Continuing Education Activity
Anisocoria is a condition characterized by unequal pupil size. The etiology of anisocoria is complex, ranging from benign to potentially life-threatening causes. Potential etiologies of anisocoria include systemic drug use, topical ophthalmic drug use, headaches, trauma, ophthalmologic diseases, and autonomic ganglion pathology. This activity examines when anisocoria should be considered on differential diagnosis and how to evaluate it properly and highlights the role of the interprofessional team in caring for patients with this condition.
Objectives:
- Identify the etiology of anisocoria.
- Describe the evaluation of a patient with anisocoria.
- Outline the treatment and management options available for anisocoria.
- Explain the importance of improving care coordination among interprofessional team members to improve outcomes for patients affected by anisocoria.
Introduction
Anisocoria is a term derived from two Greek words, “aniso-” meaning unequal, “kore” meaning pupil, and a Latin suffix “ia” meaning abnormal condition. Anisocoria is characterized by a difference in pupil sizes. This phenomenon results due to disturbances in the efferent pathway dynamics. It can be physiological as well as pathological, occurring due to numerous causes, ranging from benign to life-threatening. This article highlights the neurological as well as the ophthalmological aspects of this condition.
Etiology
Important etiologies of anisocoria include third nerve palsy, Adie pupil, pharmacologic mydriasis, pharmacologic miosis, traumatic mydriasis, physiologic anisocoria, and Horner syndrome.
A third nerve palsy (TNP) may spare the pupil or cause it to dilate with no reaction to light or convergence. Isolated pupillary dilation is not classically considered a third nerve palsy; however, careful evaluation for subtle ptosis or abnormal extraocular movement is necessary to eliminate a TNP using this criterion. The most well-known, life-threatening cause of TNP is a posterior communicating artery aneurysm causing pressure on the third nerve. Patients usually experience pain with this entity. Diagnosis is radiological with computed tomogram (CT) or magnetic resonance imaging (MRI). Magnetic resonance angiogram (MRA) has a threshold of 3 to 5mm and may indicate other pathologies. CTA has a resolution down to 1 to 2 mm. TNP is an example of a large, abnormal pupil.
Tonic pupil, or Adie pupil, is a well-known cause of anisocoria. Here the large pupil is also abnormal. The pupil is large and more commonly occurs in young women. The affected pupil demonstrates a response with poor constriction to light but significantly better to accommodation; this is referred to as light near dissociation. The tonic pupil is often benign but may eventually become miotic. Anatomical abnormalities may exist to cause this entity. The diagnosis of a tonic pupil is usually clinical. There are no cranial nerve palsies in tonic pupil cases.
Pharmacologic agents may cause both mydriasis, which is more common, and miosis. Dilating agents are nasal vasoconstrictors, scopolamine patches, glycopyrrolate deodorants, and various herbals, such as Jimson weed. Small pupils may be caused by opiates, clonidine, organophosphates, pilocarpine, and prostaglandins. Generally, medications taken systemically will not cause anisocoria since both pupils will constrict or dilate but can cause anisocoria if the medication gets into only one eye. The diagnostic approach first involves a careful ophthalmological examination. A dilated pupil can be tested pharmacologically. The muscarinic agent pilocarpine, both dilute (0.05-0.15%) and non-dilute (1 to 2%), acts on the neuromuscular junction of the pupillary constrictor to cause miosis. Dilute pilocarpine will cause constriction in a dilated pupil of greater than two weeks due to denervation of the neuromuscular junction. This previously was thought to help differentiate this form of mydriasis from TNP, but newer results cast some questions on this. If non-dilute pilocarpine fails to constrict the pupil, then the pupil is pharmacologically dilated.
Horner syndrome (HS) involves an abnormally small pupil. Classic clinical findings are unilateral miosis, ptosis, and anhydrosis, which may be present in any combination and also be incomplete and difficult to ascertain. Dilation lag of the pupil in the dark may be helpful (greatest at 5 sec and less at 25 sec). No abnormality of pupillary constriction to light or near occurs. Four percent to 10% of cocaine may be used as one confirmation of the diagnosis, and 0.5 to 1% apraclonidine is also used. Cocaine blocks norepinephrine reuptake, resulting in pupillary dilation 45 to 60 minutes after use. The pupil in Horner will minimally dilate or not dilate at all; post-drop anisocoria of 0.8mm or more is positive. Apraclonidine has different findings; thirty to 45 minutes after use, the abnormal eyelid will rise, and the pupil dilates to “reverse” the deficit. The normal pupil will be unchanged or slightly smaller. Apraclonidine relies on super denervation sensitivity; the minimum time is 36 hours, and it may take a week or longer.
