Continuing Education Activity
Advancing wavelike epitheliopathy (AWE) is a chronic or recurrent disorder characterized by well-demarcated, wavelike plaques of coarse, thickened corneal epithelium. This activity reviews the etiology, epidemiology, and pathophysiology of advancing wavelike epitheliopathy. It also summarizes current recommendations on the evaluation, treatment, and management of patients with this condition. It discusses the role of the interprofessional team.
Objectives:
- Describe the pathophysiology of advancing wavelike epitheliopathy.
- Explain the common ocular exam findings associated with advancing wavelike epitheliopathy.
- Identify the treatment considerations for patients with advancing wavelike epitheliopathy.
- Explain the importance of improving care coordination amongst the interprofessional team to enhance the delivery of care for patients with advancing wavelike epitheliopathy.
Introduction
Advancing wavelike epitheliopathy (AWE) is a chronic or recurrent disorder characterized by well-demarcated, wavelike plaques of coarse, thickened corneal epithelium. This process characteristically extends from the superior limbus and spreads toward the visual axis.[1] Some cases also show that they may originate from the inferior limbus.[2] Corneal epithelial scrapings show no signs of dysplasia or irregularity, and the conjunctiva remains unaffected.[1] AWE can be unilateral or bilateral.[1][2]
Etiology
While the exact cause of advancing wavelike epitheliopathy remains unclear, it appears that it may occur in response to irritation or insult to the corneal epithelium. Possible stimuli include prior ocular surgery, contact lens use, topical ocular medications, ocular exposure to toxins or irritants, or underlying inflammatory or dermatological disorders.[1][2][3][4]
Specific possible medications include:[1][2]
- Topical antiglaucoma medications
- 5-fluorouracil
- Topical acyclovir
- Contact lens solution
Specific possible disease processes include:[1]
- Ocular cicatricial pemphigoid
- Acne rosacea
- Atopic dermatitis
Epidemiology
Advancing wavelike epitheliopathy usually presents after the age of 40, can be monocular or binocular, and occurs equally in males and females.[1][2][5]
Pathophysiology
Very little is known about the underlying mechanism of advancing wavelike epitheliopathy, which appears to be multifactorial. D’Aversa et al., the first to report on this disease, suggest that it may stem from abnormal parakeratotic limbal epithelial stem cells proliferating and migrating onto the cornea, leading to the characteristic epithelial waves.[1] This process presents similarly to partial limbal stem cell deficiency or dysfunction, which lends credence to the theory that these may arise from similar disease processes. Patients with limbal stem cell deficiency (LCSD) also present with symptoms of blurry vision and corneal irritation.[6] LCSD often exhibits epitheliopathy arising from the involved limbus, most commonly at the superior limbus, as does AWE.[7][8][9] LCSD may occur through similar stimuli, including trauma, surgery, contact lens use, and topical antiglaucoma medications.[6][7][8][9][10][11]
Histopathology
Pathology shows unremarkable epithelium on H&E staining. Epithelial dysplasia is not present on the histological exam of the debrided epithelium.[2][5][1] Full-thickness biopsy shows parakeratosis of the conjunctival epithelium and underlying focal mononuclear cell infiltrates, which may compress or extend into the overlying epithelium.[5] One study showed a reduction in the subepithelial nerve plexus compared to healthy eyes.[4]
History and Physical
Patients with AWE present with decreased visual acuity, which chronically progresses or relapses and with periods of remission over months to years. Patients also complain of foreign body sensation, tearing, redness, or irritation, although some may be asymptomatic if the lesion is small and outside the visual axis. History of ocular surgery or trauma, topical ocular medications, atopic dermatitis, or acne rosacea have all been associated with the disease process.[1][5][2]
The slit-lamp exam with fluorescein staining along with confocal microscopy are tools for diagnosis and show specific findings as described below.
