[1]
Samánek M,Vorísková M, Congenital heart disease among 815,569 children born between 1980 and 1990 and their 15-year survival: a prospective Bohemia survival study. Pediatric cardiology. 1999 Nov-Dec;
[PubMed PMID: 10556387]
[2]
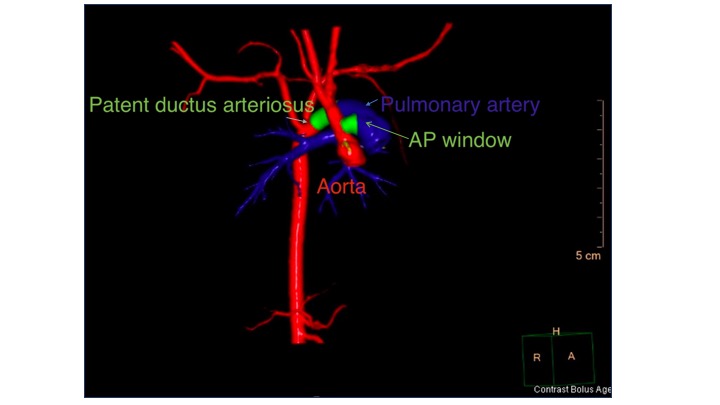
Prabhu S,Keshav M,Ramachandra P,Raj V,John C,Karl TR, Tetralogy of Fallot with pulmonary atresia and aortopulmonary window may mimic common arterial trunk. Cardiology in the young. 2021 Jun 17;
[PubMed PMID: 34134806]
[3]
Sondhi S,Negi PC,Sharma R,Mehta A, Aortopulmonary window with pumonary atresia with ventricular septal defect with D-transposition of great arteries: extremely rare anomaly. BMJ case reports. 2018 Jun 13;
[PubMed PMID: 29898907]
Level 3 (low-level) evidence
[4]
Bin-Moallim M,Hamadah HK,Alhabshan F,Alghamdi AA,Kabbani MS, Aortopulmonary window: Types, associated cardiovascular anomalies, and surgical outcome. Retrospective analysis of a single center experience. Journal of the Saudi Heart Association. 2020;
[PubMed PMID: 33154906]
Level 2 (mid-level) evidence
[5]
Alakhfash AA,Tagelden M,Almesned A,Alqwaiee A, Aortopulmonary window with anomalous right coronary artery from the pulmonary artery. Case report and literature review. Cardiology in the young. 2020 Jan
[PubMed PMID: 31854282]
Level 3 (low-level) evidence
[6]
Grünenfelder J,Zünd G,Vogt PR,Turina MI, Aortopulmonary window with anomalous origin of the right coronary artery. The Annals of thoracic surgery. 1999 Jan
[PubMed PMID: 10086558]
[7]
Rajagopal R,Sinha M,Pandey NN,Bhambri K,Kumar S, Tetralogy of fallot with pulmonary atresia and aorto-pulmonary window: Or is it truncus arteriosus? Journal of cardiovascular computed tomography. 2020 Sep - Oct;
[PubMed PMID: 30385324]
[8]
Trowitzsch E,Schneider M,Urban A,Asfour B, Congenital pulmonary sling, aorto-pulmonary window and pulmonary vein obstruction as a diagnostic and therapeutic challenge in an infant with VACTERL association. Clinical research in cardiology : official journal of the German Cardiac Society. 2006 Jun
[PubMed PMID: 16598388]
[9]
Milovanovic V,Stefanovic I,Ilic S, Tricuspid atresia associated with aortopulmonary window: diagnostic and therapeutic dilemmas. Cardiology in the young. 2017 Apr;
[PubMed PMID: 27680574]
[10]
Van Mierop LH,Kutsche LM, Cardiovascular anomalies in DiGeorge syndrome and importance of neural crest as a possible pathogenetic factor. The American journal of cardiology. 1986 Jul 1;
[PubMed PMID: 3728313]
[11]
Kutsche LM, Van Mierop LH. Anatomy and pathogenesis of aorticopulmonary septal defect. The American journal of cardiology. 1987 Feb 15:59(5):443-7
[PubMed PMID: 3812313]
[12]
Verma B,Abhinay A,Singh A,Kumar M, Double outlet right ventricle and aortopulmonary window in a neonate with Bohring-Opitz (Oberklaid-Danks) syndrome: First case report. Journal of family medicine and primary care. 2019 Mar
[PubMed PMID: 31041292]
Level 3 (low-level) evidence
[13]
Jacobs JP,Quintessenza JA,Gaynor JW,Burke RP,Mavroudis C, Congenital Heart Surgery Nomenclature and Database Project: aortopulmonary window. The Annals of thoracic surgery. 2000 Apr
[PubMed PMID: 10798415]
[14]
Awasthy N,Jawid SA, Aortopulmonary Window with Crisscross Pulmonary Arteries: Anatomically Type 1, Physiologically Type 2. Journal of cardiovascular echography. 2017 Oct-Dec;
[PubMed PMID: 29142813]
[15]
Tongprasert F,Sittiwangkul R,Jatavan P,Tongsong T, Prenatal Diagnosis of Aortopulmonary Window: A Case Series and Literature Review. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine. 2017 Aug;
