Continuing Education Activity
Diverticulosis is a clinical condition in which multiple sac-like protrusions (diverticula) develop along the gastrointestinal tract. Though diverticula may form at weak points in the walls of either the small or large intestines, the majority occur in the large intestine (most commonly the sigmoid colon). The majority of individuals with diverticulosis are asymptomatic. Diverticular disease occurs when there is symptomatic diverticulosis (e.g., diverticular bleeding); diverticulitis (e.g., acute or chronic inflammation that may or may not is complicated by abscess formation, fistula formation, bowel obstruction, or perforation); or associated segmental colitis (e.g., inflammation in segments of the mucosal segments of the colon in between diverticula). This activity reviews the causes, pathophysiology, and diagnosis of diverticulosis and highlights the interprofessional team's role in managing these patients.
Objectives:
- Review the causes of diverticulosis.
- Describe the workup of a patient with diverticulosis.
- Summarize the treatment options for diverticulosis.
- Explain the importance of improving care coordination among interprofessional team members to improve outcomes for patients affected by diverticulosis.
Introduction
Diverticulosis is a clinical condition in which multiple sac-like protrusions (diverticula) develop along the gastrointestinal tract. Though diverticula may form at weak points in the walls of either the small or large intestines, the majority occur in the large intestine (most commonly the sigmoid colon).
The majority of individuals with diverticulosis are asymptomatic. Diverticular disease occurs when there is symptomatic diverticulosis (e.g., diverticular bleeding); diverticulitis (e.g., acute or chronic inflammation that may or may not is complicated by abscess formation, fistula formation, bowel obstruction, or perforation); or associated segmental colitis (e.g., inflammation in segments of the mucosal segments of the colon in between diverticula).[1][2][3]
Etiology
Diverticulosis is thought to occur due to peristalsis abnormalities (e.g., intestinal spasms), intestinal dyskinesia, or high segmental intraluminal pressures. Although the exact cause is unknown, some environmental and lifestyle risk factors have been linked to this condition.[4][5] Several studies have suggested that a diet low in fiber and high in red meat may be associated with an increased risk of diverticulosis, although a diet high in fiber will not reduce the symptoms of an uncomplicated diverticular disease. In patients with symptomatic complicated diverticular disease (e.g., inflammation or bleeding), there may be a benefit from a diet high in fiber by decreasing overall inflammation and favorably changing the intestinal microbiota.
The risk of diverticulitis and bleeding is significantly higher in patients with obesity or larger waist circumference. Smokers have been noted to have an increased incidence of diverticular abscess formation or perforation. Medications associated with an increased risk of diverticular bleeding or diverticulitis include nonsteroidal anti-inflammatory drugs, opiates, and steroids.
Epidemiology
The prevalence of diverticulosis is highest in the Western world and in countries that follow a more Western lifestyle. Diverticulosis affects 5% to 45% of individuals in the Western world, depending on both the method of diagnosis and the age of the individual. In general, the prevalence of diverticulosis increases with age from under 20% of individuals affected at age 40 up to 60% of individuals affected by age 60. Approximately 95% of patients in the Western world with diverticulosis have diverticula in the sigmoid colon. Of all of the patients with diverticulosis, 24% have diverticula involving mainly the sigmoid colon, 7% have diverticula spread evenly throughout the colon, and 4% have diverticula located only proximal to the sigmoid colon.[6][7]
In Asia, diverticulosis has a prevalence of approximately 13% to 25%. Individuals with diverticulosis in this region also tend to have predominantly right-sided colonic diverticula (unlike the Western world where left-sided diverticula are much more common). Approximately 5% to 15% of patients with diverticulosis experience bleeding. A third of which experience massive bleeding. In 50% to 60% of patients experiencing diverticular bleeding, the source is right-sided diverticula, possibly due to the thinner wall of the right-sided colon or the wider neck and domes of right-sided diverticula (e.g., an increased surface area of exposure of the vasa recta to potential injury).
