Introduction
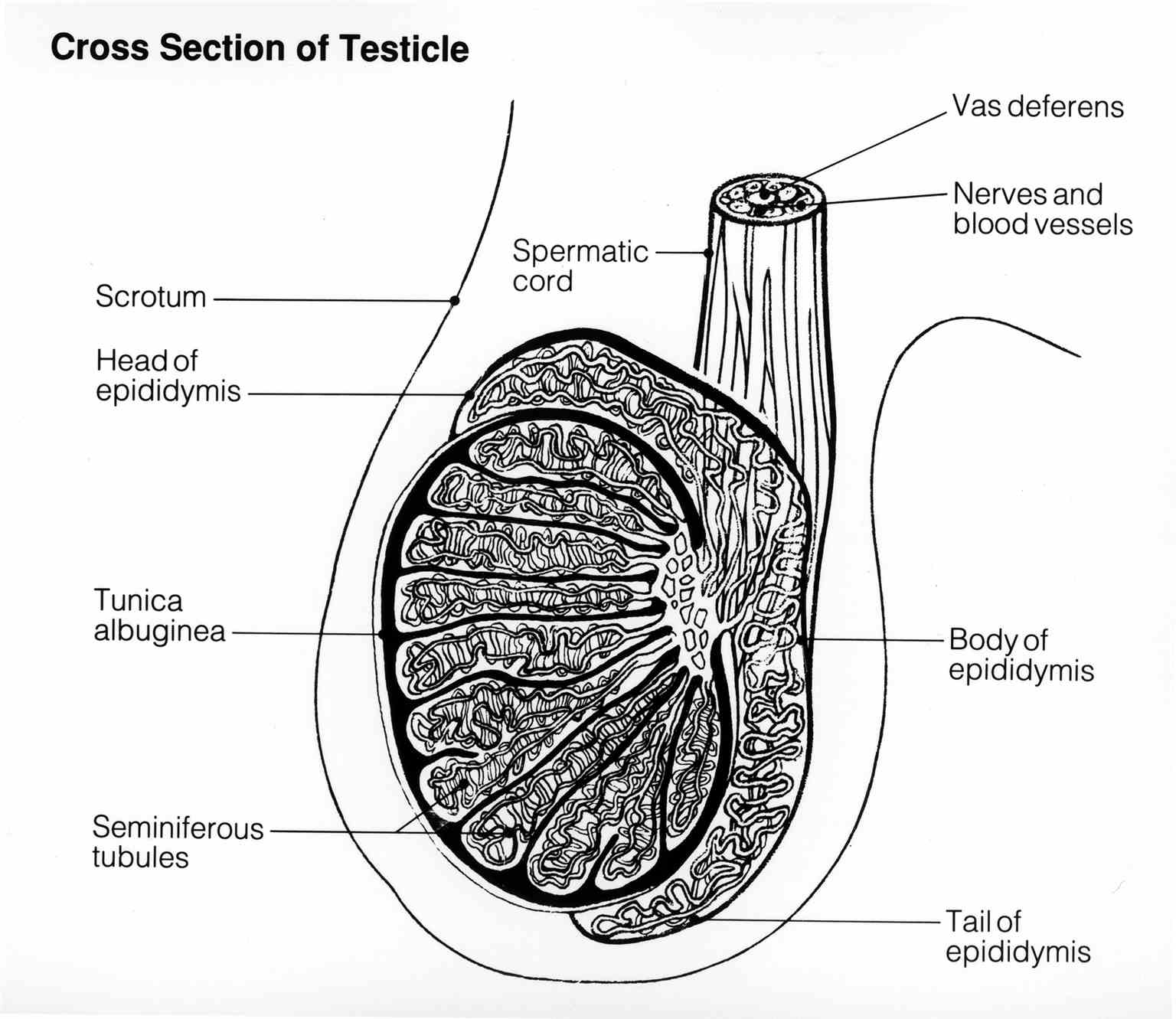
The testes are male sex glands that have both an endocrine and exocrine function. The testes are oval-shaped reproductive structures that are found in the scrotum and separated by the scrotal septum. The shape of the testes is bean-shaped and measures three cm by five cm in length and 2 cm to 3 cm in width. When palpated through the scrotum, the testes are smooth and soft. The spermatic cord suspends the superior aspect of the testes. At the inferior end, the testes are attached to the scrotum by the scrotal ligament which is a remnant of the gubernaculum. In general, the left testis is affixed slightly lower than the right testis.[1][2]
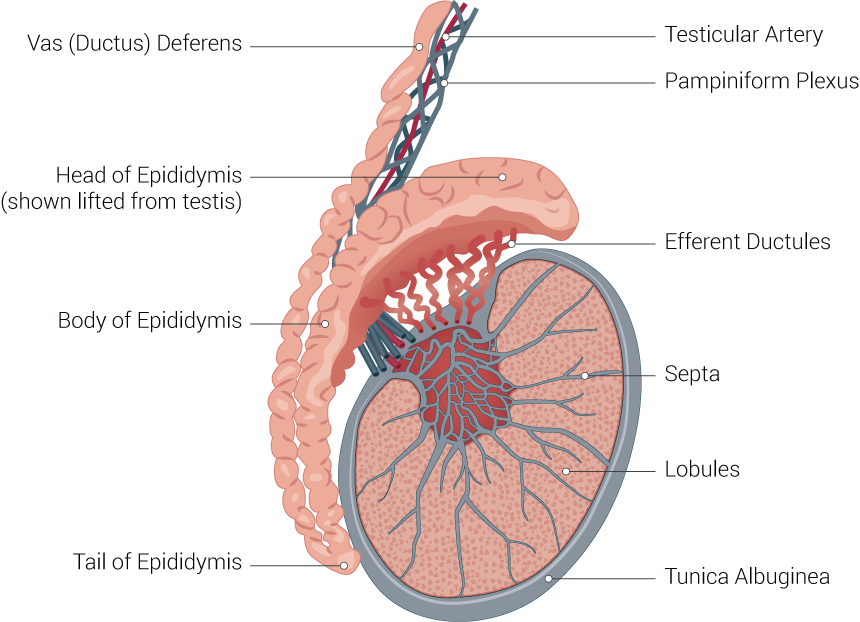
The double-layered tunica vaginalis envelop the testes except at the posterior and superior borders where the epididymis and spermatic cord are attached. The visceral or inner layer of the tunica vaginalis is close to the epididymis, testes and vas deferens. On the posterior lateral surface of the testes, there is a small space between the testes and body of the epididymis which is known as the sinus of the epididymis. Deep to the tunica vaginalis is located the tunica albuginea, which is a durable fibrous covering of the testes.
The epididymis is a small curved shaped elongated structure which is highly convoluted and tightly compressed. When open in a straight line, it is estimated that its length is about 20 feet. The epididymis is found on the posterior border of the testis and consists of three parts which include the head (caput), body (corpora), and tail (Cauda). The head of the epididymis lies at the upper pole of the testes and receive seminal fluid from the ducts of the testis. It then permits passage of sperm into the distal portion of the epididymis. Because of its length, the epididymal ducts have ample space for storage and maturation of sperm.