[1]
Situ-LaCasse E, Grieger RW, Crabbe S, Waterbrook AL, Friedman L, Adhikari S. Utility of point-of-care musculoskeletal ultrasound in the evaluation of emergency department musculoskeletal pathology. World journal of emergency medicine. 2018:9(4):262-266. doi: 10.5847/wjem.j.1920-8642.2018.04.004. Epub
[PubMed PMID: 30181793]
[2]
Partridge DG, Winnard C, Townsend R, Cooper R, Stockley I. Joint aspiration, including culture of reaspirated saline after a 'dry tap', is sensitive and specific for the diagnosis of hip and knee prosthetic joint infection. The bone & joint journal. 2018 Jun 1:100-B(6):749-754. doi: 10.1302/0301-620X.100B6.BJJ-2017-0970.R2. Epub
[PubMed PMID: 29855250]
[3]
Wu T, Dong Y, Song Hx, Fu Y, Li JH. Ultrasound-guided versus landmark in knee arthrocentesis: A systematic review. Seminars in arthritis and rheumatism. 2016 Apr:45(5):627-32. doi: 10.1016/j.semarthrit.2015.10.011. Epub 2015 Dec 17
[PubMed PMID: 26791571]
Level 1 (high-level) evidence
[4]
Zhang Q, Zhang T, Lv H, Xie L, Wu W, Wu J, Wu X. Comparison of two positions of knee arthrocentesis: how to obtain complete drainage. American journal of physical medicine & rehabilitation. 2012 Jul:91(7):611-5. doi: 10.1097/PHM.0b013e31825a13f0. Epub
[PubMed PMID: 22710881]
[5]
Jennings JM, Dennis DA, Kim RH, Miner TM, Yang CC, McNabb DC. False-positive Cultures After Native Knee Aspiration: True or False. Clinical orthopaedics and related research. 2017 Jul:475(7):1840-1843. doi: 10.1007/s11999-016-5194-4. Epub
[PubMed PMID: 27942968]
[6]
Bhavsar TB, Sibbitt WL Jr, Band PA, Cabacungan RJ, Moore TS, Salayandia LC, Fields RA, Kettwich SK, Roldan LP, Suzanne Emil N, Fangtham M, Bankhurst AD. Improvement in diagnostic and therapeutic arthrocentesis via constant compression. Clinical rheumatology. 2018 Aug:37(8):2251-2259. doi: 10.1007/s10067-017-3836-x. Epub 2017 Sep 14
[PubMed PMID: 28913649]
[7]
Shahid A, Malik A, Bukhari A, Shaikh A, Rutherford J, Barkatali B. Do Platelet-Rich Plasma Injections for Knee Osteoarthritis Work? Cureus. 2023 Feb:15(2):e34533. doi: 10.7759/cureus.34533. Epub 2023 Feb 2
[PubMed PMID: 36751575]
[8]
Eker HE, Cok OY, Aribogan A, Arslan G. The efficacy of intra-articular lidocaine administration in chronic knee pain due to osteoarthritis: A randomized, double-blind, controlled study. Anaesthesia, critical care & pain medicine. 2017 Apr:36(2):109-114. doi: 10.1016/j.accpm.2016.05.003. Epub 2016 Jul 30
[PubMed PMID: 27485803]
Level 1 (high-level) evidence
[9]
Yaqub S, Sibbitt WL Jr, Band PA, Bennett JF, Emil NS, Fangtham M, Fields RA, Hayward WA, Kettwich SK, Roldan LP, Bankhurst AD. Can Diagnostic and Therapeutic Arthrocentesis Be Successfully Performed in the Flexed Knee? Journal of clinical rheumatology : practical reports on rheumatic & musculoskeletal diseases. 2018 Sep:24(6):295-301. doi: 10.1097/RHU.0000000000000707. Epub
[PubMed PMID: 29424762]
[10]