Diverticulitis occurs in approximately 4% to 15% of patients with diverticula, and the incidence increases with age. On average, patients admitted for diverticulitis are about 63 years old. The overall incidence of diverticulitis continues to rise, with a 26% jump from 1998 to 2005, and the largest increases were seen in patients between the ages of 18 to 44 years. Under the age of 50, diverticulosis is more common in males, whereas between the ages of 50 to 70, the disease is seen slightly more often in females. Over the age of 70, there is a significantly greater incidence of diverticulosis in females.
Pathophysiology
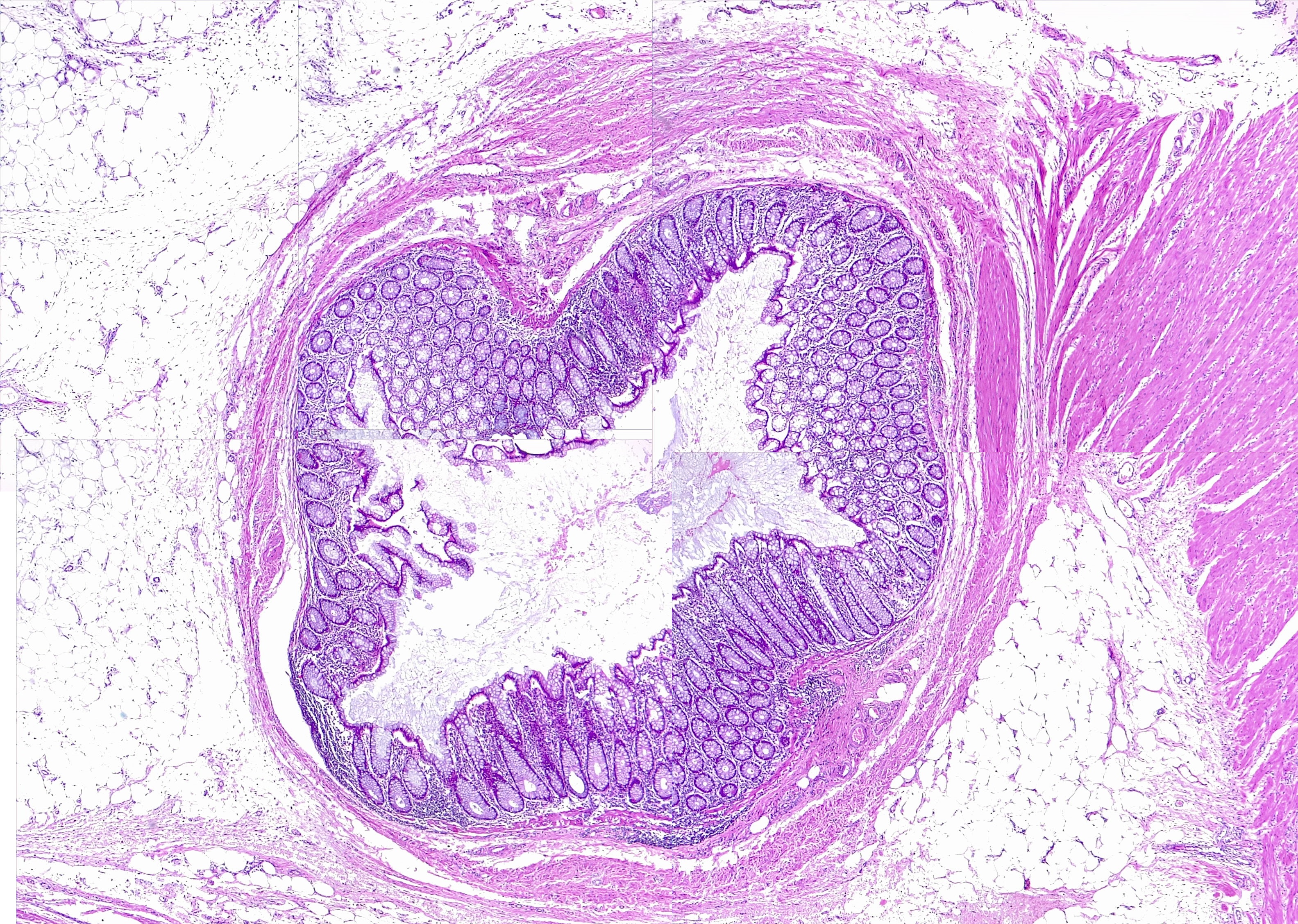
Diverticula occur in weaker portions of the colonic wall where the vasa recta infiltrate the circular muscular layer. The vast majority of colonic diverticula are typically “false” diverticula, which are mucosa and submucosa herniating through a defect or weakness in the muscularis layer, covered externally only by serosa. True diverticula are much more uncommon (e.g., Meckel’s diverticulum) and involve outpouching of all layers of the intestinal wall (e.g., mucosa, muscularis, and serosa).[8]
A major predisposing factor for the formation of colonic diverticula is abnormal colonic motility (e.g., intestinal spasms or dyskinesis), resulting in exaggerated segmental muscle contractions, elevated intraluminal pressures, and separation of the colonic lumen into chambers. As the sigmoid colon is the colon segment with the smallest diameter, it is also the segment with the highest intraluminal pressures. Connective tissue disorders such as Marfan syndrome, Ehlers-Danlos syndrome, or autosomal dominant polycystic kidney disease may also predispose an individual to colonic diverticula formation as these diseases often involve structural changes (e.g., weakness) in the intestinal wall.
Diverticula are prone to bleeding due to the proximity of the vasa recta to the intestinal lumen as a result of herniation of the mucosa and submucosa through the muscularis layer. With diverticula formation, the vasa recta become separated from the intestinal lumen by a layer of mucosa alone and are exposed to a greater amount of injury. This results in eccentric intimal thickening, thinning of the media, and ultimately segmental weaknesses along these arteries, which predispose the vasa recta to rupture and bleeding into the intestinal lumen. Diverticular bleeding typically occurs in the absence of diverticular inflammation or infection (i.e., diverticulitis).
