[1]
Alpert JS, Thygesen K, Antman E, Bassand JP. Myocardial infarction redefined--a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. Journal of the American College of Cardiology. 2000 Sep:36(3):959-69
[PubMed PMID: 10987628]
Level 3 (low-level) evidence
[2]
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, White HD, ESC Scientific Document Group. Fourth universal definition of myocardial infarction (2018). European heart journal. 2019 Jan 14:40(3):237-269. doi: 10.1093/eurheartj/ehy462. Epub
[PubMed PMID: 30165617]
[3]
Wilson PW. Established risk factors and coronary artery disease: the Framingham Study. American journal of hypertension. 1994 Jul:7(7 Pt 2):7S-12S
[PubMed PMID: 7946184]
[4]
Canto JG, Kiefe CI, Rogers WJ, Peterson ED, Frederick PD, French WJ, Gibson CM, Pollack CV Jr, Ornato JP, Zalenski RJ, Penney J, Tiefenbrunn AJ, Greenland P, NRMI Investigators. Number of coronary heart disease risk factors and mortality in patients with first myocardial infarction. JAMA. 2011 Nov 16:306(19):2120-7. doi: 10.1001/jama.2011.1654. Epub
[PubMed PMID: 22089719]
[5]
Hartikainen TS, Sörensen NA, Haller PM, Goßling A, Lehmacher J, Zeller T, Blankenberg S, Westermann D, Neumann JT. Clinical application of the 4th Universal Definition of Myocardial Infarction. European heart journal. 2020 Jun 14:41(23):2209-2216. doi: 10.1093/eurheartj/ehaa035. Epub
[PubMed PMID: 32077925]
[6]
Writing Group Members, Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Després JP, Fullerton HJ, Howard VJ, Huffman MD, Isasi CR, Jiménez MC, Judd SE, Kissela BM, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Magid DJ, McGuire DK, Mohler ER 3rd, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Rosamond W, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Woo D, Yeh RW, Turner MB, American Heart Association Statistics Committee, Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association. Circulation. 2016 Jan 26:133(4):e38-360. doi: 10.1161/CIR.0000000000000350. Epub 2015 Dec 16
[PubMed PMID: 26673558]
[7]
Kolodgie FD, Burke AP, Farb A, Gold HK, Yuan J, Narula J, Finn AV, Virmani R. The thin-cap fibroatheroma: a type of vulnerable plaque: the major precursor lesion to acute coronary syndromes. Current opinion in cardiology. 2001 Sep:16(5):285-92
[PubMed PMID: 11584167]
Level 3 (low-level) evidence
[8]
Scharf RE. Platelet Signaling in Primary Haemostasis and Arterial Thrombus Formation: Part 1. Hamostaseologie. 2018 Nov:38(4):203-210. doi: 10.1055/s-0038-1675144. Epub 2018 Oct 23