Evaluation
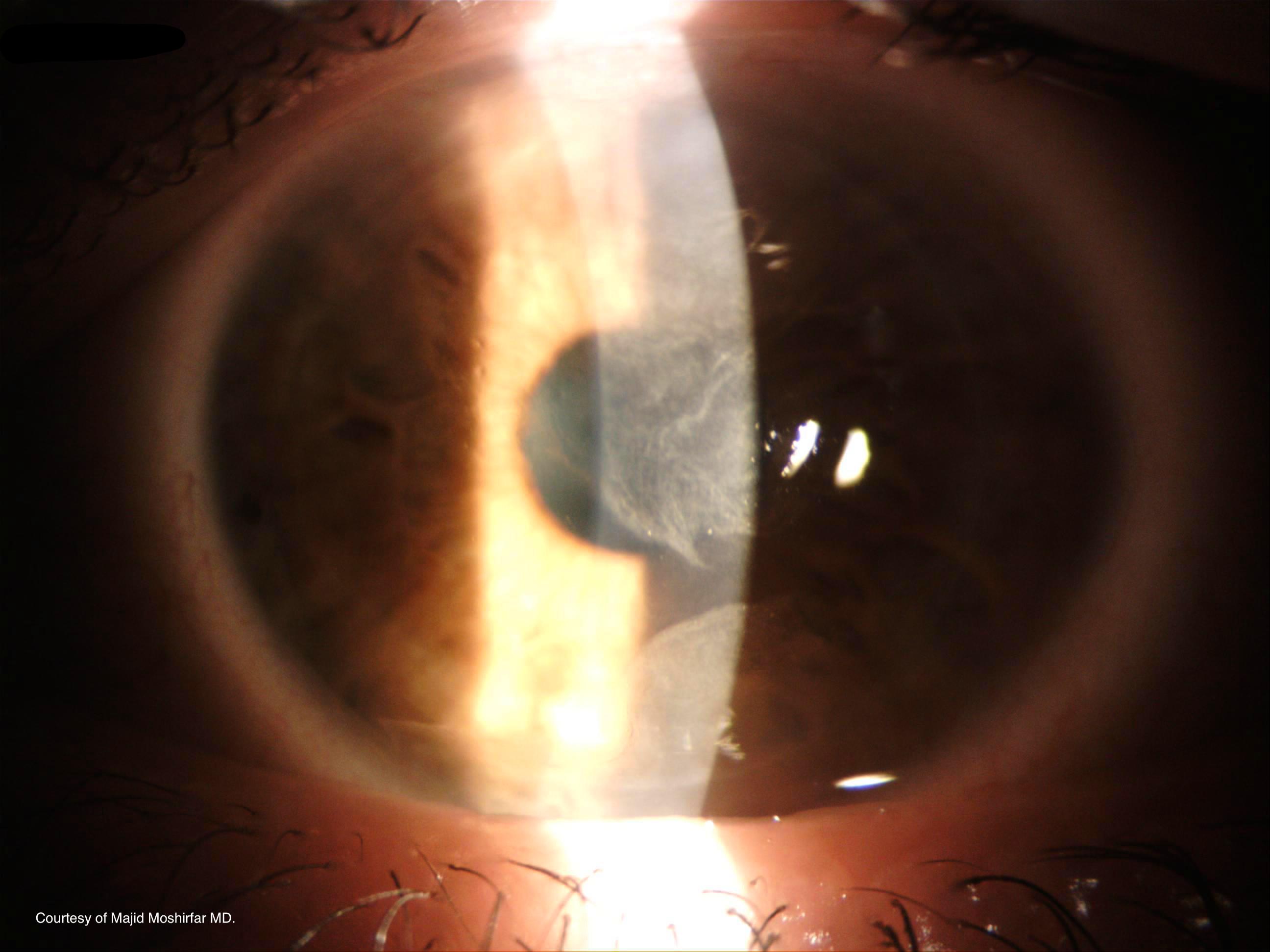
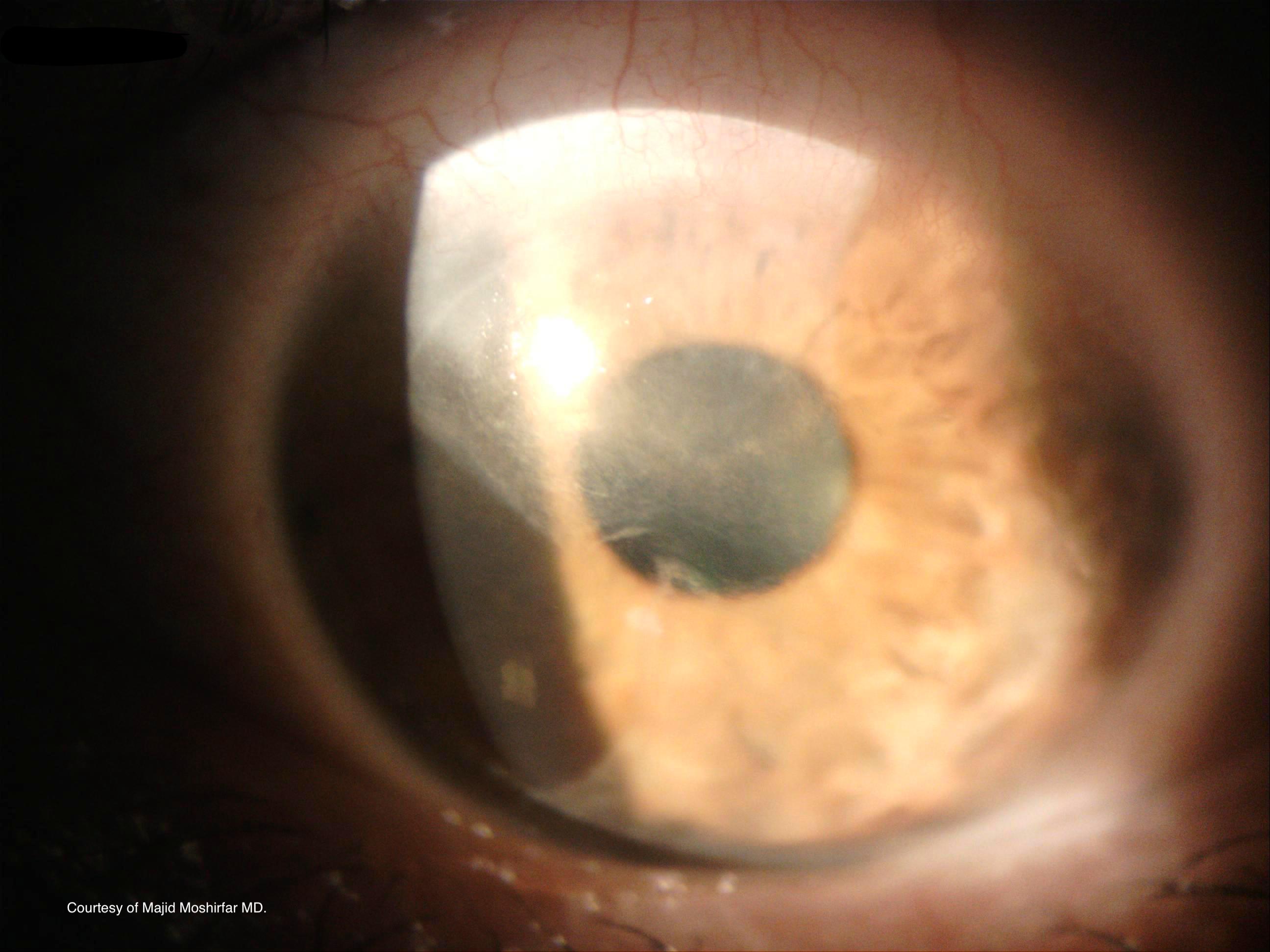
The diagnosis of advancing wavelike epitheliopathy is made clinically with the use of a slit lamp and confocal microscopy. Slit-lamp examination reveals a well-demarcated, wavelike plaque progressing from the superior limbus. Sclerotic scatter reveals a granular texture and distinct lesion margins (Figure 1).[1][2] A subepithelial haze may be present with no discrete opacities or infiltrates within the patches (Figure 2). Fluorescein staining shows a punctate pattern with well-defined borders.[1][2][5] Confocal microscopy shows atypical, elongated cells oriented centripetally with hyperreflective nuclei, a large nuclear to cytoplasmic ratio, and loss of visible cellular borders in the basal epithelium.[1][2]
Treatment / Management
The accepted course of treatment for advancing wavelike epitheliopathy is the elimination of identifiable offending agents, debridement of the abnormal epithelium, and empiric application of a 1% silver nitrate solution to the superior corneoscleral limbus.[1][5]
Most sterile compounding pharmacies are able to formulate this solution, as it is not available in a premade form. For treatment, the affected eye should be anesthetized with proparacaine, after which a cotton applicator is saturated with 1% silver nitrate solution and applied in a rolling fashion to the affected area. The area is flushed with saline, a bandage contact lens applied, and a 1-week course of topical antibiotics is prescribed. The bandage lens may be removed after 3 to 4 days, after complete epithelialization for the cornea.[1][5]
Symptoms usually resolve within two weeks of treatment with the replacement of irregular epithelium with normal-appearing tissue. Following treatment, most patients experience a total return of vision in the affected eye, although some patients exhibit a mild permanent decrease in visual acuity.[1][2][5] In cases where AWE does not cause symptoms, simply removing the causative agent may be sufficient for resolution.
