Continuing Education Activity
Temporal bone fractures are uncommon but may involve many important structures and cause various diagnostic and therapeutic issues. A large amount of force is required to fracture the temporal bone, so patients often present with other concomitant injuries. Unlike fractures in other head and neck regions, the management of temporal bone fractures is focused on addressing functional deficits rather than reduction and fixation. Since the temporal bone is non-weight bearing, cosmetic sequelae are rare secondary to this trauma. However, deficits from facial nerve injury can be devastating to patients from not only a functional perspective but also a cosmetic standpoint. This activity reviews the etiology, presentation, evaluation, and management of facial nerve injuries associated with temporal bone fractures and reviews the role of the interprofessional team in evaluating, diagnosing, and managing patients with these injuries.
Objectives:
- Discuss the pathophysiology of temporal bone trauma and how it can affect the facial nerve and other important structures.
- Outline the evaluation process, including history and physical examination procedures, needed to effectively evaluate facial nerve damage secondary to temporal bone trauma.
- Review the treatment options available in temporal bone fracture-associated facial nerve injury cases.
- Explain the importance of interprofessional team strategies for improving care coordination and communication to aid in prompt diagnosis of temporal bone trauma with facial paralysis and to improve patient outcomes in the short and long term.
Introduction
Temporal bone fractures are fortunately comparatively uncommon, occurring in roughly half of blunt head injuries; when they do occur, however, they have the potential to involve many vital structures that may result in acute and long-term disability. A large amount of force is required to fracture the temporal bone, particularly the petrous portion. For this reason, patients tend to present with concomitant trauma, such as intracranial bleeding, cervical spine fractures, and other musculoskeletal injuries.
Unlike other fractures in the head and neck region, the management of temporal bone fractures focuses on addressing functional deficits rather than reduction and fixation; the temporal bone is non-weight bearing, and cosmetic sequelae are rare secondary to fracture. However, functional deficits from the facial nerve and cochleovestibular injuries can be devastating to patients and may cause considerable decrements in quality of life.
Etiology
In the adult population, most temporal bone fractures result from motor vehicle accidents (55%), with falls being the second most common cause (25%), industrial accidents the third (16%), and assaults fourth (4%).[1] In pediatric patients, 30% result from motor vehicle accidents compared to 60% from falls.[2]
Most temporal bone fractures are caused by laterally-directed blows to the skull, but anteroposterior blows can also cause temporal bone fractures and are liable to produce fractures that propagate transversely across the petrous pyramid and involve the otic capsule - the region of dense bone that contains the cochlea, vestibule, and semicircular canals.
Epidemiology
Temporal bone fractures have been reported across all age groups; however, 70% occur within the second through fourth decades of life with a 3 to 1 male to female predominance.[3] Facial paralysis occurs in 7 to 12% of temporal bone fractures, 83% resulting from a unilateral fracture, 5% associated with bilateral fractures, and 12% in the absence of a radiologically-apparent fracture.[1][3][4]
Bilateral fractures occur in roughly 17% of patients, and the distribution between left and right sides in cases of unilateral fracture is approximately equal.[3] Other complications that occur in the setting of temporal bone fractures include conductive hearing loss (66% of patients), bloody otorrhea (61%), hemotympanum (56%), tympanic membrane perforation (26%), cerebrospinal fluid (CSF) leak (9%), and sensorineural hearing loss (5%).[1] Overall, temporal bone fractures occur in 30-70% of blunt head injuries.[5][6]
Pathophysiology
The temporal bone is divided into four portions: the squamous, which makes up part of the lateral portion of the cranial vault; the tympanic, which contains the middle ear cleft; the mastoid, which contains the air cells contiguous with the middle ear via the antrum, and the petrous pyramid, which contains the otic capsule - the densest bone in the human body. Temporal bone fractures typically occur in the setting of high-energy blunt head trauma; the force required to fracture the temporal bone is approximately 1,875 lbs.[7] For this reason, concomitant injuries, such as concussion and maxillofacial and cervical spine fractures, are common.