[PubMed PMID: 28393388]
Level 2 (mid-level) evidence
[16]
Collinet P,Chatelet-Cheront C,Houze de l'Aulnoit D,Rey C, Prenatal diagnosis of an aorto-pulmonary window by fetal echocardiography. Fetal diagnosis and therapy. 2002 Sep-Oct;
[PubMed PMID: 12169817]
[17]
Demir IH,Erdem A,Sarıtaş T,Demir F,Erol N,Yücel IK,Aydemir NA,Celebi A, Diagnosis, treatment and outcomes of patients with aortopulmonary window. Balkan medical journal. 2013 Jun
[PubMed PMID: 25207099]
[18]
Chen J,Guo J,Cao S, Unexplained pulmonary hypertension: an overlooked aortopulmonary window. European heart journal. 2020 Mar 14
[PubMed PMID: 32034904]
[19]
Myers PO,Lador F,Hachulla AL,Bouchardy J,Noble S,Licker M,Pache JC,Kalimanovaska-Ostric D,Djukic M,Kalangos A,Beghetti M, Unrestrictive Aortopulmonary Window: Extreme Presentation as Non-Eisenmenger in a 30-Year-Old Patient. Circulation. 2016 May 10
[PubMed PMID: 27166350]
[20]
Dev M,Sharma M,Rana N, Large Unrepaired Aortopulmonary Window Presenting in Adulthood. Current cardiology reviews. 2020
[PubMed PMID: 31092183]
[21]
Talwar S,Siddharth B,Gupta SK,Choudhary SK,Kothari SS,Juneja R,Saxena A,Airan B, Aortopulmonary window: results of repair beyond infancy. Interactive cardiovascular and thoracic surgery. 2017 Nov 1;
[PubMed PMID: 28633352]
[22]
Zografos PM,Protopapas EM,Hakim NI,Alexopoulos C,Sarris GE, Remarkably Still Repairable Large Aortopulmonary Window in an Adult Patient. World journal for pediatric
[PubMed PMID: 31755375]
[23]
Gangana CS,Malheiros AF,Alves EV,de Azevedo MA,Bernardes RM,Simões LC, Aortopulmonary window--impact of associated lesions on surgical results. Arquivos brasileiros de cardiologia. 2007 Apr
[PubMed PMID: 17546268]
[24]
Gowda D,Gajjar T,Rao JN,Chavali P,Sirohi A,Pandarinathan N,Desai N, Surgical management of aortopulmonary window: 24 years of experience and lessons learned. Interactive cardiovascular and thoracic surgery. 2017 Aug 1
[PubMed PMID: 28475712]
[25]
Talwar S,Agarwal P,Choudhary SK,Kothari SS,Juneja R,Saxena A,Airan B, Aortopulmonary window: Morphology, diagnosis, and long-term results. Journal of cardiac surgery. 2017 Feb
[PubMed PMID: 28139013]
[26]
Konstantinov IE,Karamlou T,Williams WG,Quaegebeur JM,del Nido PJ,Spray TL,Caldarone CA,Blackstone EH,McCrindle BW,Congenital Heart Surgeons Society., Surgical management of aortopulmonary window associated with interrupted aortic arch: a Congenital Heart Surgeons Society study. The Journal of thoracic and cardiovascular surgery. 2006 May
[PubMed PMID: 16678601]
[27]
Uçar T,Karagözlü S,Ramoğlu MG,Tutar E, Transcatheter closure of aortopulmonary window with Amplatzer duct occluder II: additional size. Cardiology in the young. 2020 Mar;
[PubMed PMID: 31928548]
[28]
Trehan V,Nigam A,Tyagi S, Percutaneous closure of nonrestrictive aortopulmonary window in three infants. Catheterization and cardiovascular interventions : official journal of the Society for Cardiac Angiography
[PubMed PMID: 18288731]
[29]
El Dick J,El-Rassi I,Tayeh C,Bitar F,Arabi M, Aortopulmonary window in adults: A rare entity leading to Eisenmenger syndrome. Echocardiography (Mount Kisco, N.Y.). 2019 Jun
[PubMed PMID: 31116466]
[30]
Barnes ME, Mitchell ME, Tweddell JS. Aortopulmonary window. Seminars in thoracic and cardiovascular surgery. Pediatric cardiac surgery annual. 2011:14(1):67-74. doi: 10.1053/j.pcsu.2011.01.017. Epub
[PubMed PMID: 21444051]