Neither of the above agents is any value in the localization of the lesion in the sympathetic chain. The sympathetic pathway for mydriasis is long. First-order neurons, which originate in the hypothalamus, may be affected by the hypothalamic, brain stem, cervical cord lesions, or other causes. Second-order neurons may be affected by the pathology of the lung, thyroid, sympathetic chain, and other causes. Third-order neurons may indicate carotid pathology or cavernous sinus lesions, or other abnormalities such as a lesion of the sixth nerve. Hydroxyamphetamine (1%) may distinguish third from first- and second-order neuron etiologies. Hydroxyamphetamine releases norepinephrine and causes bilateral pupillary dilation when first- or second-order neurons are involved. Failure for the Horner pupil to dilate indicates third-order neuron dysfunction. Use must wait 48 hours after cocaine or apraclonidine, and false-positive and negative rates are high. Radiological workup involves an MRI of the neck and MRA. Comprehensive imagining in adults extends to the brain, neck, and chest.
Epidemiology
The prevalence of physiologic anisocoria is generally considered to be around 10 to 20%, which does not seem to differ greatly around the world.[1] Physiologic anisocoria does not seem to have a sex predilection nor occurs at a specific age.[2] Physiologic anisocoria is probably the most common cause. The prevalence of other causes of anisocoria is associated with the prevalence of the underlying condition.
Pathophysiology
Distinct pathways control miosis and mydriasis (dilation of the pupil). The parasympathetic pathway causes miosis by activating the iris sphincter. These pathways arise within the brain stem and then extend along cranial nerve III to finally innervate the iris sphincter. This pathway is activated by the pupillary light reflex and accommodation.[3]
Mydriasis is activated by the sympathetic pathway. Sympathetic fibers arise in the hypothalamus, extend to synapse at the C8-T2 spinal cord level, and finally course through the sympathetic chain to synapse with a third neuron in the superior cervical ganglion. Then, these third-order neurons traverse through the cavernous sinus alongside the periarterial carotid plexus until they enter the orbit and travel as the short and long ciliary nerves prior to innervating the dilator pupillae muscle.[4] Although complicated, these pathways illustrate that dilated or constricted pupils are influenced by different anatomical areas and may exhibit different secondary symptoms.[5][6]
As mentioned before, anisocoria can be broken down into three categories:
- An inhibition of constriction of the pupil on one side - the pathological pupil remains larger than the other pupil (pupil is dilated), and this difference is more pronounced in light conditions
- An inhibition of dilatation of the pupil on one side - the pathological pupil remains smaller than the other pupil (pupil is constricted), and this difference is more pronounced in dark conditions
- Difference pupil sizes that in which the difference remains the same in light and dark condition - the anisocoria is more likely to be physiologic with neither pupil having pathology
History and Physical
As with many medical conditions, the first approach should be to get a good history from the patient, family, friends, and medical records. Finding out the timing of the onset of anisocoria occurred is very helpful, as a longstanding anisocoria is much less likely to represent a dangerous medical condition. Looking at an old picture of the patient can help show that the anisocoria may be chronic. Next, a thorough history of the medications the patient takes needs to be made, especially eye drops that have been put in the patient's eye. A history of a recent visit to an eye doctor is also very helpful since the anisocoria could be caused by eye drops given during the visit. A history of eye trauma and eye surgery must also be elicited from the patient, as these can be the cause of anisocoria. Other conditions to ask about include uveitis, iris coloboma, corectopia, neovascularization of the iris, or iridocorneal endothelial (ICE) syndrome.
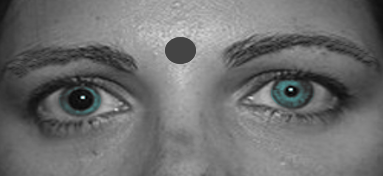
Once a thorough history has been taken, the abnormal pupil needs to be identified. To do this, both pupil sizes should be measured with the room lights on brightly and then again with the room lights dim. Having the room lights completely off may not be practical since the pupils need to be visible for measurement. To measure the pupil, a small ruler may be used. There are also near cards that have pupil sizes on them for comparison. While measuring the pupils, the patient should focus on a distant object. This is to avoid miosis (pupillary constriction) while the patient is accommodating at a near target. After the pupils have been measured, the practitioner should identify whether the anisocoria is greater in light or darker conditions.
