Continuing Education Activity
Multiple sclerosis is a chronic autoimmune disease affecting the central nervous system and is characterized by inflammation, demyelination, gliosis, and neuronal loss. This condition manifests with a wide range of neurological symptoms, such as vision impairment, numbness and tingling, focal weakness, bladder and bowel dysfunction, and cognitive impairment. Multiple sclerosis has various disease courses, including relapsing-remitting, primary progressive, and secondary progressive. Early diagnosis, typically based on episodes separated in time and space, facilitates the prompt initiation of disease-modifying therapy aimed at reducing relapses and long-term disability, which is crucial for accurately diagnosing multiple sclerosis.
Treatment goals include decreasing relapses and magnetic resonance imaging activity while minimizing permanent disability and addressing various patient concerns such as bladder and bowel dysfunction, depression, cognitive impairment, fatigue, sexual dysfunction, sleep disturbances, and vertigo. Effective management of multiple sclerosis requires an interdisciplinary approach and various treatment options, including disease-modifying therapies such as glatiramer acetate, dimethyl fumarate, fingolimod, interferon-beta preparations, natalizumab, and mitoxantrone. This activity emphasizes the crucial role of interprofessional healthcare providers in facilitating early intervention for optimal patient outcomes due to the disease's impact on multiple systems and reduced life expectancy.
Objectives:
Identify early signs and symptoms of multiple sclerosis across various neurological domains.
Screen patients at risk for multiple sclerosis or presenting with suggestive symptoms using appropriate diagnostic tests such as magnetic resonance imaging, evoked potentials, and cerebrospinal fluid analysis.
Select appropriate symptomatic treatments for multiple sclerosis–related symptoms, such as spasticity, fatigue, pain, and bladder dysfunction.
Collaborate with other healthcare providers to address comorbidities, such as depression, cognitive impairment, and cardiovascular risk factors, in multiple sclerosis patients.
Introduction
Multiple sclerosis is a chronic autoimmune disease affecting the central nervous system (CNS) and is characterized by inflammation, demyelination, gliosis, and neuronal loss.[1] This condition manifests with a wide range of neurological symptoms, such as vision impairment, numbness and tingling, focal weakness, bladder and bowel dysfunction, and cognitive impairment.
Pathologically, perivascular lymphocytic infiltrate and macrophages lead to the degradation of myelin sheaths surrounding neurons, causing symptoms that vary depending on lesion location. Clinical symptoms characterized by acute relapses typically appear first in young adults, followed by a gradually progressive course leading to permanent disability within 10 to 15 years.[2]
Multiple sclerosis presents various disease courses and is classified into 7 categories, as outlined below.
- Relapsing-remitting (RR): This initial onset is observed in 70% to 80% of multiple sclerosis patients and is characterized by the below-mentioned neurological presentation.
- New or recurrent neurological symptoms that are consistent with multiple sclerosis
- Symptoms lasting 24 to 48 hours
- Symptoms developing over days to weeks
- Primary progressive (PP): This course presents in 15% to 20% of patients and shows a gradual deterioration from onset without relapses.
- Secondary progressive (SP): Following an initial relapsing-remitting course, this course is marked by a more gradual neurological decline. Superimposed relapses can occur but are not mandatory.
- Progressive-relapsing (PR): This course involves gradual deterioration with superimposed relapses and is seen in 5% of patients.
Additionally, the following 3 categories are sometimes considered within the spectrum of multiple sclerosis:
- Clinically isolated syndrome: This is often classified as a single episode of inflammatory CNS demyelination.
- Fulminant: This is characterized by severe multiple sclerosis with multiple relapses and rapid progression toward disability.
- Benign: This features an overall mild disability course with rare relapses.
When discussing multiple sclerosis, clinicians commonly focus on the relapsing-remitting course due to its high prevalence among affected patients. Relapses in relapsing-remitting multiple sclerosis often show partial or complete recovery over weeks or months, sometimes without treatment. However, residual symptoms from these relapses, without complete recovery, can accumulate over time and contribute to overall disability. Diagnosis of relapsing-remitting multiple sclerosis typically requires evidence of at least 2 CNS inflammatory events. Although various diagnostic criteria exist for multiple sclerosis, the general principle for diagnosing the relapsing-remitting course involves establishing episodes separated in "time and space."[3]
This entails that episodes must be temporally separated and involve distinct locations within the CNS. A prompt diagnosis of multiple sclerosis enables the timely initiation of disease-modifying therapy, leading to effective management.[1] Treatment goals include decreasing relapses and magnetic resonance imaging (MRI) activity while minimizing permanent disability and addressing various patient concerns such as bladder and bowel dysfunction, depression, cognitive impairment, fatigue, sexual dysfunction, sleep disturbances, and vertigo.