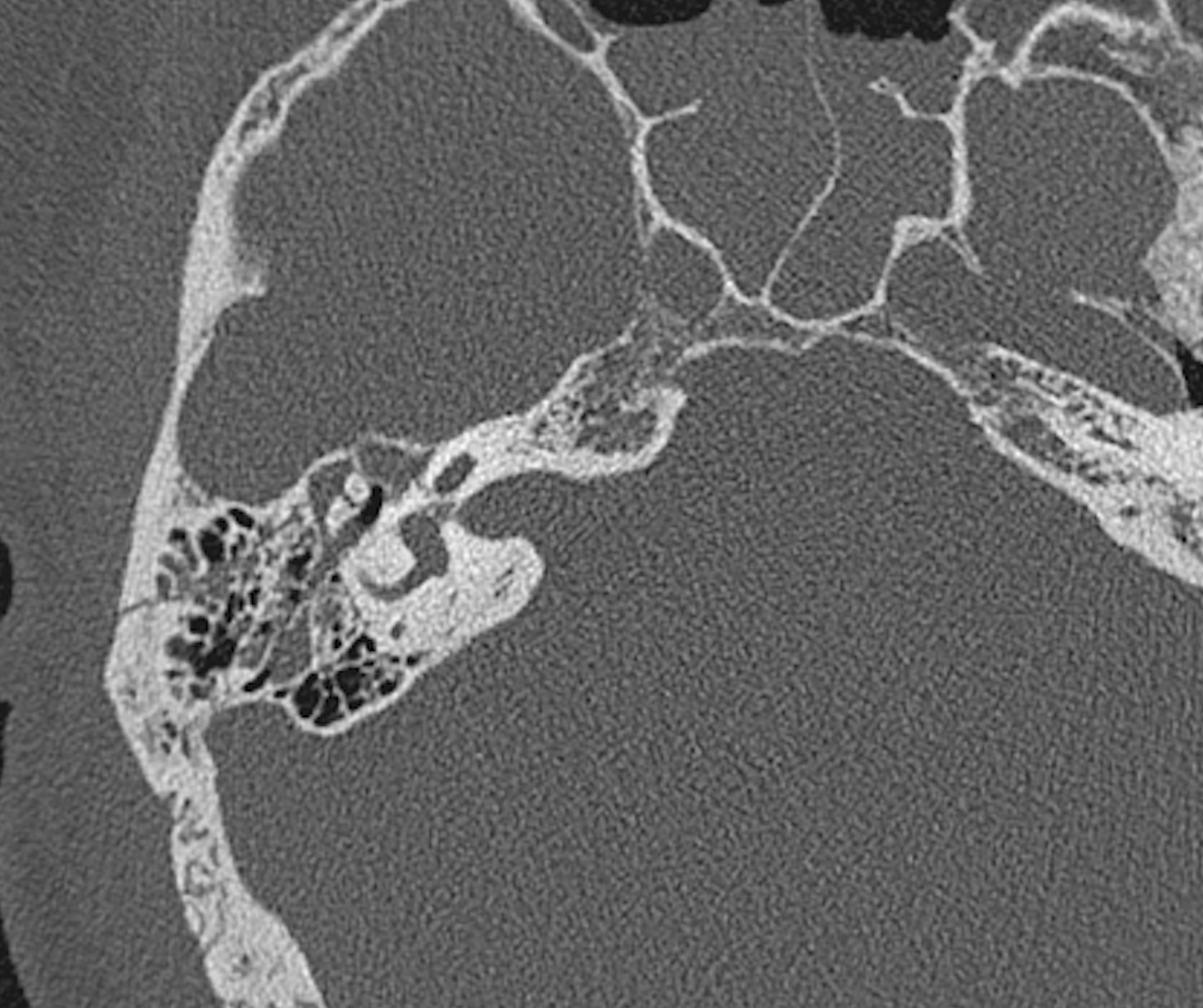
Historically, temporal bone fractures have been divided into longitudinal and transverse patterns based on the vector of fracture propagation relative to the petrous pyramid.[2] Longitudinal fractures account for 80-90% of cases, with transverse fractures making up 10-20%.[2][8] Over time, it became apparent that most fractures could not be categorized easily using this overly simplistic scheme, and functional deficits were not accurately predicted, so a new classification system was developed based on whether the fracture disrupts or spares the otic capsule.[9] Fracture patterns are determined by both the vector of the traumatic force and the positions of various weak points in the skull base, such as the jugular foramen, the stylomastoid foramen, the foramen magnum, and the foramen lacerum.[10]
Otic capsule sparing fractures travel from the squamosal portion of the temporal bone and the posterosuperior wall of the external auditory canal through the mastoid air cells and middle ear into the tegmen mastoideum and tegmen tympani (roof of the mastoid air cells and middle ear, respectively). These fractures typically result from a blow to the temporoparietal region and account for 95% of temporal bone fractures.[3] The rate of facial paralysis in otic capsule sparing fractures is comparatively low, at ~6%.[3]
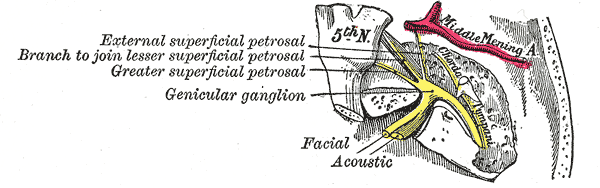
Otic capsule-disrupting fractures pass through the otic capsule and proceed from the foramen magnum to the petrous pyramid and otic capsule. These fractures do not typically affect the ossicular chain or the external auditory canal but almost always result in sensorineural hearing loss and are two to eight times more likely to result in CSF otorrhea than otic capsule sparing fractures.[3][11][12][13] They are also highly likely to result in facial nerve injury, with 48% of patients experiencing facial weakness after one of these fractures.[3] The facial nerve courses through the Fallopian canal within the temporal bone, which itself is divided into four segments. From proximal to distal, they are the meatal segment (8-10 mm in length), the labyrinthine segment (2-4 mm in length and 1.6 mm in diameter), the tympanic segment (9 to 11 mm and 1.4 mm in diameter), and the mastoid segment (12-4 mm and 1.8 mm in diameter).[14][15]
Most facial nerve injuries due to temporal bone fractures occur in the labyrinthine portion, specifically in the geniculate ganglion.[16][17] The most common type of injury is edema with intraneural hematoma (86%); partial or complete transection, fortunately, occurs in only 14% of cases.[17]
History and Physical
In many cases, it can be difficult to perform a comprehensive physical examination because of the patient's mental status after trauma. Many patients are admitted to the intensive care unit sedated and intubated. While skeletal deformities, lacerations, ecchymosis, hemotympana, and otorrhea can be appreciated without patient cooperation, facial nerve function and hearing assessment are difficult to perform with an unconscious patient. Ideally, some measure of facial function evaluation should be obtained prior to initiation of sedation, but it is often difficult to perform a complete and systematic examination in the acute setting.