Anisocoria greater in the light indicates the large pupil is the abnormal pupil due to poor pupillary constriction. Anisocoria greater in the dark indicates the small pupil to be abnormal due to poor pupillary dilation. A small amount of anisocoria that is equal in both light and dark conditions most likely represents physiologic anisocoria.
Other important aspects of the physical exam include assessing visual acuity at both distance and near. Worse near visual acuity in the eye with a larger pupil is more likely to indicate pharmacologic dilation from a cycloplegic medication. The swinging flashlight test should be performed to assess for a relative afferent pupillary defect.[7] Eyelid position should be observed, as ptosis in the affected pupil is associated with both a horner syndrome and third nerve palsy. A full neurological, cranial nerve exam should be performed, as deficits in other cranial nerves may localize a specific lesion.[8] Special attention should be paid to assessing extraocular motility, which tests cranial nerves III, IV, and VI.[9][10][11] Lastly, a careful slit lamp examination can uncover an underlying causative etiology for the anisocoria. While this may not be available to all medical providers, an attempt at looking at both eyes closely should be made.
Evaluation
If a third nerve palsy is causing anisocoria, imaging is recommended to rule out a compressive lesion, especially an aneurysm, which can be acutely fatal. An aneurysm can be most effectively imaged with a computed tomography angiogram (CTA) or a magnetic resonance angiogram (MRA) of the head.[12] If Horner syndrome is causing the anisocoria and a carotid artery dissection or aneurysm could be the cause, imaging is recommended. A CTA or MRA of the head and neck should be performed.[13]
Treatment / Management
The treatment of anisocoria depends on the underlying condition causing the condition. Most causes of anisocoria only require observation. A referral to a neuro-ophthalmologist, ophthalmologist, or neurologist may be warranted in cases that do not resolve. Acute onset anisocoria that is concerning for a compressive third nerve palsy or horner syndrome should be sent to the emergency department immediately for imaging.
Physiologic anisocoria and Adie tonic pupil simply require observation and proper documentation of the condition to prevent unnecessary medical workup in the future potentially. Anisocoria due to medication will resolve over time. Anisocoria due to trauma may remain permanent but also may improve over time. Surgical management is rarely warranted. Anisocoria due to uveitis, ICE syndrome, and neovascularization of the iris require treatment of the underlying condition.
Differential Diagnosis
The differential of conditions causing anisocoria may be divided into three sub-categories, depending upon whether the anisocoria increases in dim light, in bright light, or remains equal in both lighting conditions.
Causes of Anisocoria Greater in Dim Light
Horner Syndrome
Horner’s syndrome occurs as a result of a lesion along the oculo-sympathetic pathway. Clinical features include ipsilateral miosis, ptosis, anhidrosis, enophthalmos, and loss of ciliospinal reflex. Inverse ptosis (upside-down ptosis), a condition where the lower eyelid elevates due to underlying denervated tarsal muscle, may also be seen. It is worth noting that the enophthalmos in Horner syndrome is not a true enophthalmos. It results due to evident narrowing of vertical palpebral fissure height, producing an apparent sunken appearance of the globe.
Prior knowledge of the sympathetic pathway is important to localize the lesion and understand the rationale behind the clinical presentation of Horner syndrome.
The sympathetic pathway comprises a three–order neuronal chain. The first–order neuron arises from the posterolateral hypothalamus and synapses at the C8-T2 level in the intermediolateral column of the spinal cord, also called the ciliospinal center of Budge. The second-order neurons now travel across the apex of the lung and along the sympathetic chain, ultimately synapsing at the level of the superior cervical ganglion. The third-order neurons (postganglionic fibers) travel with the internal carotid artery (ICA) through the cavernous sinus and then along the abducens nerve. It then follows the first division of the trigeminal nerve as the nasociliary nerve and later as the long ciliary nerves to supply the dilator pupillae.