Etiology
Although the exact etiology of multiple sclerosis is unknown, factors involved in pathogenesis are broadly grouped into 3 categories— immune factors, environmental factors, and genetic associations.
Dysimmunity with an autoimmune attack on the CNS is the leading hypothesized etiology of multiple sclerosis. The postulated "outside-in" mechanism involves CD4+ proinflammatory T cells among various proposed mechanisms.[4] Researchers hypothesize that an unknown antigen triggers and activates Th1 and Th17 cells, leading to their attachment to CNS endothelium, crossing the blood-brain barrier, and subsequently causing an immune attack through cross-reactivity. Conversely, the "inside-out" hypothesis suggests an intrinsic CNS abnormality triggering and resulting in inflammatory-mediated tissue damage.[4]
Environmental factors, such as latitudinal gradients observed in various countries, have been extensively studied.[5] Vitamin D deficiency has been considered a possible etiology for the noted predisposition of populations in higher latitudes to multiple sclerosis.[6] Certain infections, including Epstein-Barr virus, may also contribute to the disease.[7] Complex interactions between various environmental factors and patient genetics are apparent, and ongoing research aims to understand these pathways more comprehensively.
Patients with biological relatives with multiple sclerosis have a heightened risk of developing the condition.[8] Having a first-degree relative with multiple sclerosis is associated with a 2% to 4% risk of developing multiple sclerosis as compared to 0.1% in the general population.[9] Concordance rates are higher in monozygotic twins (20% to 30%) compared to dizygotic twins (5%).[10] A 2% concordance exists between parents and children, which is still 10- to 20-fold higher risk than in the general population.[11]
The human leukocyte antigen (HLA) DRB1*1501 allele strongly correlates with multiple sclerosis and is one of the most studied alleles relative to multiple sclerosis linkage.[12] No defined Mendelian form of genetic occurrence is apparent, and implications point to numerous genes.[13]
Polymorphisms in several genes may be associated with a slightly increased risk of multiple sclerosis, including the following:[14]
- Immunity-related genes: HLA-DR, IL2RA, IL4, IL6, IL12B, IL17R, IRF5, CD24, CD58, and EVI5
- Vitamin D metabolism: VDR and CYP27B1
- Certain genes in mitochondrial DNA
- Fibrinolysis: PAI-1
- CNS function and repair: ApoE and DPP6
Epidemiology
Multiple sclerosis is the most common immune-mediated inflammatory demyelinating disease of the CNS. This condition affects approximately 400,000 individuals in the United States and 2.5 million individuals worldwide.[15] The disease is 3-fold more common in females than in males.[15] Although onset typically occurs in individuals between the ages of 20 and 40, multiple sclerosis can present at any age, with the mean age of onset being 25 to 29 for relapsing-remitting multiple sclerosis and 39 to 41 for primary progressive multiple sclerosis.[16] Almost 10% of the cases are present before the age of 18.[17] The overall prevalence is cited as 1 in 1000 for populations of European ancestry.[18]
Less is known about the prevalence of multiple sclerosis in non-European populations, with most data indicating lower prevalence in individuals of East Asian and African descent.[19] However, recent studies have observed a higher prevalence in African-American populations, similar to those with European ancestry.[19] Multiple sclerosis demonstrates a prevalence gradient based on latitude, with higher prevalence in northern latitudes of Europe and North America. Additionally, observations have noted variable genetic susceptibility factors among different human subpopulations, apart from latitude, suggesting poorly understood genetic factors interacting with environmental influences.
Several studies have highlighted that populations migrating to regions with higher multiple sclerosis prevalence during childhood also adopt a higher risk of acquiring multiple sclerosis.[20] However, other studies have raised doubts about this observation.[21] Neither genetic nor external risk factors can solely account for the epidemiological patterns seen in multiple sclerosis. Notably, multiple sclerosis stands as the leading cause of permanent disability among young adults.[16] One study reported an incidence rate of pediatric-acquired multiple sclerosis at 0.51 per 100,000 person-years.[9]
Pathophysiology
The pathophysiology of multiple sclerosis primarily affects the CNS and involves various areas such as the cortical gray matter, periventricular and juxtacortical white matter, optic nerves, spinal cord, cerebellum, and meninges.
The 2 fundamental processes that constitute general pathological processes observed in multiple sclerosis patients include:
- Focal inflammation results in macroscopic plaques and injury to the blood-brain barrier.
- Neurodegeneration involves microscopic damage to various components of the CNS, such as axons, neurons, and synapses.