Diverticulitis typically results from micro- or macroscopic perforation of a diverticulum, which may or may not result from obstruction (e.g., by a fecalith). Increased intraluminal pressures or inspissated (thickened and condensed) food matter, with resultant inflammation and focal necrosis, ultimately result in diverticular perforation. Associated inflammation is usually mild, and pericolic fat and mesentery tend to wall off the perforations of the diverticula. This may or may not result in abscess or fistula formation, or intestinal obstruction. In rare cases, perforations may be large and uncontained and lead to peritonitis.
Histopathology
The mucosa of the diverticulum and the surrounding colon exhibit changes on histologic and tissue levels. Diverticular mucosa undergoes expansion of the lamina propria due to the accumulation of lymphoplasmacytic infiltrates. Histologic changes also include mucin depletion, the development of lymphoglandular complexes, and focal Paneth cell metaplasia. Acute inflammation is seen in the form of cryptitis and crypt abscesses. Hemorrhage may be seen in the diverticula and surrounding tissue. Scarring is evident in areas of resolved inflammation. In the mucosa surrounding the orifices of diverticula, we see additional changes, including pseudohypertrophy of the circular muscle leading to mucosal fold exaggeration and muscularization of the lamina propria, hyperplasia of the glands, and hemosiderin deposits, which are seen in the submucosa. The features are usually indistinguishable from those of inflammatory bowel disease.
History and Physical
Most individuals with diverticulosis do not have any symptoms, and the condition itself is not dangerous. However, some patients may experience unexplained abdominal pain or cramping, alterations in bowel habits, or notice blood in the stool. Any bleeding associated with diverticulosis is painless. A diagnosis of diverticulosis is suspected when a patient presents with a history of painless rectal bleeding or unexplained abdominal pain or cramping, or alterations in bowel function.
