Continuing Education Activity
Electrical injuries are when high-energy current travels through the body due to contact with an electrical source. Injuries occur due to either the flow of current through the body, arc flash, or clothing that catches fire. With the former two, the body converts electricity to heat, which results in a thermal burn. It is important to consider that the outward appearance of an electrical burn does not accurately predict the true extent of the injury, as internal tissues or organs may be much more severely burned than the skin. This activity reviews the pathophysiology, presentation, and treatment options available for electrical burns and highlights the role of the interprofessional team in its management.
Objectives:
- Describe the pathophysiology of electrical burns.
- Summarize the steps in the evaluation of a patient with an electrical burn.
- Review the treatment and management options available for electrical burns.
- Explain the importance of improving care coordination among interprofessional team members to improve outcomes for patients affected by electrical burns.
Introduction
Electrical injuries are when high-energy current travels through the body due to contact with an electrical source. Injuries occur due to either the flow of current through the body, arc flash, or clothing that catches fire. With the former two, the body converts electricity to heat, which results in a thermal burn. It is important to consider that the outward appearance of an electrical burn does not accurately predict the true extent of the injury, as internal tissues or organs may be much more severely burned than the skin.
It is important to note that the term “electrocution” refers only to a person who is killed as a result of exposure to electricity. Thus, someone who is exposed to electricity but survives has not been “electrocuted.”
Etiology
Electrical injuries occur when the human body comes in contact with an electrical source, either directly or through material that is a conductor. For example, a utility worker may fall from a bucket truck and instinctively grab a power line to catch himself, causing electrical injury; alternatively, the worker may be holding a pole that comes in contact with a power line, causing him to sustain electrical injury. More commonly, a person becomes a victim of electrical injury at home, such as when an electrical cord on an appliance becomes exposed and makes contact with the human body or when an electric source contacts water that an individual is in contact with as well, such as a hair dryer falling into a bathtub.
Epidemiology
Of all burns treated in a medical setting, 4% to 5% are electrical [1]. In the United States, accidental high voltage electrical injuries account for approximately 400 deaths per year. The total number of electrical deaths is approximately 1,000 yearly in the United States. Electrical injuries in adults are most commonly occupational; in children, household electrical injuries are most common. Males are more commonly injured via electricity than females[2]. The hands are the most common source point, followed by the head. Feet are usually the ground point.
Pathophysiology
Ohm’s Law states that current is directly proportional to voltage and inversely proportional to resistance. All three contribute to the pathophysiology of how electricity creates burns to the body. Contributing factors to the severity and pattern of injury include body position compared to the direction of current entering the body and duration of exposure to current.
Type of Current
Low-frequency alternating current (AC) causes more extensive injury to tissues than does high-frequency AC or direct current (DC). This is because low-frequency AC causes ongoing local muscle contraction (flexor muscles greater than extensor muscles) at the site of contact with the electrical source, often rendering the victim unable to let go of the offending object. In addition, AC injuries are much more common, as AC powers households and other buildings.
DC causes a single strong muscle contraction, often throwing its victim away from the energy source. The most common examples of DC injuries include lightning strike and contact with a car battery. Of note, the risk of death and/or severity of injury from lightning strike depends on many factors, such as if the exposure was a direct lightning strike or the lightning hit something else nearby (tree/structure/ground) and then traveled to the individual’s body.
Voltage and Amperage
Burns can be classified as high or low voltage. High voltages greater than 500-1000 Volts cause deep burns and extensive deep tissue and organ damage. Low voltage exposures tend to result in lesser injury. United States households are supplied with voltages in the 110 to 220 range which causes muscle tetany and can lead to prolonged exposure to the electrical source, as the patient cannot let go. From an external source, it takes only 60 to 100 milliamps of low-frequency AC or 300 to 500 milliamps of DC to induce ventricular fibrillation. For an internal source (pacemaker), it takes less than 1 milliamp to induce ventricular fibrillation.
Resistance
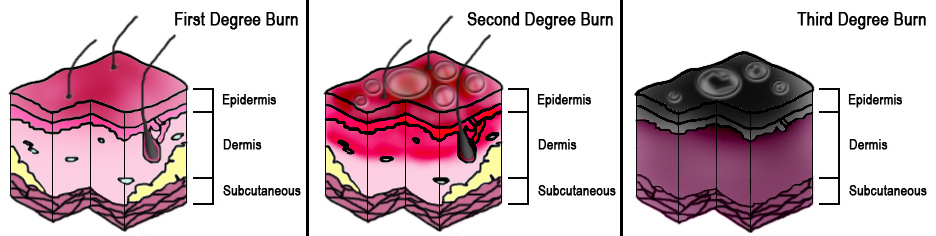
Electricity, the path of least resistance; thus, most injuries occur to tissues with the least amount of resistance. Skin is the tissue with the most amount of resistance in the human body, followed by bone. Nerves, muscle, and blood have the least amount of resistance. Further reinforcing this concept is that moist tissues (muscle) have much lower resistance than dry tissues (skin). Higher skin resistance results in more diffuse burns to the skin. Lower skin resistance results in deeper burns that are more likely to involve internal organs. Whether skin is relatively dry or moist, electricity passes through the highly-resistant skin tissue and then spreads out through the underlying tissues with less resistance. Therefore, skin burns can appear mild when internal tissues and organs are severely damaged.