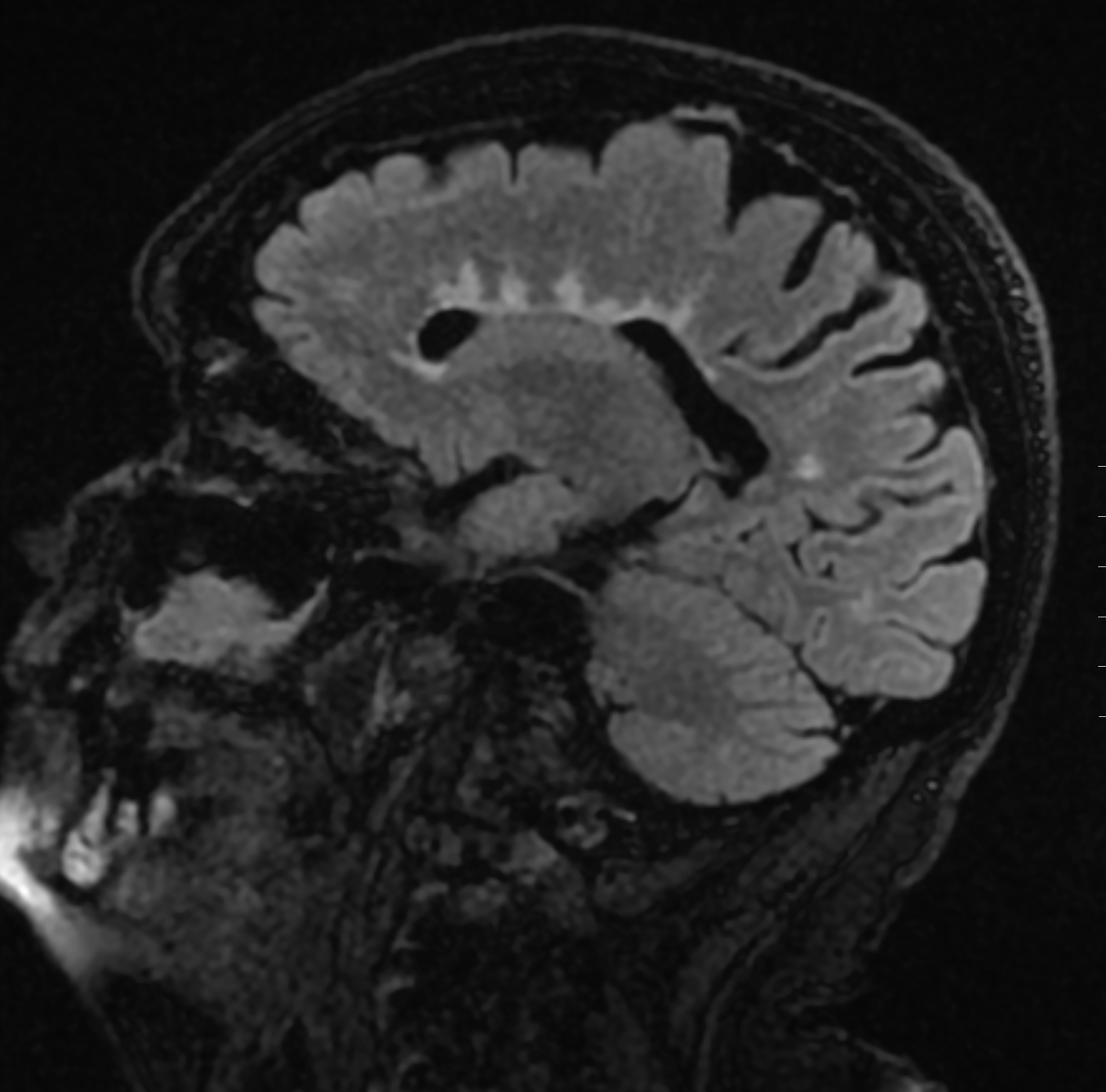
Together, these 2 primary processes result in macroscopic and microscopic injury. Lesions, called plaques, occur in waves throughout the disease course and result from focal inflammation. Multiple sclerosis plaques predominantly center around small veins and venules, displaying sharp margins. The chief components of plaque pathology include myelin loss, edema, and axonal injury. During active plaque inflammation, disruption of the blood-brain barrier corresponds to enhancement observed on MRI scans. As the inflammatory process subsides over time, it leads to the formation of an astrocytic scar (see Image. Perivascular Plaques in Multiple Sclerosis as seen in MRI).