Acute diverticulitis (e.g., inflammation, infection, or perforation) is typically suspected when a patient presents with lower abdominal pain (particularly on the left side). Patients may additionally present with abdominal tenderness to palpation and an elevated white blood cell count (leukocytosis). An abdominal CT will help differentiate between complicated versus uncomplicated disease in this case.
Evaluation
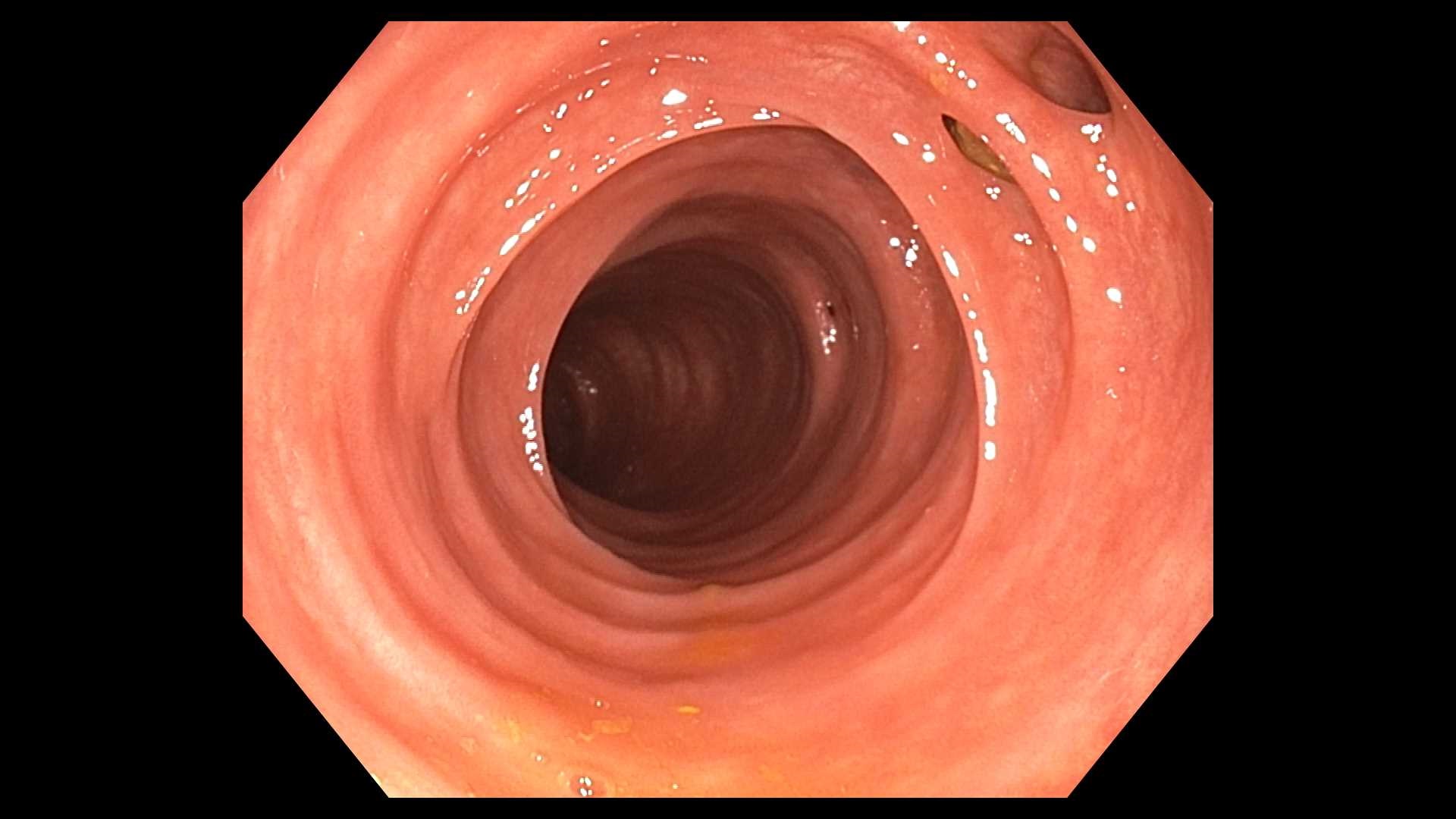
A diagnosis of diverticulosis is suspected based on clinical presentation (e.g., a history of painless rectal bleeding or unexplained abdominal pain and cramping, altered bowel movements) and may be confirmed by colonoscopy or an X-ray following a barium enema. If the patient presents with extreme abdominal pain, however, the test of choice is typically a CT of the abdomen to avoid the risk of intestinal rupture in the setting of intestinal infection or inflammation.[9]
Colonoscopy in a prepped colon remains the best test to identify the source of bleeding if blood is present in the stool. If a colonoscopy is inconclusive, as with the acute or severe bleeding, angiography, CTA, or radionuclide scanning may be considered to locate the source.
Patients presenting with acute diverticulitis may require additional treatment. Uncomplicated diverticulitis is treated non-operatively, with either intravenous (IV) or oral (PO) antibiotics. Complicated diverticulitis (e.g., with an associated fistula, abscess, obstruction, or perforation) may, in addition to antibiotic therapy, require hospitalization and/or surgery to treat the associated complication.[10][11] Similarly, patients presenting with sepsis, immunosuppression, advanced age, significant comorbidities, high fever (greater than 39.2°C), significant leukocytosis, inability to tolerate oral intake, non-compliance, or failed outpatient treatment, may require hospitalization for proper treatment.
Treatment / Management