While only about one in ten patients with a temporal bone fracture will suffer facial paralysis, it is important to attempt to determine whether the facial function was normal immediately after the injury or not. If there is complete paralysis immediately after the blow to the head, it is possible that the facial nerve was transected. If paralysis evolves slowly over the course of hours, days, or weeks after the injury, the paralysis is likely caused by edema of the facial nerve and may be managed medically. When the time course of the paralysis onset is unknown, it should be treated as a case of immediate onset. Facial paralysis can be classified in myriad different ways; however, the most common system is that of House and Brackmann, summarized below:
- Grade I: normal function
- Grade II: mild dysfunction, symmetric at rest, slight asymmetry with movement but complete eye closure with gentle effort
- Grade III: moderate dysfunction, symmetric at rest, moderate asymmetry with movement but complete eye closure with full effort
- Grade IV: moderate dysfunction, symmetric at rest, moderate asymmetry with movement, and incomplete eye closure with full effort
- Grade V: severe dysfunction, grossly asymmetric at rest, marked asymmetry with movement, and incomplete eye closure with full effort
- Grade VI: severe dysfunction, grossly asymmetric at rest, no movement at all[18]
In patients with facial paralysis after an ipsilateral temporal bone fracture, it is critical to determine two things by history and physical examination: whether the paralysis was immediate or delayed and whether it was complete (House-Brackmann VI) or incomplete (House-Brackmann II-V). With immediate, complete paralysis ipsilateral to the temporal bone fracture, the index of suspicion for nerve transection should be high; fortunately, this presentation is uncommon. When the paralysis is delayed and/or incomplete, it is unlikely that the nerve has been transected, and the patient can usually be managed conservatively. Patients with complete and immediate paralysis generally require additional evaluation (see below), and patients whose paralyzes progress to House-Brackmann grade VI palsy may also be candidates for further evaluation. When performing a physical examination to determine the House-Brackmann grade of the facial paralysis, it is essential to realize that gravity-driven complete eye closure may be preserved for several hours or even a few days after injury.
For this reason, systematically examining the rest of the face (raise eyebrows, wrinkle nose, smile, pucker lips, depress lower lip) is critical to determining the severity of the paralysis. If none of the other mimetic muscles is moving on the side of the injury, but eye closure is complete, particularly if the closure is slow and asynchronous with the other side, the patient is still graded House-Brackmann VI, and eye closure should be expected to worsen in the near future. While most patients will demonstrate some degree of recovery of facial function over time, it is easy to cause a corneal abrasion or an exposure keratopathy in the setting of paralytic lagophthalmos while facial movement slowly recovers; for this reason, it is critical to assess the cornea frequently until the ability to close the eye returns. A patient with an intact Bell's phenomenon (the globe rolls superiorly as the eyelid closes) is less likely to suffer corneal injuries than one without; patients tend to lose this protective reflex with advanced age.
