[1]
Hong S, Usami K, Hirokawa D, Ogiwara H. Pediatric meningiomas: a report of 5 cases and review of literature. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2019 Nov:35(11):2219-2225. doi: 10.1007/s00381-019-04142-y. Epub 2019 Apr 18
[PubMed PMID: 31001646]
Level 3 (low-level) evidence
[2]
Shaikh M, Khera P, Yadav T, Garg P. Dural Ectasia of the Optic Nerve: A Rare Presentation in Neurofibromatosis Type I. Journal of neurosciences in rural practice. 2019 Apr-Jun:10(2):349-351. doi: 10.4103/jnrp.jnrp_232_18. Epub
[PubMed PMID: 31001034]
[3]
Kheir V, Faouzi M, Borruat FX. Visual Outcomes of Fractionated Radiotherapy in Optic Nerve Sheath Meningioma: A Retrospective Study. Klinische Monatsblatter fur Augenheilkunde. 2019 Apr:236(4):526-529. doi: 10.1055/a-0828-7335. Epub 2019 Feb 27
[PubMed PMID: 30812038]
Level 2 (mid-level) evidence
[4]
Pandit R,Paris L,Rudich DS,Lesser RL,Kupersmith MJ,Miller NR, Long-term efficacy of fractionated conformal radiotherapy for the management of primary optic nerve sheath meningioma. The British journal of ophthalmology. 2018 Dec 20;
[PubMed PMID: 30573496]
[5]
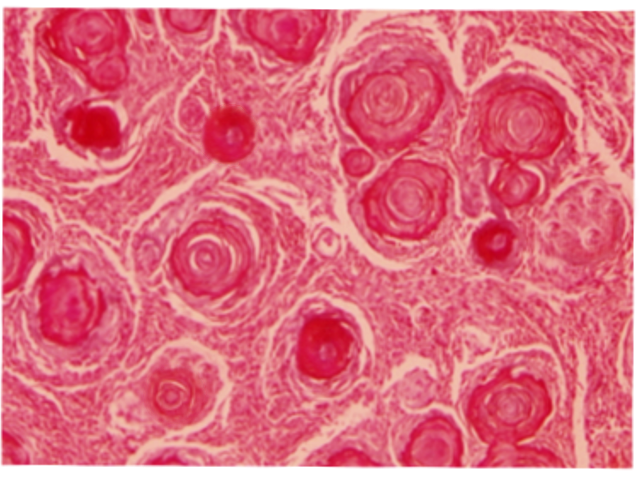
Furdová A, Babál P, Kobzová D. Optic nerve orbital meningioma. Ceska a slovenska oftalmologie : casopis Ceske oftalmologicke spolecnosti a Slovenske oftalmologicke spolecnosti. 2018 Spring:74(1):23-30
[PubMed PMID: 30541293]
[6]
Parker RT, Ovens CA, Fraser CL, Samarawickrama C. Optic nerve sheath meningiomas: prevalence, impact, and management strategies. Eye and brain. 2018:10():85-99. doi: 10.2147/EB.S144345. Epub 2018 Oct 24
[PubMed PMID: 30498385]
[7]
Rassi MS, Prasad S, Can A, Pravdenkova S, Almefty R, Al-Mefty O. Prognostic factors in the surgical treatment of intracanalicular primary optic nerve sheath meningiomas. Journal of neurosurgery. 2018 Sep 21:131(2):481-488. doi: 10.3171/2018.4.JNS173080. Epub
[PubMed PMID: 30239315]
[8]
Narayan D, Rajak S, Patel S, Selva D. Cystic change in primary paediatric optic nerve sheath meningioma. Orbit (Amsterdam, Netherlands). 2016 Aug:35(4):236-8. doi: 10.1080/01676830.2016.1176212. Epub 2016 Jun 16
[PubMed PMID: 27310300]
[9]
Levin LA, Jakobiec FA. Optic nerve tumors of childhood: a decision-analytical approach to their diagnosis. International ophthalmology clinics. 1992 Winter:32(1):223-40
[PubMed PMID: 1537660]
[10]
Lekovic GP, Schwartz MS, Hanna G, Go J. Intra-Orbital Meningioma Causing Loss of Vision in Neurofibromatosis Type 2: Case Series and Management Considerations. Frontiers in surgery. 2018:5():60. doi: 10.3389/fsurg.2018.00060. Epub 2018 Oct 9
[PubMed PMID: 30356733]
Level 2 (mid-level) evidence
[11]
Jacobi DM. Optic nerve sheath meningioma. Clinical & experimental optometry. 2019 Mar:102(2):188-190. doi: 10.1111/cxo.12819. Epub 2018 Jul 28
[PubMed PMID: 30054955]
[12]
Frisèn L,Royt WF,Tengroth BM, Optociliary veins, disc pallor and visual loss. A triad of signs indicating spheno-orbital meningioma. Acta ophthalmologica. 1973
[PubMed PMID: 4801582]
[13]
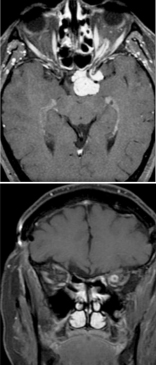
