Introduction
Cannon A waves are large-amplitude waves seen in the jugular veins during a physical exam. They are caused by simultaneous contraction of atria and ventricle leading to exaggerated right atrial pressure. Usually, Cannon A waves are irregular and intermittent. They are seen in patients with cardiac conduction defects or certain cardiac dysrhythmias. Cannon A waves can also be seen on the EKG.[1][2][3][2]
Etiology
Cannon A waves are related to rhythm disturbances causing changes in the normal cardiac blood flow causing a large pressure vein in the jugular vein. Different dysrhythmias may cause cannon A waves. Heart block may lead to cannon A waves, in particular, third-degree (complete) heart block. It may be seen with ventricular tachycardia (VT) as a result of the underlying atrioventricular (AV) dissociation. Another cause is Pacemaker syndrome without proper synchronization of atria and ventricles. [4]
Cannon A waves need to be distinguished from giant A waves that occur in right heart structural changes such as tricuspid valvulopathies, right ventricular hypertrophy, and pulmonary hypertension. To the observer of the jugular, venous-pressure giant A waves and Cannon A waves may appear similar. From physical exams alone it might be difficult to differentiate between them.
Epidemiology
Jugular vein pulsation (JVP) provides clinically meaningful information about the central venous pressure (CVP). JVP is an important and reproducible tool to diagnose various cardiac conditions which can cause a change in CVP. Canon A wave can be easily missed without close attention during bedside examination especially due to declining physical exam skills in contemporary clinical practice. Recent literature does not describe the frequency of cannon A waves in rhythm disturbances.
Pathophysiology
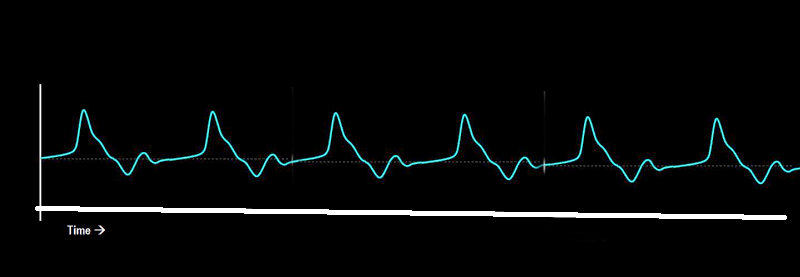
The normal function of the heart is to create forward blood flow. During each cardiac cycle, blood is pushed from the atria to the ventricles passing through the atrioventricular valves. Central venous pressure is measured in the right atrium. The bedside clinician can directly assess the jugular venous pulse by observing the patients neck. When obtaining a central or jugular venous pressure curve, its course can be described as 3 positive and 2 negative deflections. [5][6]The 3 positive deflections are:
- Atrial contraction (A wave)
- Ventricular contraction (C wave)
- Venous passive filling of the right atrium (V wave)
The negative deflections are:
- Atrial relaxation (X wave)
- Emptying of the right atrium (Y wave)
A proper heart function requires a synchronized action of the myocardium. When the cardiac rhythm is disturbed, the heart cannot provide proper blood flow. Cannon A waves are an example of this. Electrical disturbances cause mechanical problems causing atrial contraction to occur when the tricuspid valve is closed. The reflection of the pressure wave travels up the venous system and can be examined in the jugular vein as exaggerated A wave pulsation.
A Wave in JVP is an expression of normal atrial contraction. In opposition to Canon A waves, missing A waves might indicate atrial standstill as seen in atrial fibrillation.
History and Physical
Patients may complain of pulsations in the neck and abdomen as the pulse wave travels back into the venous system. Other symptoms such as a headache, cough, and jaw pain can occur. Ask the patient for polyuria since increased atrial stress leads to higher BNP levels which in return will cause polyuria. Since Cannon A waves are associated with higher right atrial pressures. Erlebacher et al. describe that this may result in baroreceptor mediated systemic hypotension.
The inspection of jugular venous pulsation should be in conjunction with auscultation of the heart. Remember the relation of the venous pressure curve to the heart sounds. The A wave is followed closely by the S1 heart sound as the atrial contraction is followed by the closure of the atrioventricular valves.
The characteristic appearance of the neck vein pulsation is called frog sign according to Contreras-Valdes et al.
According to Ranjith et al., it is helpful to differentiate between regular and irregular Cannon waves since regular Cannon A waves might be caused by junctional rhythm or supraventricular tachycardia. Whereas, atrioventricular dissociation, ectopic atrial beats can result in irregular A waves.
Evaluation
Patients complaining of symptoms that can be related to cannon A waves or direct physical exam positive for Cannon A waves should undergo further testing. To identify the cause of Cannon A waves and to distinguish from giant A waves an ECG and echocardiography should be performed. The ECG is helpful to look for rhythm disturbances. If P waves fall within QT interval should prompt examining for Cannon A waves. For assessing the structural changes, an ultrasound examination of the heart should be performed with attention to the right heart looking for hypertrophy, tricuspid pathology, and pulmonary hypertension.[7][1][8]
Treatment / Management
Treatment of Cannon A waves depends on the underlying pathology.
Differential Diagnosis
When inspecting the patient's neck, a variety of pulsation phenomena might be seen. The important differentials of elevated JVP are fluid overload due to variety of causes, superior vena cava obstruction, or an increase in intrathoracic pressure. The first step is to differentiate between arterial and venous pulsations by location and strength on palpation. There are higher pressures existent in the arterial than in the venous circulation. Right Internal jugular vein is usually preferred over the left as it is in direct line with superior vena cava.
The venous pressure curve can be altered in different ways and Cannon A waves may be mistaken. For example, giant C and V waves can occur in tricuspid regurgitation. This is called Lancisi's sign. Jugular vein distension can result from a pulmonary embolism as part of Beck's Triad. Elevated JVP without venous pulsations should raise the suspicion of superior vena cava obstruction. This illustrates the importance of venous pressure as a window to the right heart.
Consultations
Cannon A waves relate to cardiologic pathology. Since then the patient may be referred to cardiologic consultation.
Pearls and Other Issues
- The physical exam is key as it allows for fast and direct detection of cardiac pathologies.
- The central venous pressure curve is important for the identification of right heart abnormalities.
- Be confident with the normal jugular venous pressure curve and pathologic changes it may show.
- When observing pulsations of the neck, remember Cannon A waves as a possible cause and perform an ECG and ECHO as additional tests.
Enhancing Healthcare Team Outcomes
Clinicians (nurse practitioners, physicians, physician assistants) may notice a pulsating sensation in the neck. One cause for this might be a phenomenon called Cannon A wave. It is an exaggerated pulse wave. In normal healthy people, when the atria contract blood is pushed into the ventricles. When the cardiac action is not well synchronized as might be the case in cardiac rhythm abnormalities, blood pushes against the closed tricuspid valve and create a large reverse pulsation into the venous system. This pressure wave might be felt in the neck, jaw, and abdomen. A feeling of pulsation should prompt further investigation. When Cannon A waves are found, further investigations may be needed to identify the reason why the heart rhythm is not well synchronized. Cardiology consultation may be necessary.