[PubMed PMID: 30352470]
[9]
Reimer KA, Jennings RB. The "wavefront phenomenon" of myocardial ischemic cell death. II. Transmural progression of necrosis within the framework of ischemic bed size (myocardium at risk) and collateral flow. Laboratory investigation; a journal of technical methods and pathology. 1979 Jun:40(6):633-44
[PubMed PMID: 449273]
[10]
Amsterdam EA, Wenger NK, Brindis RG, Casey DE Jr, Ganiats TG, Holmes DR Jr, Jaffe AS, Jneid H, Kelly RF, Kontos MC, Levine GN, Liebson PR, Mukherjee D, Peterson ED, Sabatine MS, Smalling RW, Zieman SJ. 2014 AHA/ACC Guideline for the Management of Patients with Non-ST-Elevation Acute Coronary Syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Journal of the American College of Cardiology. 2014 Dec 23:64(24):e139-e228. doi: 10.1016/j.jacc.2014.09.017. Epub 2014 Sep 23
[PubMed PMID: 25260718]
Level 3 (low-level) evidence
[11]
Torpy JM, Burke AE, Glass RM. JAMA patient page. Coronary heart disease risk factors. JAMA. 2009 Dec 2:302(21):2388. doi: 10.1001/jama.302.21.2388. Epub
[PubMed PMID: 19952328]
[12]
McCord J, Jneid H, Hollander JE, de Lemos JA, Cercek B, Hsue P, Gibler WB, Ohman EM, Drew B, Philippides G, Newby LK, American Heart Association Acute Cardiac Care Committee of the Council on Clinical Cardiology. Management of cocaine-associated chest pain and myocardial infarction: a scientific statement from the American Heart Association Acute Cardiac Care Committee of the Council on Clinical Cardiology. Circulation. 2008 Apr 8:117(14):1897-907. doi: 10.1161/CIRCULATIONAHA.107.188950. Epub 2008 Mar 17
[PubMed PMID: 18347214]
[13]
Akbar H, Kahloon A, Kahloon R. Diagnostic Challenge in a Symptomatic Patient of Arteria Lusoria with Retro-esophageal Right Subclavian Artery and Absent Brachiocephalic Trunk. Cureus. 2020 Feb 18:12(2):e7029. doi: 10.7759/cureus.7029. Epub 2020 Feb 18
[PubMed PMID: 32117665]
[14]
Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, Joint ESC/ACCF/AHA/WHF Task Force for the Universal Definition of Myocardial Infarction, Katus HA, Lindahl B, Morrow DA, Clemmensen PM, Johanson P, Hod H, Underwood R, Bax JJ, Bonow RO, Pinto F, Gibbons RJ, Fox KA, Atar D, Newby LK, Galvani M, Hamm CW, Uretsky BF, Steg PG, Wijns W, Bassand JP, Menasché P, Ravkilde J, Ohman EM, Antman EM, Wallentin LC, Armstrong PW, Simoons ML, Januzzi JL, Nieminen MS, Gheorghiade M, Filippatos G, Luepker RV, Fortmann SP, Rosamond WD, Levy D, Wood D, Smith SC, Hu D, Lopez-Sendon JL, Robertson RM, Weaver D, Tendera M, Bove AA, Parkhomenko AN, Vasilieva EJ, Mendis S. Third universal definition of myocardial infarction. Circulation. 2012 Oct 16:126(16):2020-35. doi: 10.1161/CIR.0b013e31826e1058. Epub 2012 Aug 24