Examination of the external auditory canal should focus on identifying step-offs or lacerations that could indicate a fracture, and the presence or absence of otorrhea should be noted. If otorrhea is present, the tympanic membrane is likely perforated, and consideration should be given to testing the fluid to determine whether CSF is present. Packing the external auditory canal is unnecessary unless it is required to control significant hemorrhage. If profuse hemorrhage cannot be controlled with packing, the patient may need to be taken to the operating room for carotid artery ligation or angiography for balloon occlusion. Examination of the tympanic membrane should determine if it is intact or perforated. Bloody otorrhea and hemotympanum are the two most common signs of temporal bone fracture. Generally, hemotympanum is self-resolving within 4 to 6 weeks. Traumatic tympanic membrane perforations may heal spontaneously, depending on their overall size.
Hearing is initially assessed at the bedside via tuning fork examination with a 512 Hz tuning fork. Both Weber and Rinne tests are helpful to determine if a conductive or sensorineural hearing loss is present. Preoperative audiometry is essential in the presence of facial paralysis or CSF fistula where operative management is indicated.
The vestibular system is contained within the temporal bone and should also be routinely evaluated in the presence of a temporal bone injury. Neurologic injuries such as concussions, contusions, and other injuries to the brainstem and cerebellar pathways may coexist with otic capsule disrupting fractures. A bedside vestibular evaluation should be performed in addition to a neurological assessment. The presence of a cervical spine injury must be excluded before any vestibular evaluation can be performed, however. Vestibular evaluation should include examination for spontaneous and gaze-evoked nystagmus, head thrust nystagmus for refixation saccades, and assessment of post-head-shake nystagmus. Gait abnormalities should be evaluated, and a Dix-Hallpike test should be performed to look for benign paroxysmal positional vertigo (BPPV). The most common injuries to the vestibular system are BPPV and vestibular hypofunction.
Lastly, palpation of the cranium to assess any deformities or flail segments is important. Most temporal bone fractures are not displaced and do not require any reduction or fixation.
Evaluation
High-resolution computed tomography (CT) is the gold standard for diagnosing and classifying temporal bone fractures. In most cases of injury sufficiently severe to produce a temporal bone fracture, a CT scan will have been ordered as part of the initial trauma evaluation. If not, CT scans of the temporal bone without contrast should be ordered in the presence of facial paralysis, cerebrospinal fluid fistula, disruption of the superior wall of the external auditory canal or scutum with potential trapping of epithelium, suspected vascular injury, or when surgical intervention is anticipated.[19] Hearing loss without other complications does not necessarily warrant CT scanning. CT angiography is superior to non-contrast-enhanced CT scanning if a vascular injury is suspected.[20][21] The CT scan will determine whether the fracture is otic capsule sparing or otic capsule disrupting and indicate whether the Fallopian canal of the facial nerve has been involved. If the canal is fractured or there is a bony fragment impinging on the canal, these may be considered indications for facial nerve decompression.
For patients with complete paralysis (House-Brackmann VI) ipsilateral to the temporal bone fracture, electrodiagnostic testing of the facial nerve may be helpful to determine prognosis and candidacy for surgical facial nerve decompression. Electroneuronography (ENoG) is the most commonly employed testing modality. It involves stimulating the facial nerve transcutaneously where it exits the skull base at the stylomastoid foramen and recording the amplitude of the compound muscle action potentials in the face via surface electrodes placed over the orbicularis oculi and orbicularis oris muscles. If >90% of the action potential amplitude is lost on the injured side, the patient is considered a candidate for facial nerve decompression.[16]
Because it requires an uninjured side to serve as a control, ENoG testing can only be performed effectively in cases of unilateral facial paralysis. Even though some cases of facial paralysis occur immediately after injury to the temporal bone, ENoG testing should not be performed three days after the fracture to permit sufficient time for Wallerian degeneration. Wallerian degeneration is the process by which axons and myelin distal to the site of injury degenerate to allow for regrowth of the axon and its supporting Schwann cells. The process takes at least three days in the case of transection injury but can take weeks or months to complete in the case of crush injuries; the protracted course of Wallerian degeneration in crush injuries explains why some patients do not reach House-Brackmann grade VI paralysis until several weeks after suffering a temporal bone fracture. If ENoG is performed before Wallerian degeneration is complete, the results will underestimate the severity of axonal injury. Patients with slowly evolving facial paralysis should be followed closely until they reach a functional nadir. If that nadir occurs at House-Brackmann grade VI, ENoG testing should be performed.[16]
While it is generally accepted that in the case of Bell's palsy, there is no benefit to surgical facial nerve decompression if it is performed after 14 days, that does not appear to be the case in temporal bone fractures; temporal bone fracture patients may benefit from facial nerve decompression even if it is performed two months post-injury.[16][22] Patients with facial paralysis from temporal bone trauma should be followed with weekly serial ENoGs until clinical improvement is apparent; two months have passed since the injury. After that point, decompression is less likely to improve outcomes, or the ENoG indicates candidacy for facial nerve decompression.[16] Some authors suggest supplementing the ENoG with voluntary needle electromyography (EMG) to confirm the denervation of the facial muscles with the presence of fibrillation, insertional activity, and positive sharp waves.[16][17]
The advantage to an EMG is that in the case of nerve recovery, the ENoG, which relies on synchronous action potentials at the neuromuscular junction, may not demonstrate significant recovery of action potential amplitude, while the EMG may show polyphasic action potentials, which indicate recovery in progress and may forestall an unnecessary surgical procedure.