Anhidrosis is typically present in cases of central (1 order) or pre-ganglionic (2 order) lesions. Although the classical clinical features are sufficient to diagnose Horner syndrome, several pharmacological tests are available to confirm a case of suspected Horner syndrome, as summarised in Table 2.
|
Drug
|
Mechanism of Action
|
Response
|
Rationale
|
Localization
|
Remarks
|
|
Cocaine
(2 drops, 4% or 10%)
|
Noradrenaline reuptake inhibitor (released at nerve terminals)
|
Anisocoria > 1 mm after 45-60 mins, diagnostic of Horner’s syndrome on the miotic side
|
Horner pupil has negligible noradrenaline at the synaptic cleft.
|
No role in the localization of the lesion
|
Better than apraclonidine for children as the latter causes CNS/respiratory arrest
|
|
Apraclonidine (0.5% or 2%)
|
α-2 adrenergic agonist + weak α-1 agonist activity on iris dilator
|
Horner pupil dilates, and the anisocoria decreases. This is known as the “reversal of anisocoria.”
|
Only the Horner’s pupil will dilate in response to weak α-1 due to denervation hypersensitivity
|
Theoretically more sensitive for the post-ganglionic lesions. No definitive role
|
Not useful for acute-onset Horner syndrome as the denervation hypersensitivity takes 2-5 days to set in
|
|
Phenylephrine (10% or 2.5%)
|
Direct sympathomimetic activity
|
Horner pupil dilates
|
Direct action of the drug
|
No role in localizing sympatholytic lesion
|
It helps in ruling out mechanical causes
|
|
Hydroxyamphetamine (1%)
|
Presynaptic norepinephrine release from intact post-ganglionic neuron
|
Horner pupil with post-ganglionic lesion will not dilate. Pupils dilate if 1/2 order neuron dysfunction is present.
|
Presynaptic norepinephrine release will only occur if the post-ganglionic pathway is intact.
|
Post-ganglionic location if the Horner’s pupil does not dilate
|
Cocaine interferes with the efficacy of hydroxy-amphetamine, and thus, the two tests must be used at least 3 days apart.
|
Anisocoria due to Horner syndrome associated with pain should be treated as an emergency warranting immediate recognition. The most important cause of a painful Horner’s syndrome is ICA dissection.[14]
Children with anisocoria must be evaluated for birth trauma. It is the most common cause of congenital Horner’s syndrome. If no evidence of trauma is found, a dedicated work-up to rule out neuroblastoma is mandated in children. Appropriate imaging, including Magnetic Resonance Imaging (MRI) head, neck, chest, and abdomen, should be carried out for timely detection and appropriate management.
Cholinergic Medications
Cholinergic medications can cause miosis of the pupil through activation of the sphincter pupillae. The most common eye drop is pilocarpine, which has historically been used to treat glaucoma.
Posterior Synechiae
If posterior synechiae (abnormal connections between the iris and the lens) develop, the pupil may not be able to dilate fully. This can be caused by uveitis, angle-closure glaucoma, or other inflammatory conditions. The best way to evaluate for posterior synechiae is with a slit lamp examination. In this case, the underlying condition needs to be treated.
Causes of Anisocoria Greater in Bright Light
Third Nerve Palsy
The parasympathetic fibers run along the periphery of the third nerve. Thus, compressive lesions of the third nerve would affect the parasympathetic fibers. This inhibits the signal to the sphincter pupillae, causing unopposed dilation of the pupil on the affected side. A third nerve palsy can be differentiated from other causes if the oculomotor component is affected. There would be significant ptosis of the affected upper eyelid due to inhibition to the levator palpebrae superioris. The eye would also be abducted and depressed, also known as "down and out." This is due to the unopposed action of the lateral rectus and superior oblique, which are the two extraocular muscles not innervated by the third cranial nerve. [12] A very concerning compressive lesion would be an aneurysm, which can be acutely fatal.
Migraine Headache
A migraine headache can cause anisocoria associated with pain. The pupil will typically be dilated, and the dilation often resolves after the headache has subsided.
Cycloplegic Medications
Cycloplegic medications cause paralysis of the sphincter pupillae, which in turn causes unopposed dilation. This pupil will, at most, minimally constrict with light and, much of the time, will not react at all due to paralysis. Pilocarpine will not be effective in causing this pupil to constrict. Cycloplegic eye drops include cyclopentolate, atropine, and tropicamide. The same effect can be achieved if a patient touches an anticholinergic medication and then touches the eye. Getting a history of cycloplegic medication use is the best way to make this diagnosis.
Sympapathomymetics
Eye drops that cause activation of the dilator pupillae can cause mydriasis of the pupil. There still should be some reactivity of the pupil. The dilation is not as great as with cycloplegic medications.