Treatment is typically aimed at reducing intestinal spasms, which is potentially achievable by increasing fiber and fluids in the diet. Greater intestinal bulk reduces the number of spasms, and as a result, decreases intestinal pressures. Studies found no positive or negative association between diverticular disease and consumption of nuts, grains, potassium, β-carotene, vitamin C, and magnesium. Data related to the association between diverticular disease and alcohol and red meat consumption is controversial. Most bleeding associated with diverticulosis is self-limiting and does not require intervention. In some cases, however, endoscopic, radiologic, or surgical intervention may be required to stop persistent bleeding ((e.g., injection, coagulation (cautery, argon plasma coagulator), or mechanical devices (clips, bands, loops)). If a source cannot be determined in the case of recurrent bleeding, surgery may be considered to remove portions of the affected intestine (e.g., colectomy). Similarly, in the case of a giant diverticulum, with an increased risk of infection and rupture, surgery is more likely to be considered.[4][12]
Differential Diagnosis
Diverticulosis presents with bleeding per rectum, and most of the time, that is the only presenting symptom. The differential diagnosis includes:
- Hemorrhoids
- Ulcers in the gut wall
- Inflammatory bowel disease
- Anal fissure
- Anal abscess or fistula
- Colonic polyps
- Colon cancer
- Constipation
- Radiation therapy
- Angiodysplasias
- Colitis
- Proctitis
Pertinent Studies and Ongoing Trials
Diverticula are usually seen on colonoscopy. Recent studies have shown that the detection rate of colonoscopy for left-sided diverticular disease is lower than barium enema. Follow-up barium enema for diverticular disease of the left colon is a potential area to study and improve clinical practice.
Staging
Diverticular disease is classified based on whether it is uncomplicated diverticulosis or it has been complicated by diverticulitis. A summary is given below;
- Type 0: Asymptomatic diverticulosis
- Type I: Acute uncomplicated diverticulitis
- Type II: Acute complicated diverticulitis
- Type III: Chronic diverticular disease
Complicated diverticular disease is further classified using the Hinchey classification system, which is largely based on CT findings.