Audiometry, particularly acoustic reflex testing, can also be helpful in the setting of temporal bone fractures to indicate whether a hearing loss is present, whether it is conductive, sensorineural, or mixed in nature, and whether there is a facial nerve injury. Ossicular injury or chain disruption is uncommon in temporal bone fractures but may occur at the incudostapedial or incudomallear joint and may require reconstruction.[8] If there is clear fluid draining from the ear canal or the nasal cavity, the presence of CSF should be determined by testing the fluid for β-2 transferrin or β-trace protein. If those assays are unavailable, fluid sampling will reveal a glucose content approximately two-thirds that of the blood level. If there is suspicion that the eye on the injured side is not closing properly and is at risk for injury, fluorescein testing will reveal the presence of corneal abrasions or exposure keratopathy.
Treatment / Management
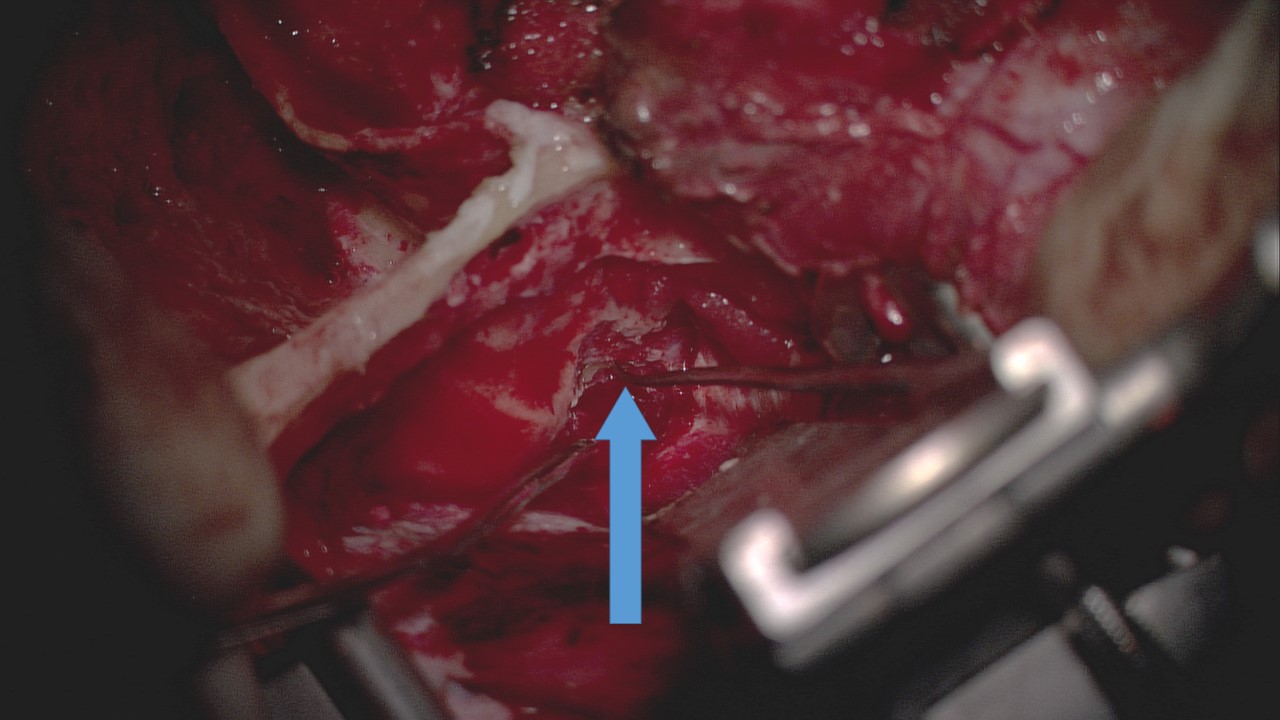
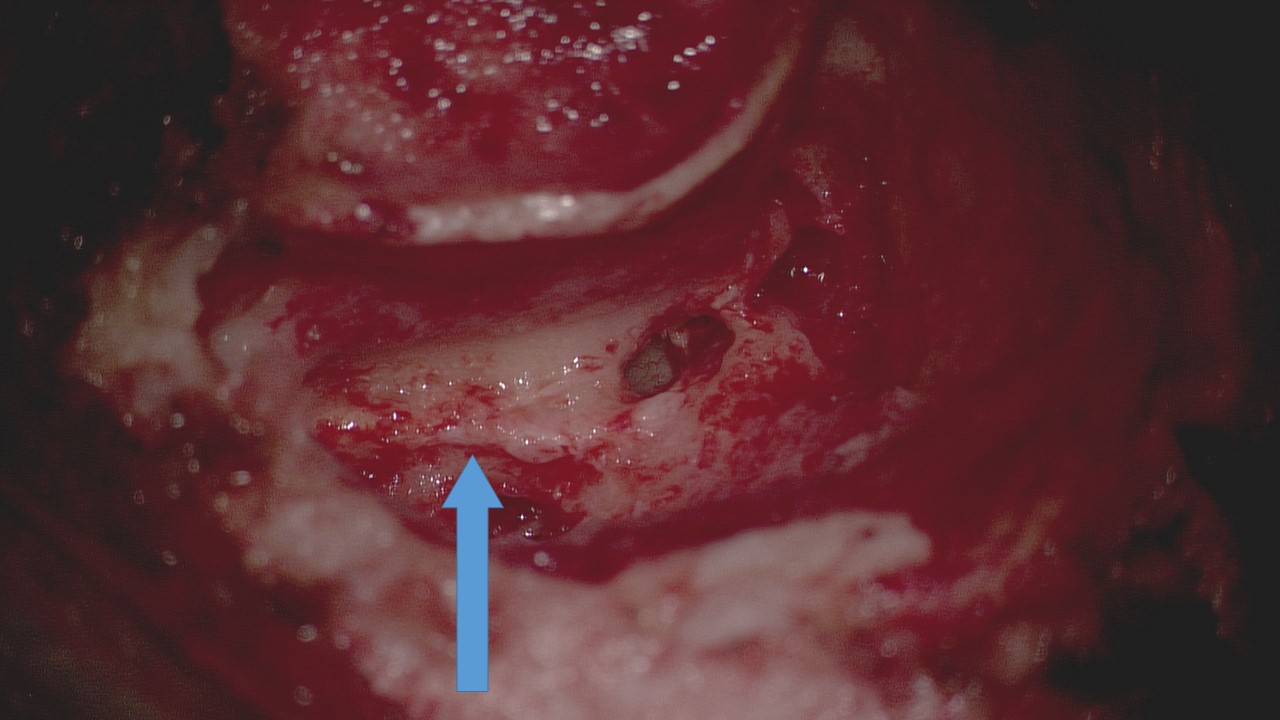
Some authors would contend that immediate and complete facial paralysis after a temporal bone fracture is an absolute indication for surgical facial nerve decompression and, if necessary, repair of the facial nerve, but many would treat this group similar to other patients who present with complete hemifacial paralysis in a delayed manner, waiting three days and then performing an ENoG.[1][10][16] Regardless, once the ENoG identifies >90% degeneration of action potential amplitude on the injured side, the patient may be offered facial nerve decompression. If the patient has intact hearing, middle fossa craniotomy and transmastoid approaches can be used to decompress the facial nerve.[23]
