Introduction
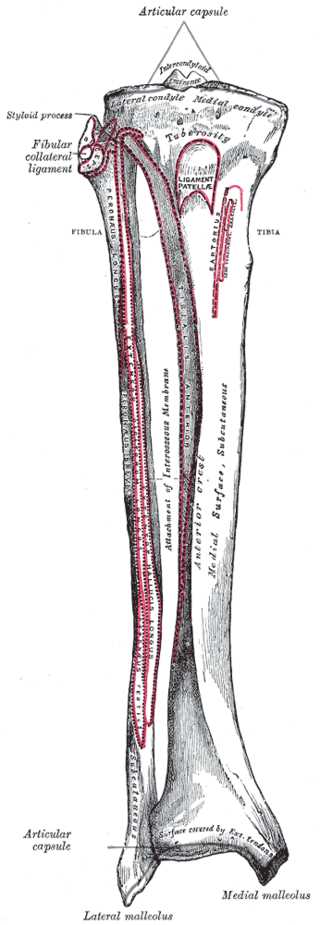
The tibia is one of two bones that comprise the leg.[1] As the weight-bearing bone, it is significantly larger and stronger than its counterpart, the fibula. The tibia forms the knee joint proximally with the femur and forms the ankle joint distally with the fibula and talus. The tibia runs medial to the fibula from just below the knee joint to the ankle joint and is connected to the fibula by the interosseous membrane.[2]
The proximal portion of the tibia consists of a medial and lateral condyle, which combine to form the inferior portion of the knee joint. Between the two condyles lies the intercondylar area, which is where the anterior collateral ligament, posterior collateral ligament, and menisci all have attachments.
The shaft of the tibia is triangular in cross-section with three borders and three surfaces. [3] The three borders as the anterior, medial, and interosseous and the three surfaces are the lateral, medial (anterior), and posterior. The anterior border divides the medial and lateral surface, the medial border divides the medial and posterior surface, and the interosseous border divides the lateral and posterior surface. While the medial surface is mostly subcutaneous, the lateral surface abuts the anterior compartment of the leg, and the posterior surface abuts the posterior compartment.
The distal portion of the tibia is shaped like a box with a distal medial protuberance that makes up the medial malleolus.[4] There are five surfaces that make up the distal tibia.
- The inferior surface provides a smooth articulation with the talus.
- The anterior surface is covered by extensor tendons and provides an area for ankle joint capsule attachment.
- The posterior surface has a groove for the tibialis posterior muscle.
- The lateral surface has a fibular notch which serves as an attachment for the interosseous membrane.
- The medial surface is a large bony prominence that makes up the medial malleolus.