History and Physical
Patients with electrical burns should be examined and treated following trauma patient treatment protocols with priority to ABCDEs with a primary and secondary survey.
A thorough history should be obtained, including the source of patients electrical injury, the voltage and current type (AC or DC) of the energy source, the duration of electrical exposure, and how the injury was incurred. It is also important to obtain the patient's cardiac history, including any history of prior arrhythmias. A head-to-toe examination should also be completed, giving particular attention to the skin, including the scalp.
The patient will usually present with burns that are indistinguishable from thermal burns, except they may have a pattern counsistent with body part in contact with the source and the ground. For example, the patient may have burns on the hands from contact with the electrical source. The electricity then travels through the tissues of their body, causing injury. Finally, the electricity causes a burn where it exits the body, commonly on the feet, which are the “ground.” These patients are specifically at risk for cardiac damage if the path of the current traversed the heart. Patients may also present with injuries from falls caused by the electrical shock, such as long bone fractures, spinal fractures, or joint dislocations (classically posterior shoulder dislocations). Of note, patients who have experienced injuries from electrical shock may have no external injuries at all, such as when a person who drops a hair dryer in the water while in a bathtub.
When documenting wounds, one should refer to areas of burns as “contact points” rather than entrance wounds and exit wounds.
Evaluation
EKG, cardiac enzymes, CBC, and urinalysis (to check for myoglobin due to rhabdomyolysis) should be obtained. Any patient that was in contact with a high voltage source should have continuous cardiac monitoring during evaluation. One may also consider CT imaging of the head if the patient has altered mental status or associated head trauma from a fall or being thrown in a blast.
Treatment / Management
The number one priority is to treat the patient without putting rescuers at risk of injury. Immediate treatment includes the following:
- Remove the patient from the source of electricity (shut off the power source)
- Remove the patient's clothing, especially any metal that is in contact with the body (jewelry or equipment).
- Next, ACLS should be followed for patients without a pulse.
- In a conscious patient, pain control and fluid management (preferably Lactated Ringers) would be priorities.
- Large-bore IV access and large-volume fluid resuscitation is important in patients with anything more than a very minor low-voltage injury.
Fluids should be titrated to produce adequate urine output (75 to 100 mL/hr in adults or 1 mg/kg/hr in children). Avoid hypothermia in these patients. Patients who are pregnant, have chest pain, have a history of cardiac arrhythmias, or have a history of heart disease, or those with high voltage exposure should be placed on a cardiac monitor and observed for 6 to 12 hours. Pregnant patients at greater than 20 weeks gestation should also be placed on a fetal monitor, especially if exposed to high voltage. Patients with severe burns should be referred to the nearest burn center.
Since internal injuries are more difficult to interpret in patients with electrical injuries vs simple thermal burns, one should have a lower threshold for transfer to a burn center overall. If the patient is stable during monitoring, has no concerning findings on labs, and has unremarkable EKG, he or she may be discharged after the burns have been treated, injuries have been addressed, and the tetanus vaccination has been updated.
Differential Diagnosis
Electrical injuries usually cause burns but do not always, thus if one has no external burns, but the history is consistent with an electrical injury, one should not rule out electricity as a differential.
Prognosis
Prognosis varies widely depending on the direction that the current travels through the body, the duration of exposure, the type of current, voltage and amperage of the electrical source, and the resistance of the tissues through which the current travels. This is discussed more under the Pathophysiology section above.
Complications
Complications from electrical injuries are similar to those of other thermal burns, such as infection (which can progress to sepsis), compartment syndrome, and rhabdomyolysis (due to extensive muscle damage from internal burns). Additionally, one may have associated injuries from being thrown from the electrical source or from falling from a height (roof, bucket truck, ladder) due to the electrical shock, and these injuries (long bone fractures, spinal fractures, lacerations, pneumothorax, etc.) should be assessed and treated appropriately.
Cardiac complications can occur. One can have an arrhythmia, possibly even a fatal arrhythmia, at the time of the injury. Anyone who experiences an arrhythmia or any chest pain or other typical cardiac-related symptoms is also at risk of arrhythmia in the 24 to 48 hours following the injury. Thus these patients should be kept on a cardiac monitor at all times. Any high voltage injury should have continuous cardiac monitoring for a minimum of 8 hours [3].
A special consideration is pediatric electrical injuries that occur as the result of a child putting a cord in the mouth and biting down, causing burn injury to the corners of the mouth. These patients can be sent home if there are no other associated injuries, however, the complication in this case to warn parents about is delayed bleeding from the labial artery, which can occur about 7 days following the date of injury.
Due to the complicated nature of injury patterns with electrical injuries, anything more than a minor electrical injury should have a qualified trauma and burn center as a final disposition.
Deterrence and Patient Education
There are multiple safety warnings on electrical appliances warning the public about improper use of electrical devices and risk of serious injury or death. These warnings should be heeded. In addition, workplace safety rules should be followed and enforced to help prevent work related electrical injuries in high-risk jobs particularly.
Enhancing Healthcare Team Outcomes
Like many things in medicine, a team approach is best in the complete management of a patient with an electrical burn. There should be open and clear communication between providers regarding wound care from nursing or technicians involved in patient care, airway from respiratory therapy, sedation and analgesia from pharmacy, consultants such as a general surgeon or plastic surgeon, and the primary provider/team caring for the patient.