The middle fossa craniotomy provides access to the internal auditory canal and geniculate ganglion, while a transmastoid approach exposes the nerve from the geniculate ganglion to the stylomastoid foramen. If the fracture and site of compression are lateral to the geniculate ganglion, the transmastoid approach can be used alone. For patients with complete anacusis due to otic capsule disrupting fractures, a translabyrinthine approach via a mastoidectomy may be employed because it provides exposure of the entire facial nerve.[17]
If a gap in the facial nerve is encountered and it cannot be reconstructed via primary neurorrhaphy, a cable graft from either the sural nerve or the greater auricular nerve may be required; likewise, if more than 50% of the thickness of the nerve has been disrupted, replacing the injured segment with a cable graft is recommended.[17][24] Regardless of whether or not patients with temporal bone fracture-associated facial paralysis undergo decompression, a two-week course of high-dose oral steroids (prednisone 60 mg daily) should be prescribed.[1][16]
Length of convalescence and degree of recovery are variable, depending greatly on the extent of the injury and the patient's overall health. In some cases, it may be useful to place an eyelid weight in order to help prevent corneal ulceration or exposure keratopathy.[25] Most patients will ultimately recover function to House-Brackmann grades I-III, and therefore, many will be able to have the weight removed at a later time.[16][17]
Other indications for operative intervention in temporal bone fractures include CSF leak refractory to 14 days of conservative management (head of bed elevation and lumbar drain placement), hemorrhage refractory to packing, ossicular chain disruption, persistent tympanic membrane perforation, external auditory canal stenosis, and entrapment of epithelium that places the patient at risk for cholesteatoma development.