Saeed P, Rootman J, Nugent RA, White VA, Mackenzie IR, Koornneef L. Optic nerve sheath meningiomas. Ophthalmology. 2003 Oct:110(10):2019-30
[PubMed PMID: 14522782]
[14]
Sibony P, Strachovsky M, Honkanen R, Kupersmith MJ. Optical coherence tomography shape analysis of the peripapillary retinal pigment epithelium layer in presumed optic nerve sheath meningiomas. Journal of neuro-ophthalmology : the official journal of the North American Neuro-Ophthalmology Society. 2014 Jun:34(2):130-6. doi: 10.1097/WNO.0000000000000107. Epub
[PubMed PMID: 24625774]
[15]
Loo JL, Tian J, Miller NR, Subramanian PS. Use of optical coherence tomography in predicting post-treatment visual outcome in anterior visual pathway meningiomas. The British journal of ophthalmology. 2013 Nov:97(11):1455-8. doi: 10.1136/bjophthalmol-2013-303449. Epub 2013 Aug 21
[PubMed PMID: 23966371]
[16]
Hénaux PL, Bretonnier M, Le Reste PJ, Morandi X. Modern Management of Meningiomas Compressing the Optic Nerve: A Systematic Review. World neurosurgery. 2018 Oct:118():e677-e686. doi: 10.1016/j.wneu.2018.07.020. Epub 2018 Aug 3
[PubMed PMID: 30010062]
Level 1 (high-level) evidence
[17]
Maza G, Subramaniam S, Yanez-Siller JC, Otto BA, Prevedello DM, Carrau RL. The Role of Endonasal Endoscopic Optic Nerve Decompression as the Initial Management of Primary Optic Nerve Sheath Meningiomas. Journal of neurological surgery. Part B, Skull base. 2019 Dec:80(6):568-576. doi: 10.1055/s-0039-1677689. Epub 2019 Jan 10
[PubMed PMID: 31750042]
[18]
Hunt PJ, DeMonte F, Tang RA, Su SY, Raza SM. Surgical Resection of an Optic Nerve Sheath Meningioma: Relevance of Endoscopic Endonasal Approaches to the Optic Canal. Journal of neurological surgery reports. 2017 Apr:78(2):e81-e85. doi: 10.1055/s-0037-1600897. Epub
[PubMed PMID: 28413768]
[19]
Sasano H, Shikishima K, Aoki M, Sakai T, Tsutsumi Y, Nakano T. Efficacy of intensity-modulated radiation therapy for optic nerve sheath meningioma. Graefe's archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 2019 Oct:257(10):2297-2306. doi: 10.1007/s00417-019-04424-w. Epub 2019 Aug 3
[PubMed PMID: 31377848]
[20]
Liu JK, Forman S, Hershewe GL, Moorthy CR, Benzil DL. Optic nerve sheath meningiomas: visual improvement after stereotactic radiotherapy. Neurosurgery. 2002 May:50(5):950-5; discussion 955-7
[PubMed PMID: 11950397]
[21]
Ratnayake G, Oh T, Mehta R, Hardy T, Woodford K, Haward R, Ruben JD, Dally MJ. Long-term treatment outcomes of patients with primary optic nerve sheath meningioma treated with stereotactic radiotherapy. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia. 2019 Oct:68():162-167. doi: 10.1016/j.jocn.2019.07.005. Epub 2019 Aug 7
[PubMed PMID: 31401001]
[22]
Micieli JA, Streutker CJ, McIntyre K. Isolated Optic Perineuritis as the Presenting Sign of Sarcoidosis. Journal of neuro-ophthalmology : the official journal of the North American Neuro-Ophthalmology Society. 2020 Jun:40(2):255-257. doi: 10.1097/WNO.0000000000000822. Epub
[PubMed PMID: 31490345]