Adie Tonic Pupil
In this condition, the larger pupil fails to constrict to the extent of the other pupil. However, when the eye accommodates, the pupil has greater constriction. This cause of anisocoria can be diagnosed with dilute pilocarpine, which causes significant constriction of the larger pupil. Other causes of a dilated pupil typically do not respond to dilute pilocarpine, helping confirm the diagnosis of Adie tonic pupil.[15]
Traumatic Mydriasis
Damage to the pupillary sphincter due to trauma or intraocular surgery may leave the pupil dilated and potentially with an irregular shape. The pupil may then be unable to constrict. The best way to diagnosis traumatic mydriasis is to get a complete history of ocular trauma and eye surgeries and then perform a slit lamp exam. Mydriasis due to trauma may improve over time or remain permanent. An irregular pupil after intraocular surgery has a higher likelihood of remaining permanent.
Causes of Anisocoria that is Equal in Bright and Dim Light Conditions
Physiological Anisocoria
Physiologic anisocoria is usually defined as a pupillary inequality of 0.4 mm, seldom greater than 0.8 mm, not due to a secondary cause. If the anisocoria is physiologic, the difference in pupil sizes should remain equal in dim and bright lights. This also should be something that patient has had for a long time and has not acutely changed. The difference in pupil size in physiologic anisocoria remains stable over time and is not a concern for an underlying medical condition.
Prognosis
The prognosis of anisocoria depends entirely on the causative factor. There is no difference in mortality from most causes anisocoria compared to the general population, with the exception of two causative conditions.
Ruptured aneurysms causing a third nerve palsy have a very poor prognosis. Only fifty percent of patients survive a ruptured aneurysm after six months.[16] Horner syndrome can cause a miotic pupil, with the concerning conditions being a carotid artery dissection, which causes 2.5% of strokes, and a Pancoast lung tumor. [17][18]
Anisocoria itself generally does not affect ocular health, and visual acuity usually is minimally affected. Visual prognosis is mostly based on the causative condition.
Complications
Anisocoria itself is unlikely to cause significant complications, although some do exist. A larger pupil may cause light sensitivity and visual aberrations. A smaller pupil may cause worsened visualization through a cataract, difficulty viewing the fundus during the posterior exam, or difficulty in cataract surgery. The main complication of anisocoria is not the difference in pupil size but the complications of the underlying condition itself.
Deterrence and Patient Education
Anisocoria is a clinical sign, and patients may not be able to identify this. However, patients should be educated that if they develop a sudden severe headache, blood in sputum, or a sudden blurring of vision with an associated anisocoria, they should be seen by a medical specialist as soon as possible. These signs could indicate a serious medical issue and need to be evaluated.
Pearls and Other Issues
Anisocoria has a variety of causes, many of which are benign. The two entities causing anisocoria that are the most significant to the clinician and require prompt and accurate diagnosis are TNP and Horner syndrome. TNP is potentially life-threatening if caused by an aneurysm, and Horner syndrome can indicate carotid dissection, among many other possibilities. A comprehensive radiological workup may be required in these cases. The final point is that an accurate examination is essential in evaluating anisocoria; this can only be done in a room where the light can be turned on and then dimmed, with the patient focusing on a distant object.
Enhancing Healthcare Team Outcomes
All types of medical providers may come across a patient with uneven pupils. It is important to know that while the condition can be benign, there are many serious pathologies associated with this eye finding. It is important to communicate this finding with other healthcare providers so that the appropriate intervention can take place.
There are multiple pathways involved in determining pupillary size and reactivity. Pupillary size may be influenced by systemic drug use or topical ophthalmics. Anisocoria also may be present in a cluster headache with lacrimation and rhinorrhea. Other rare forms of a headache also may invoke anisocoria. Additionally, some autonomic ganglion pathology may manifest as anisocoria. Also, there are reports of a variety of unusual causes involving a number of medicines as well as surgical procedures that usually occur on the face.[19] Lastly, iatrogenic trauma from ophthalmic surgery can cause an irregular pupil, and an ophthalmic surgical history should be obtained whenever assessing anisocoria.
A referral to a neurologist and/or ophthalmologist is highly recommended in most cases of anisocoria in which the underlying etiology has not been identified. In cases of acute anisocoria with concern for a compressive third nerve palsy or Horner syndrome, the patient should be sent to the emergency department immediately for imaging.[6] [Level 5] Identification of an aneurysm or carotid dissection early from anisocoria can save a patient's life.