breast cancer have been identified, but it is important to ensure that women over the age of 45 have regular mammograms, eat a healthy diet, exercise, and refrain from smoking.
Male Breasts
Male breasts develop from the same embryological cells as females. However, males have a lower production of estrogens and a higher production of androgens. In some men, the breasts may grow quite large as a consequence of an imbalance between estrogens and testosterone. About two-thirds of boys will have some type of temporary gynecomastia which resolves within 24 months. Sometimes gynecomastia can be caused by medications like digoxin and spironolactone.
Other Issues
Cosmetic surgery is often performed to augment or reduce the size of the breasts. In other cases, plastic surgery is done to reconstruct a deformed breast, especially in women who undergo surgery for breast cancer. Both breast lifts and breast augmentation are strictly cosmetic procedures, whereas a breast reduction in women is often done for medical reasons (back or neck pain). Sometimes, breast reconstruction is done for asymmetrical breasts.
Breast augmentation, when done properly, does not interfere with a woman's ability to breastfeed. However, breast reduction surgery is known to damage the nerves in the nipple areolar complex and lead to a decreased sensation. In addition, many women who have had breast reduction surgery may not be able to breastfeed because the glandular tissues have been removed. Finally, it is important to know that breast implants can interfere with mammography.[9]