[PubMed PMID: 22923432]
[15]
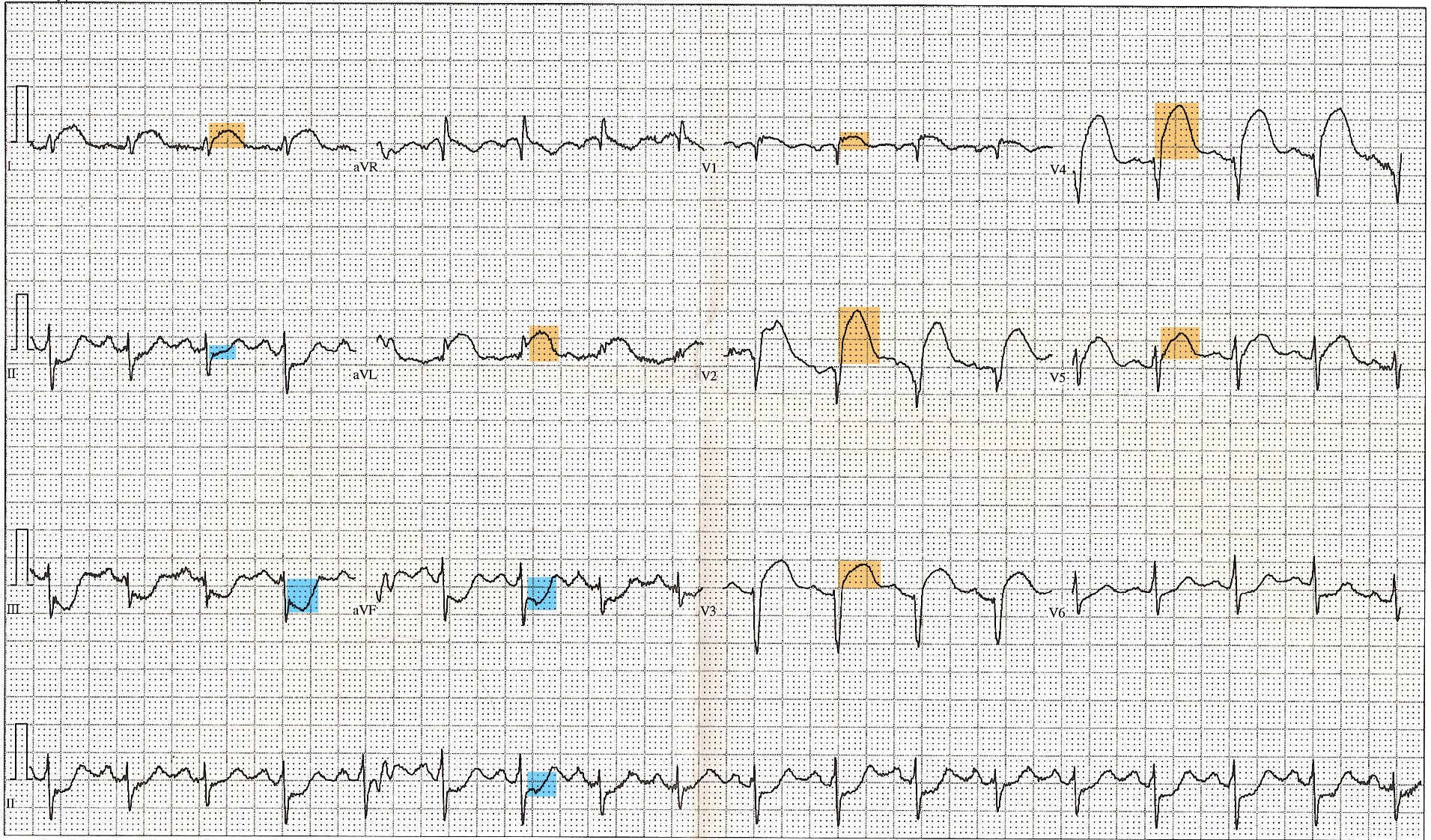
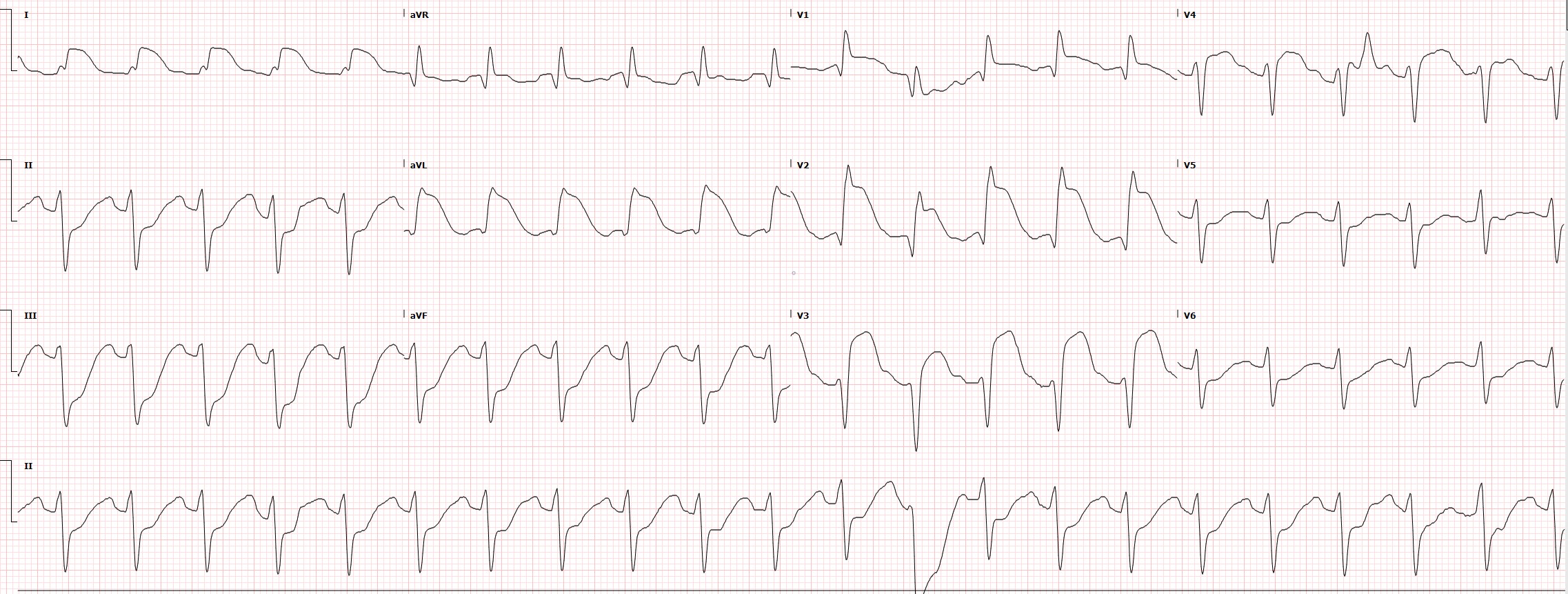
Sgarbossa EB, Pinski SL, Barbagelata A, Underwood DA, Gates KB, Topol EJ, Califf RM, Wagner GS. Electrocardiographic diagnosis of evolving acute myocardial infarction in the presence of left bundle-branch block. GUSTO-1 (Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries) Investigators. The New England journal of medicine. 1996 Feb 22:334(8):481-7
[PubMed PMID: 8559200]
[16]
Smith SW, Dodd KW, Henry TD, Dvorak DM, Pearce LA. Diagnosis of ST-elevation myocardial infarction in the presence of left bundle branch block with the ST-elevation to S-wave ratio in a modified Sgarbossa rule. Annals of emergency medicine. 2012 Dec:60(6):766-76. doi: 10.1016/j.annemergmed.2012.07.119. Epub 2012 Aug 31
[PubMed PMID: 22939607]
[17]
Stub D, Smith K, Bernard S, Nehme Z, Stephenson M, Bray JE, Cameron P, Barger B, Ellims AH, Taylor AJ, Meredith IT, Kaye DM, AVOID Investigators. Air Versus Oxygen in ST-Segment-Elevation Myocardial Infarction. Circulation. 2015 Jun 16:131(24):2143-50. doi: 10.1161/CIRCULATIONAHA.114.014494. Epub 2015 May 22
[PubMed PMID: 26002889]
[18]
Hofmann R, James SK, Jernberg T, Lindahl B, Erlinge D, Witt N, Arefalk G, Frick M, Alfredsson J, Nilsson L, Ravn-Fischer A, Omerovic E, Kellerth T, Sparv D, Ekelund U, Linder R, Ekström M, Lauermann J, Haaga U, Pernow J, Östlund O, Herlitz J, Svensson L, DETO2X–SWEDEHEART Investigators. Oxygen Therapy in Suspected Acute Myocardial Infarction. The New England journal of medicine. 2017 Sep 28:377(13):1240-1249. doi: 10.1056/NEJMoa1706222. Epub 2017 Aug 28
[PubMed PMID: 28844200]
[19]
O'Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Ou N, Radford MJ, Tamis-Holland JE, Tommaso CL, Tracy CM, Woo YJ, Zhao DX, Anderson JL, Jacobs AK, Halperin JL, Albert NM, Brindis RG, Creager MA, DeMets D, Guyton RA, Hochman JS, Kovacs RJ, Kushner FG, Ohman EM, Stevenson WG, Yancy CW, American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013 Jan 29:127(4):e362-425. doi: 10.1161/CIR.0b013e3182742cf6. Epub 2012 Dec 17
[PubMed PMID: 23247304]
Level 3 (low-level) evidence
[20]
Meine TJ, Roe MT, Chen AY, Patel MR, Washam JB, Ohman EM, Peacock WF, Pollack CV Jr, Gibler WB, Peterson ED, CRUSADE Investigators. Association of intravenous morphine use and outcomes in acute coronary syndromes: results from the CRUSADE Quality Improvement Initiative. American heart journal. 2005 Jun:149(6):1043-9