Silver nitrate likely works via its cytological effects, causing apoptosis or chemical alteration of the abnormal stem cells that are responsible for the pathology.[1] One study used liquid nitrogen cryotherapy in place of silver nitrate with similar results.[5]
Corneal epithelial debridement allows for a more complete treatment of the epitheliopathy and a more rapid resolution of symptoms.[1] Debridement alone is temporarily adequate but is almost universally followed by recurrence and the need for repeat treatment after several months.[1][2] One theory suggests that abnormal limbal stem cells may be the source of the pathology and must be altered to obtain complete resolution. Silver nitrate and cryotherapy appear to fill this role.[2][7]
AWE has rarely responded to artificial tears and topical steroids, although most patients showed no improvement, and steroid use was discontinued in all cases due to a rise in intraocular pressure. Hypertonic saline solution, antibiotics, and therapeutic contact lenses have been found to have little or no benefit in treating AWE.[2][1]
Because of the similarities between AWE and partial limbal stem cell deficiency, there is the possibility that additional medical therapies effective in partial LCSD may also be applied to the treatment of AWE. These include topical retinoids, topical cyclosporine, autologous topical serum drops, and interferon-alpha-2b.[6][7][8][12][13] These treatments have yet to be proven and will need clinical trials for validation.
Differential Diagnosis
Several ocular diseases can present similarly to advancing wavelike epitheliopathy but can be identified or ruled out based on physical exam findings and response to treatment. These conditions include the following:[1][2][5]
- Corneal intraepithelial neoplasia
- Corneal epithelial dysplasia
- Squamous cell carcinoma
- Carcinoma in situ
- Hereditary benign intraepithelial dyskeratosis
- Corneal pannus
- Corneal epithelial keratinization
- Contact lens-induced keratopathy
- Superior limbic keratoconjunctivitis
- Prominent epithelial basement membrane dystrophy
- Whorled microcystic dystrophy
- Underlying dermatologic or inflammatory disorders
Prognosis
The majority of cases respond well to silver nitrate resulting in a return of baseline vision, although rarely, patients may experience mild permanent vision loss. In some cases, small patches of irregular epithelium remain after treatment; however, remnants are almost exclusively at the corneal periphery, leaving the visual axis clear. Recurrence is rare and usually less severe, tending to occur outside the visual axis without requiring repeated treatment.[1]
Complications
Complications are rare but include corneal abrasion and incomplete resolution requiring further treatment.[1]
Deterrence and Patient Education
Patients diagnosed with advancing wavelike epitheliopathy should seek to identify possible triggers and avoid those stimuli in the future. Patients who regularly wear contact lenses should be advised to maintain proper care of their lens and avoid extended wear. If a multipurpose contact lens solution is a possible cause, substitution with a hydrogen peroxide solution may be indicated.
Pearls and Other Issues
- AWE is a chronic or recurrent disorder characterized by progressive visual loss and often ocular irritation or discomfort.
- AWE usually occurs after the age of 40 and is more common in patients with a history of eye trauma or surgery, topical ocular medications, atopic dermatitis, and acne rosacea.
- AWE is diagnosed clinically with slit lamp and confocal microscopy. Pathology and confocal microscopy are also characteristic but not necessary for diagnosis.
- AWE is treated with 1% silver nitrate applied topically and usually resolves within 2 to 3 weeks of a single treatment.
Enhancing Healthcare Team Outcomes
Patients may approach primary care providers when initially experiencing the symptoms associated with AWE. Artificial tears may be beneficial for symptomatic relief of ocular irritation or discomfort. Patients who experience a confirmed decrease in visual acuity, use topical ocular medications, or have symptoms that do not resolve with conservative treatment should be referred to an ophthalmologist. Ophthalmology nurses and pharmacists aid in patient education and care. [Level 5]