Continuing Education Activity
Herpes zoster, also known as shingles, is a viral syndrome caused by reactivation of the varicella-zoster virus. After an episode of varicella (chicken-pox), the varicella-zoster virus remains dormant in the nervous system. Herpes zoster typically occurs in adults or elderly. This activity outlines the presentation, evaluation, and management of shingles and highlights the role of the interprofessional team in managing patients with this condition.
Objectives:
- Identify the etiology of shingles.
- Describe the presentation of a patient with shingles.
- List treatment and management options available for shingles.
- Explain interprofessional team strategies to prevent shingles and improve the care of affected individuals.
Introduction
Herpes zoster is commonly known as shingles. It is a viral disease caused by reactivation of varicella-zoster virus which remains dormant in the sensory ganglia of the cranial nerve or the dorsal root ganglia after a previous varicella infection. Varicella is commonly known as chickenpox; it occurs in children while herpes zoster occurs in adults or the elderly.[1][2][3]
It is believed that zoster occurs due to the failure of the immune defense system to control the latent replication of the virus. The incidence of herpes zoster is strongly correlated to the immune status. Individuals who maintain a high level of immunity rarely develop shingles. The infection is not benign and can present in many ways. Even after herpes zoster resolves, many patients continue to suffer from moderate to severe pain known as postherpetic neuralgia.
Etiology
Upon reactivation, the virus replicates in neuronal cell bodies, and virions shed from the cells which are carried down the nerve to the area of skin innervated by that ganglion. In the skin, the virus causes local inflammation and blistering. The pain caused by zoster is due to inflammation of affected nerves with the virus.[4][5][6]
Triggers for herpes zoster include
- Emotional stress
- Use of medications (immunosuppressants)
- Acute or chronic illness
- Exposure to the virus
- Presence of a malignancy
Epidemiology
The incidence of herpes zoster ranges from 1.2 to 3.4 per 1000 persons per year among younger healthy individuals while incidence is 3.9 to 11.8 per 1000 persons per year among patients older than 65 years. There is no seasonal variation seen with herpes zoster.
Recurrences are most common in patients who are immunosuppressed.
Pathophysiology
Cutaneous lesions of herpes zoster produce Varicella-zoster virus-specific T-cell proliferation, while the production of interferon alfa leads to the resolution of herpes zoster. In immunocompetent patients, specific antibodies (IgG, IgM, and IgA) appear more rapidly and reach higher titers during reactivation (herpes zoster) than during the primary infection causing long-lasting, enhanced, cell-mediated immunity to the varicella-zoster virus.
The dermatological involvement is centripetal and follows a dermatome. In most cases, it is the lumbar and cervical roots that are involved, whereas motor involvement is rare. The infection is contagious to individuals who have no prior immunity to varicella-zoster, however, the rates of transmission are low. The virus can be transmitted either via direct skin contact or by inhaling infected droplets.
It is important to be aware that herpes infections can also occur at the same time. Herpes simplex, CMV, EBV, and human herpesviruses have all been found in patients with shingles.
History and Physical
Zoster characteristically presents with a prodrome of fever, malaise, and excruciating burning pain followed by the outbreak of vesicles that appear in one to three crops over three to five days. Lesions are distributed unilaterally within a single dermatome.
Clinically, lesions start as closely grouped erythematous papules which, rapidly become vesicles on an erythematous and edematous base and may occur in continuous or interrupted bands in one, two, or more contiguous dermatomes unilaterally. Dermatomes commonly involved are thoracic (53%), cervical (20%), and trigeminal (15%) including ophthalmic and lumbosacral (11%).
The three phases of the infection include:
- Preeruptive stage presents with abnormal skin sensations or pain within the dermatome affected. this phase appears at least 48 hours prior to any obvious lesions. At the same time, the individual may experience headaches, general malaise, and photophobia.
- The acute eruptive phase is marked by the vesicles and the symptoms seen in the pre-eruptive phase. The lesions initially start as macules and quickly transform into painful vesicles. The vesicles often rupture, ulcerate and eventually crust over. Patients are most infectious in this stage until the lesion dry out. Pain is severe during this phase and often unresponsive to traditional pain medications. The phase may last 2-4 weeks but the pain may continue.
- Chronic infection is characterized by recurrent pain that lasts more than 4 weeks. Besides the pain, patients experience paresthesias, shock-like sensations, and dysesthesias. The pain is disabling and may last 12 months or longer.
Shingles oticus is also known as Ramsay Hunt syndrome type II. It is due to the spreading of the virus from the facial nerve to the vestibulocochlear nerve which involves the ear and causes hearing loss and vertigo (rotational dizziness).