- Stage 1: Phlegmon (1a) or diverticulitis with pericolic or mesenteric abscess (1b)
- Stage 2: Diverticulitis with walled-off pelvic abscess
- Stage 3: Diverticulitis with generalized purulent peritonitis
- Stage 4: Diverticulitis with generalized fecal peritonitis
Prognosis
Diverticulosis is usually asymptomatic, or it may cause episodes of bleeding. Approximately fifteen percent will develop diverticular bleeding. If inflammation develops within the diverticula, around eighty-five percent of people will respond to medical treatment. The remaining people may need a surgical procedure to get the inflamed diverticula fixed. Overall, the prognosis for most patients is good as long as they change their lifestyle, become physically active, eat a high fiber diet, and avoid constipation.
Complications
Diverticulosis usually remains asymptomatic or causes bleeding through the rectum. The symptomatic uncomplicated diverticular disease presents with constant abdominal pain attributed to diverticula in the absence of colitis or diverticulitis. Segmental colitis is the inflammation in the diverticular mucosa without the involvement of the diverticular orifices. Diverticulitis is defined as the inflammation of a diverticulum. It can be acute or chronic, uncomplicated, or complicated. Diverticulitis is complicated by an abscess, fistula, bowel obstruction, or free perforation. Inflammation within the diverticula may result in the formation of a fistula between the colon and adjacent viscera. Fistulas most commonly involve the bladder resulting in a colovesical fistula, or vagina causing a colovaginal fistula. Colovesical fistula presents with pneumaturia, fecaluria, or dysuria. Patients with a colovaginal fistula may experience the vaginal passage of feces or flatus.
Consultations
A diagnosis of diverticulosis often requires interdisciplinary care. Primary care doctors are front line providers who see these patients. Gastroenterologists and general surgeons get involved if the diverticular disease gets complicated. Infectious disease helps determine what antibiotics would help patients with the right selection of antibiotics if the disease is refractory to standard regimens.
Deterrence and Patient Education
Diverticulosis describes the presence of diverticula, which is a pouch-like structure that can form from the points of weakness through the muscular wall of the colon. Diverticulosis usually affects men and women equally. People with diverticulosis who do not have symptoms do not require treatment. It is not a normal finding to see blood in the stool. This can be a sign of several conditions, some of which are serious and require immediate treatment. Anyone who experiences this should see his/her healthcare provider to get the appropriate evaluation done. Diverticular bleeding occurs when an artery located within a diverticulum gets eroded and bleeds into the lumen of the colon, causing painless bleeding from the rectum. Most clinicians recommend increasing fiber content in the diet, which can help increase the bulk of the stools. Fiber also helps to control the recurrence of symptoms. Patients with diverticular disease are also advised to avoid seeds, corn, and nuts because of the belief that these foods could cause diverticulitis. However, recent studies do not prove this association.
Enhancing Healthcare Team Outcomes
The prevalence of diverticulosis is very high, and while the disorder is asymptomatic, it can present with painless bleeding or progress into an inflammatory state. Because of the enormous healthcare costs in managing complications of diverticulosis, the condition is managed by an interprofessional team.
A dietitian must be consulted to educate the patient on a high-fiber diet. The pharmacist should educate the patient on the avoidance of medications that cause constipation. The nurse should educate the patient on avoiding smoking, drinking ample water, and becoming more physically active, all of which lead to less constipation. The clinician should educate the patient on the potential complications of diverticulosis and the associated healthcare costs. Once a patient has been diagnosed with diverticulosis, the patient should be seen by the interprofessional team to ensure that the patient has acquired sufficient knowledge in preventing complications.
These simple recommendations can help avoid complications like bleeding and diverticulitis. Finally, it is important to inform the patient that when surgery is undertaken for a complication of diverticulosis, there is always a risk of a stoma, which can seriously impair the quality of life.[13][14]