Differential Diagnosis
The differential diagnosis for facial paralysis is long and broad, but acute facial paralysis in the setting of head trauma is rarely a result of anything other than a temporal bone fracture.[25] Head injury may also result in cerebrovascular accidents, with pontine and brainstem injuries potentially presenting with ipsilateral hemifacial paralysis and cortical injuries causing paralysis of the lower two-thirds of the face on the contralateral side.
However, strokes typically result in multiple neurological symptoms, including other cranial neuropathies, headache, nausea and vomiting, vital sign instability, and potentially limb weakness, rather than isolated facial nerve palsy.[26][27] Other causes of acute facial weakness include viral reactivation syndromes, such as Ramsay Hunt syndrome and Bell's palsy, infectious diseases, such as Lyme disease, human immunodeficiency virus, and polio, autoimmune disorders, such as Guillain-Barré syndrome and multiple sclerosis, iatrogenic injury, and neoplasms.[28][29][27]
Similarly, the differential diagnosis for acute hearing loss or vertigo is broad. It includes barotrauma, noise trauma, cholesteatoma, sudden sensorineural hearing loss, superior semicircular canal dehiscence syndrome, autoimmune inner ear disease, labyrinthitis, Ménière's disease, BPPV, neoplasm, and many others.[30][31][32][33][34][35] Again, however, the history of recent head trauma should focus the clinical evaluation on ruling out a temporal bone fracture. Clear otorrhea with or without rhinorrhea may also result from otitis externa or neoplasm, but ruling out a CSF leak in the setting of head injury is a critical step in managing trauma patients.
Staging
As discussed above, temporal bone fractures have been historically classified using the transverse vs. longitudinal scheme with limited success. Currently, most clinicians classify these fractures as otic capsule sparing or otic capsule disrupting.[36][37] In 1997, Yanigahara and colleagues developed the following system to classify temporal bone fractures, specifically in patients with post-fracture facial paralysis:[4]
- Type 1: A fracture line travels across the mastoid process.
- Type 2: A fracture line travels across the mastoid process and extends to the external auditory canal.
- Type 3: A fracture line extends across the mastoid cortex and the external auditory canal to the pyramidal or horizontal portion of the facial nerve.
- Type 4: A fracture travels across the tegmen of the middle ear and the antrum with the involvement of the geniculate ganglion. The facial nerve between the labyrinthine segment and the horizontal segment is involved. Type 4 is further subdivided into types 4A and 4B:
- Type 4A: No direct injury of the inner ear or internal auditory canal.
- Type 4B: The inner ear and/or the internal auditory canal are directly violated. The typical type 4B corresponds with the classic transverse fracture.
Prognosis
Most patients with temporal bone fracture-associated facial paralysis will demonstrate recovery, often with synkinesis. Only patients who present with House-Brackmann grade VI paralysis are at risk for a final outcome of House-Brackmann grade VI paralysis, but even the majority of these patients improve to House-Brackmann grade III function or better.[17][20] Patients who present with immediate House-Brackmann grade VI paralysis are at the greatest risk of complete failure to recover because as long as the facial nerve is at least partially intact after the fracture, axonal regeneration will occur. At least some movement will be restored.
Conversely, according to Brodie and Thompson, when paralysis develops in a delayed fashion, regardless of how severe it is or if the paralysis is incomplete (House-Brackmann grade II-V), the worst the final outcome will be is House-Brackmann grade II function[3]. When patients meet ENoG severity criteria for decompression, their outcomes tend to be poorer than if they do not. Patients who underwent surgery in a 2001 series published by Darrouzet et al. had an 86.2% chance of recovery to House-Brackmann grade III function or better by one year and a 93.8% chance by two years after injury. This result contrasts notably with their patients who were managed with steroids and did not meet eligibility criteria for surgical facial nerve decompression; these patients had a 98% chance of returning to House-Brackmann grade III function or better by one month after injury and a 100% chance of recovery to House-Brackmann grade II function or better by one year.[17]
A systematic review published in 2010 by Nash et al. looked more specifically at rates of return to normal function: their patients requiring and undergoing surgery had a 23% chance of returning to House-Brackmann grade I (normal) function; patients not requiring surgery and receiving steroids only had a 67% chance of returning to House-Brackmann grade I function, and patients who were only observed had a 66% chance of returning to House-Brackmann grade I function.[20]
Complications
The primary long-term sequela of facial nerve injury from a temporal bone fracture is facial synkinesis, manifested by voluntary movements accompanied by involuntary movements, spasms, tension, and soreness. Synkinesis is caused by aberrant reinnervation during the axonal regeneration process, specifically when an axon either regenerates such that it connects to the motor end plate of a muscle to which it was not previously connected or when a single axon connects to multiple motor endplates in the correct muscle, the incorrect muscle, or a combination of both.[38] Having more axons than normal terminating in a given muscle results in higher resting tone in the muscle, which can cause tension and soreness; having axons terminate in the incorrect muscle results in involuntary and dyscoordinated movements.[39][40] Synkinesis is typically managed with physical therapy and chemodenervation but can also be treated with surgical procedures, such as selective neurectomy and nerve or even muscle transfer.[41][42]
While synkinesis is the most common result of incomplete recovery, flaccid weakness may persist after temporal bone fracture in some patients, and this may subsequently necessitate facial reanimation procedures such as eyelid weight placement, static facial suspension, nerve transfer (such as masseteric or hypoglossal), or muscle transfer (such as temporalis or gracilis).[43][44][45][46][47] Regardless of whether synkinesis or flaccidity persists, the impact of substantial facial asymmetry on social function can have profound and lasting behavioral health implications for many patients and must be addressed by the treating physician.[43][48]
Other potential complications of temporal bone fracture include long-term hearing loss, which may require rehabilitation with hearing aids or even cochlear implantation, vestibular dysfunction and persistent imbalance, cholesteatoma from entrapped middle ear epithelium, external auditory canal stenosis, and meningitis from chronic CSF leak. Closed head injury may also result in neurocognitive sequelae and/or post-concussive syndrome.