Zoster may occur in the mouth if the maxillary or mandibular division of the trigeminal nerve is affected. Clinically, it presents with vesicles or erosions occurring over the mucous membrane of the upper jaw (palate, gums of the upper teeth) or the lower jaw (tongue or gums of the lower teeth). Oral involvement may occur alone or in combination with the lesions on the skin over the cutaneous distribution of the same trigeminal branch.
Due to the close relationship of blood vessels to nerves, the virus can spread to involve the blood vessels compromising the blood supply, and causing ischemic necrosis. Complications such as osteonecrosis, tooth loss, periodontitis, pulp calcification, pulp necrosis, periapical lesions, and tooth developmental anomalies can occur due to it.
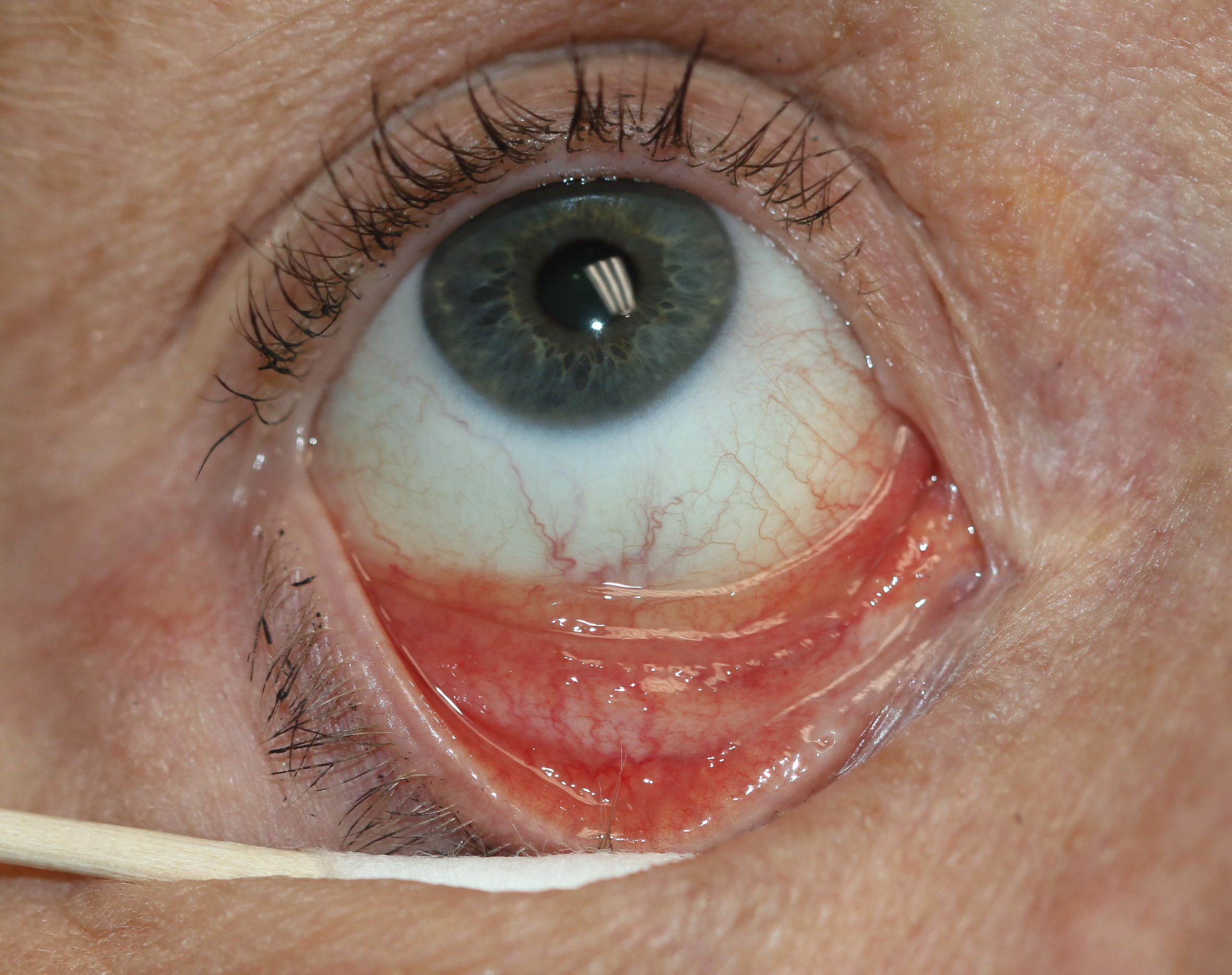
The ophthalmic division of the trigeminal nerve is the most commonly involved branch which causes ophthalmic zoster. The skin of the forehead, upper eyelid, and orbit of the eye may be involved. It is seen in approximately 10% to 25% of cases presenting with features of, keratitis, uveitis, and optic nerve palsies. Complications in the form of chronic ocular inflammation, loss of vision, and debilitating pain can occur.