[PubMed PMID: 15976786]
Level 2 (mid-level) evidence
[21]
Wiviott SD, Braunwald E, McCabe CH, Montalescot G, Ruzyllo W, Gottlieb S, Neumann FJ, Ardissino D, De Servi S, Murphy SA, Riesmeyer J, Weerakkody G, Gibson CM, Antman EM, TRITON-TIMI 38 Investigators. Prasugrel versus clopidogrel in patients with acute coronary syndromes. The New England journal of medicine. 2007 Nov 15:357(20):2001-15
[PubMed PMID: 17982182]
[22]
Wallentin L, Becker RC, Budaj A, Cannon CP, Emanuelsson H, Held C, Horrow J, Husted S, James S, Katus H, Mahaffey KW, Scirica BM, Skene A, Steg PG, Storey RF, Harrington RA, PLATO Investigators, Freij A, Thorsén M. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. The New England journal of medicine. 2009 Sep 10:361(11):1045-57. doi: 10.1056/NEJMoa0904327. Epub 2009 Aug 30
[PubMed PMID: 19717846]
[23]
Sabatine MS, Cannon CP, Gibson CM, López-Sendón JL, Montalescot G, Theroux P, Claeys MJ, Cools F, Hill KA, Skene AM, McCabe CH, Braunwald E, CLARITY-TIMI 28 Investigators. Addition of clopidogrel to aspirin and fibrinolytic therapy for myocardial infarction with ST-segment elevation. The New England journal of medicine. 2005 Mar 24:352(12):1179-89
[PubMed PMID: 15758000]
[25]
McManus DD, Gore J, Yarzebski J, Spencer F, Lessard D, Goldberg RJ. Recent trends in the incidence, treatment, and outcomes of patients with STEMI and NSTEMI. The American journal of medicine. 2011 Jan:124(1):40-7. doi: 10.1016/j.amjmed.2010.07.023. Epub
[PubMed PMID: 21187184]
[26]
Jernberg T, Johanson P, Held C, Svennblad B, Lindbäck J, Wallentin L, SWEDEHEART/RIKS-HIA. Association between adoption of evidence-based treatment and survival for patients with ST-elevation myocardial infarction. JAMA. 2011 Apr 27:305(16):1677-84. doi: 10.1001/jama.2011.522. Epub
[PubMed PMID: 21521849]
[27]
Rosamond WD, Chambless LE, Heiss G, Mosley TH, Coresh J, Whitsel E, Wagenknecht L, Ni H, Folsom AR. Twenty-two-year trends in incidence of myocardial infarction, coronary heart disease mortality, and case fatality in 4 US communities, 1987-2008. Circulation. 2012 Apr 17:125(15):1848-57. doi: 10.1161/CIRCULATIONAHA.111.047480. Epub 2012 Mar 15
[PubMed PMID: 22420957]
Level 3 (low-level) evidence
[28]