Postoperative and Rehabilitation Care
As with any blunt head injury, rehabilitation can be a critical part of recovery after a temporal bone fracture. Patients may require physical and occupational therapy after concussion; vestibular rehabilitation may also be useful, particularly in the event of otic capsule disruption. If hearing loss occurs as a sequela of temporal bone fracture, audiological care will be needed, and this may include fitting hearing aids or programming and managing cochlear implants. Follow-up should also include monitoring for CSF leaks or observing a known leak and ensuring signs of meningitis do not develop. Cerebrospinal fluid leaks do not necessarily require prophylactic antibiotics, but a high index of suspicion should be maintained for meningitis because the risk of infection is higher in patients with CSF fistulae.[49] Additionally, patients should be monitored for cholesteatoma formation, which can result from middle ear epithelium trapped within a fracture line.
With respect to facial paralysis, patients who recover some movement but do not recover completely normal function may require rehabilitation therapy for synkinesis or chemodenervation.[39][40] If patients fail to recover any movement and flaccid paralysis persists in the long term, numerous strategies exist to restore function, ranging from placement of eyelid weights to brow lifting and both static and dynamic reanimation or reinnervation of the face.[43][50][51][52]
Consultations
While temporal bone fractures may occur as isolated injuries, they more often occur in conjunction with polytrauma, and therefore patients with temporal bone fractures frequently require care from multiple specialists.[8] Otolaryngologists are best suited to manage some of the sequelae of the temporal bone fracture itself - facial paralysis and hearing loss - but neurosurgeons may be required to attend to CSF leaks and other intracranial injuries, which occur with up to 90% of temporal bone fractures.[53]
Neurologists may likewise be consulted for concussions and orthopedists and trauma surgeons for other injuries that may occur simultaneously. Longer-term care will also likely involve physical and occupational therapists and may require audiologists, vestibular therapists, and others.
Deterrence and Patient Education
The single most important piece of education that can be provided to patients to help prevent temporal bone fractures is emphasizing the importance of helmet wear when performing activities such as cycling, skateboarding, skiing, rollerblading, and riding snowboards, horses, motorcycles, and all-terrain vehicles. Numerous studies have shown that helmet use decreases rates of skull fracture in patients who sustain head injuries while performing various sporting and industrial activities.[54][55]
Enhancing Healthcare Team Outcomes
Temporal bone fractures are often seen in the emergency department, but their management requires an interprofessional team that includes a neurologist, specialty nurses, trauma surgeon, neurosurgeon, otolaryngologist, and intensivist. Most of these fractures are associated with concomitant injury to the face, spine, and chest; appropriate specialists for these injuries should be involved. The trauma and critical care services monitor patients and notify the other specialists of clinical developments. Besides the injury to the facial nerve, other complications include CSF leak, meningitis, and cholesteatoma formation. The prognosis for non-displaced temporal bone fractures is good, but displaced fractures with nerve involvement may require surgical decompression. Surgery may be associated with complications, and recovery is often protracted.[24]
ALl interprofessional team members must carefully follow and monitor that patient's condition and progress, noting their observations in the patient's permanent health record so that all team members can access the same up-to-date data. Additionally, any status changes must promptly be communicated to the appropriate interprofessional team members so additional therapeutic interventions can be implemented if necessary. This interprofessional interaction will help drive optimal patient outcomes for these injuries. [Level 5]