The involvement of the CNS is not uncommon. since the virus resides in the sensory root ganglia, it can affect any part of the brain causing cranial nerve palsies, muscular weakness, diaphragmatic paralysis, neurogenic bladder, Guillain Barre syndrome, and myelitis. In severe cases, patients may develop encephalitis.
Complications of herpes zoster include secondary bacterial infection, post-herpetic neuralgia, scarring, nerve palsy, and encephalitis in the case with disseminated zoster.
- Disseminated zoster is defined as more than twenty skin lesions developing outside the primarily affected area or dermatomes directly adjacent to it. Besides the skin, other organs may also be affected, causing hepatitis or encephalitis making this condition potentially lethal.
- Post-herpetic neuralgia is the persistence of pain after a month of onset of herpes zoster. It is the commonest side effect seen in elderly patients with involvement of the ophthalmic division of trigeminal nerve.
- Complications like cranial neuropathies, polyneuritis, myelitis, aseptic meningitis, or partial facial paralysis occur due to the involvement of the nervous system.
During pregnancy, varicella may lead to infection in the fetus and complications in the newborn, but chronic infection or reactivation, in other words, herpes zoster, is not associated with fetal infection.
Zoster sine herpete is an entity with a pain in the involved dermatome without any skin lesions.
Evaluation
Herpes zoster is clinically diagnosed with burning pain, characteristic morphology, and typical distribution. Herpes simplex virus can occasionally produce a rash in a pattern called as zosteriform herpes simplex.[7][8][9]
Tests for varicella-zoster virus include the following:
- The Tzanck smear of vesicular fluid shows multinucleated giant cells. It has lower sensitivity and specificity than direct fluorescent antibody (DFA) or Polymerase chain reaction (PCR).
- Varicella-zoster virus-specific IgM antibody in blood is detected during the active infection of chickenpox or shingles but not when the virus is dormant
- Direct fluorescent antibody testing of vesicular fluid or corneal fluid can be done when there is eye involvement.
- PCR testing of vesicular fluid, a corneal lesion, or blood in a case with eye involvement or disseminated infection.
Molecular biology tests based on in vitro nucleic acid amplification (PCR tests) are currently considered the most reliable. Nested PCR test has high sensitivity, but is susceptible to contamination leading to false-positive results. The latest real-time PCR tests are rapid, easy to perform, as sensitive as nested PCR, have a lower risk of contamination, and also have more sensitivity than viral cultures.
Differential Diagnosis
Cutaneous lesions of herpes zoster need to be differentiated from herpes simplex, dermatitis herpetiformis, impetigo, contact dermatitis, candidiasis, drug reactions, and insect bites. Preceding pain without the development of skin lesions in herpes zoster is different from cholecystitis and biliary colic, renal colic, trigeminal neuralgia, or any dental infection.
Herpes zoster tends to involve only one side of the oral cavity, which distinguishes it from other oral blistering conditions. In the mouth, it presents initially as vesicles that break down quickly to leave ulcers that heal within 10 to 14 days. The prodromal pain before the rash may be confused with a toothache which leads to unnecessary dental treatment.
Treatment / Management
Antiviral therapy hastens the resolution of lesions, decreases acute pain and helps to prevent post-herpetic neuralgia especially in elderly patients. Acyclovir 800 mg, five times daily for five days, valacyclovir 1 gm three times daily for five days, and famciclovir 500 mg three times daily for seven days are the antiviral drugs used to treat herpes zoster. Topical antibiotic creams like mupirocin or soframycin help to prevent secondary bacterial infection. Analgesics help to relieve the pain. Occasionally, severe pain may require an opioid medication. Topical lidocaine and nerve blocks may also reduce pain.[7][10][11]
Post-herpetic neuralgia commonly occurs in elderly patients, and once the lesions have crusted, they can use topical capsaicin and Emla cream.
Enhancing Healthcare Team Outcomes
Shingles is a common infectious disorder in the elderly with significant morbidity. The condition has no cure but can be prevented in most patients via vaccination. When there is eye involvement, patients must be referred ASAP to an ophthalmologist. Healthcare workers including the primary care provider, nurse practitioner, internist and pharmacist should educate the patient on the benefits of the vaccine. [12][13]