Morrow DA, Antman EM, Charlesworth A, Cairns R, Murphy SA, de Lemos JA, Giugliano RP, McCabe CH, Braunwald E. TIMI risk score for ST-elevation myocardial infarction: A convenient, bedside, clinical score for risk assessment at presentation: An intravenous nPA for treatment of infarcting myocardium early II trial substudy. Circulation. 2000 Oct 24:102(17):2031-7
[PubMed PMID: 11044416]
[29]
Batts KP, Ackermann DM, Edwards WD. Postinfarction rupture of the left ventricular free wall: clinicopathologic correlates in 100 consecutive autopsy cases. Human pathology. 1990 May:21(5):530-5
[PubMed PMID: 2338333]
Level 3 (low-level) evidence
[30]
Yip HK, Wu CJ, Chang HW, Wang CP, Cheng CI, Chua S, Chen MC. Cardiac rupture complicating acute myocardial infarction in the direct percutaneous coronary intervention reperfusion era. Chest. 2003 Aug:124(2):565-71
[PubMed PMID: 12907544]
[31]
Figueras J, Alcalde O, Barrabés JA, Serra V, Alguersuari J, Cortadellas J, Lidón RM. Changes in hospital mortality rates in 425 patients with acute ST-elevation myocardial infarction and cardiac rupture over a 30-year period. Circulation. 2008 Dec 16:118(25):2783-9. doi: 10.1161/CIRCULATIONAHA.108.776690. Epub 2008 Dec 8
[PubMed PMID: 19064683]
[32]
Crenshaw BS, Granger CB, Birnbaum Y, Pieper KS, Morris DC, Kleiman NS, Vahanian A, Califf RM, Topol EJ. Risk factors, angiographic patterns, and outcomes in patients with ventricular septal defect complicating acute myocardial infarction. GUSTO-I (Global Utilization of Streptokinase and TPA for Occluded Coronary Arteries) Trial Investigators. Circulation. 2000 Jan 4-11:101(1):27-32
[PubMed PMID: 10618300]
[33]
Tcheng JE, Jackman JD Jr, Nelson CL, Gardner LH, Smith LR, Rankin JS, Califf RM, Stack RS. Outcome of patients sustaining acute ischemic mitral regurgitation during myocardial infarction. Annals of internal medicine. 1992 Jul 1:117(1):18-24
[PubMed PMID: 1596043]
[34]
Krumholz HM, Herrin J, Miller LE, Drye EE, Ling SM, Han LF, Rapp MT, Bradley EH, Nallamothu BK, Nsa W, Bratzler DW, Curtis JP. Improvements in door-to-balloon time in the United States, 2005 to 2010. Circulation. 2011 Aug 30:124(9):1038-45. doi: 10.1161/CIRCULATIONAHA.111.044107. Epub 2011 Aug 22
[PubMed PMID: 21859971]
[35]
Bradley EH, Nallamothu BK, Herrin J, Ting HH, Stern AF, Nembhard IM, Yuan CT, Green JC, Kline-Rogers E, Wang Y, Curtis JP, Webster TR, Masoudi FA, Fonarow GC, Brush JE Jr, Krumholz HM. National efforts to improve door-to-balloon time results from the Door-to-Balloon Alliance. Journal of the American College of Cardiology. 2009 Dec 15:54(25):2423-9. doi: 10.1016/j.jacc.2009.11.003. Epub
[PubMed PMID: 20082933]