Battistone MJ, Barker AM, Grotzke MP, Beck JP, Berdan JT, Butler JM, Milne CK, Huhtala T, Cannon GW. Effectiveness of an Interprofessional and Multidisciplinary Musculoskeletal Training Program. Journal of graduate medical education. 2016 Jul:8(3):398-404. doi: 10.4300/JGME-D-15-00391.1. Epub
[PubMed PMID: 27413444]
[11]
Kontovazenitis PI, Starantzis KA, Soucacos PN. Major complication following minor outpatient procedure: osteonecrosis of the knee after intraarticular injection of cortisone for treatment of knee arthritis. Journal of surgical orthopaedic advances. 2009 Spring:18(1):42-4
[PubMed PMID: 19327266]
Level 3 (low-level) evidence
[12]
Morag Y, Ford MK, Jacobson JA, Jamadar DA. Sonographic diagnosis of an arterioarticular fistula following knee arthrocentesis. Journal of clinical ultrasound : JCU. 2006 May:34(4):207-9
[PubMed PMID: 16615056]
[13]
Tarar MY, Choo XY, Khan S. The Risk of Bleeding Complications in Intra-Articular Injections and Arthrocentesis in Patients on Novel Oral Anticoagulants: A Systematic Review. Cureus. 2021 Sep:13(9):e17755. doi: 10.7759/cureus.17755. Epub 2021 Sep 6
[PubMed PMID: 34659968]
Level 1 (high-level) evidence
[14]
Yui JC, Preskill C, Greenlund LS. Arthrocentesis and Joint Injection in Patients Receiving Direct Oral Anticoagulants. Mayo Clinic proceedings. 2017 Aug:92(8):1223-1226. doi: 10.1016/j.mayocp.2017.04.007. Epub
[PubMed PMID: 28778256]
[15]
Dooley DP. Aspiration of the possibly septic joint through potential cellulitis: just do it! The Journal of emergency medicine. 2002 Aug:23(2):210
[PubMed PMID: 12359298]
[16]
Geirsson AJ, Statkevicius S, Víkingsson A. Septic arthritis in Iceland 1990-2002: increasing incidence due to iatrogenic infections. Annals of the rheumatic diseases. 2008 May:67(5):638-43
[PubMed PMID: 17901088]
[17]
Guyver PM, Arthur CH, Hand CJ. The acutely swollen knee. Part 1: Management of atraumatic pathology. Journal of the Royal Naval Medical Service. 2014:100(1):24-33
[PubMed PMID: 24881423]
[18]
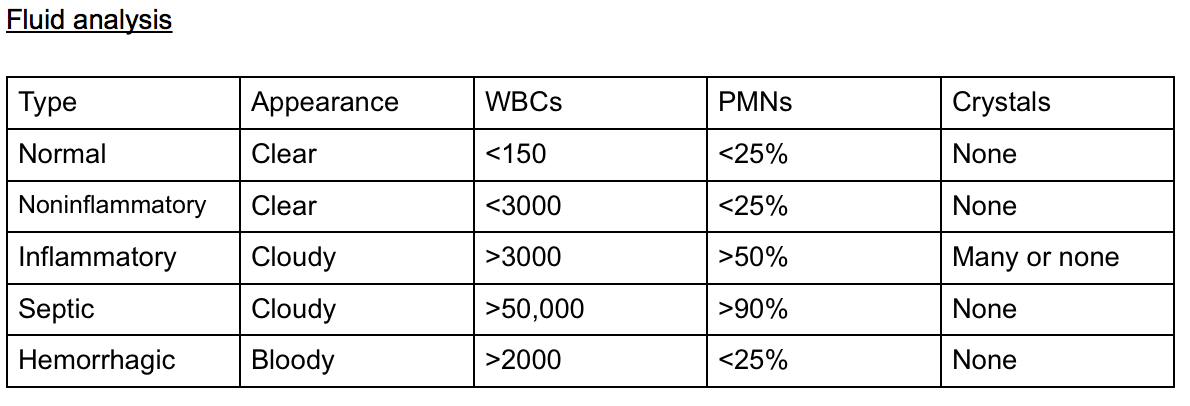
McGillicuddy DC, Shah KH, Friedberg RP, Nathanson LA, Edlow JA. How sensitive is the synovial fluid white blood cell count in diagnosing septic arthritis? The American journal of emergency medicine. 2007 Sep:25(7):749-52
[PubMed PMID: 17870475]
[19]
Margaretten ME, Kohlwes J, Moore D, Bent S. Does this adult patient have septic arthritis? JAMA. 2007 Apr 4:297(13):1478-88
[PubMed PMID: 17405973]
[20]
Baer PA, Tenenbaum J, Fam AG, Little H. Coexistent septic and crystal arthritis. Report of four cases and literature review. The Journal of rheumatology. 1986 Jun:13(3):604-7
[PubMed PMID: 3735282]
Level 3 (low-level) evidence
[21]
Eren TK, Aktekin CN. How reliable are the synovial cell count and blood parameters in the diagnosis of septic arthritis? Joint diseases and related surgery. 2023 Aug 21:34(3):724-730. doi: 10.52312/jdrs.2023.1222. Epub 2023 Aug 21
[PubMed PMID: 37750279]
[22]
Darraj H, Hakami KM, Zogel B, Maghrabi R, Khired Z. Septic Arthritis of the Knee in Children. Cureus. 2023 Sep:15(9):e45659. doi: 10.7759/cureus.45659. Epub 2023 Sep 21
[PubMed PMID: 37868524]