Microscopically, multiple sclerosis lesions show mononuclear infiltrates with perivenular cuffing and infiltration surrounding the white matter. Innate immune cells such as monocytes and macrophages stimulate T-cell migration across the blood-brain barrier, resulting in blood-brain barrier injury and systemic immune cell infiltration. Microglia, the primary antigen-presenting cells of the primary CNS, often precede cell entry. This CNS injury triggers cytotoxic activities in microglia, leading to the release of nitric oxide and other superoxide radicals. Inflamed areas with blood-brain barrier breakdown are visible on MRI as gadolinium-enhancing lesions.
Recently, a greater understanding of the critical role of B cells and antibody production has been recognized in the pathogenesis of multiple sclerosis.[22] B-cell follicles in the meninges of multiple sclerosis patients have been noted, and they are associated with early-onset multiple sclerosis.[23] The pathological events ultimately lead to demyelination, neuroaxonal degeneration, loss of synapses, dying-back oligodendrogliopathy, tissue injury, and astrogliosis.
Histopathology
Histologically, multiple sclerosis plaques are primarily characterized by inflammation and myelin breakdown.[24] Additional features include neurodegeneration and oligodendrocyte injury. The common histopathological stains used to detect multiple sclerosis, with adjunct immunohistochemistry assisting in diagnosis, include hematoxylin and eosin staining, myelin stains such as Luxol fast blue, monocyte and macrophage markers such as CD68, and axonal and astrocyte stains.
Active plaques exhibit varying degrees of the following features:
- Extensive macrophage infiltration
- Myelin debris often found within macrophages
- Presence of major myelin protein, notably in late active plaques
- Perivascular inflammatory infiltrates
- Presence of lymphocytes, particularly CD8-positive cytotoxic T cells
- Plump-shaped and mitotic astrocytes
- Variable degrees of oligodendrocyte injury
- Activated microglia, particularly evident in the peri-plaque white matter zone
Chronic plaques are known for their circumscribed demyelinated lesions, and they occur more frequently and exhibit the following features:[24]
- Hypocellularity and demyelination
- Macrophages laden with myelin
- Relatively decreased perivascular inflammation compared to active plaques
- Resolving edema
- In remyelinated plaques, thinly myelinated axons and axons with newly formed myelin sheaths are apparent.
- Presence of oligodendrocyte precursor cells, typically seen in remyelinated plaques
History and Physical
Multiple sclerosis presents with a broad range of symptoms reflective of the multifocal lesions of the CNS. The severity and diversity of symptoms are influenced by the burden, location, and extent of tissue injury. Interestingly, symptoms may not always align with MRI evidence of active plaques due to the involvement of repair mechanisms and neural plasticity in tissue injury and recovery processes.
Typical clinical manifestations noted in patient history include:
- Vision symptoms such as vision loss (either monocular or homonymous), double vision, symptoms relating to optic neuritis, and pain with eye movement
- Vestibular symptoms such as vertigo and gait imbalance
- Bulbar dysfunction, which manifests as dysarthria and dysphagia
- Motor symptoms such as weakness (hemiparesis, monoparesis, or paraparesis), tremors, spasticity, and fatigue [25]
- Sensory symptoms such as loss of sensation, paresthesias, dysesthesias, and a band-like sensation around the chest or abdomen
- Urinary and bowel symptoms ranging from incontinence, retention, urgency, constipation, diarrhea, and reflux
- Cognitive symptoms such as memory impairment, executive function impairment, and difficulty concentrating
- Psychiatric symptoms such as depression and anxiety
- Brainstem symptoms such as facial muscle weakness and/or reduced facial sensations, diplopia, oscillopsia (jerking sensation in the visual field)
Features considered atypical for multiple sclerosis include seizures, steady progression of symptoms, deficits developing rapidly within minutes, onset before age 10 or after 50, rigidity or sustained dystonia, cortical deficits such as apraxia, alexia, aphasia, or neglect, and early onset of dementia.
The relapsing-remitting course of multiple sclerosis, observed in a majority of patients, is characterized by exacerbation and relapses of neurological symptoms, with stability between episodes.[26] The following features generally characterize the relapsing-remitting course of multiple sclerosis:
- New or recurrent neurological symptoms
- Symptoms developing over days and weeks
- Symptoms lasting between 24 and 48 hours
Symptoms from relapses frequently resolve. However, over time, residual symptoms relating to episodes of exacerbation accrue. This accrual of symptoms, generally after 10 to 15 years, results in long-term disability over time. Neurological manifestations are heterogeneous in severity and degree of recovery. The secondary progressive course is often noted in patients with relapsing-remitting after 10 to 15 years of onset and is characterized by a more gradual worsening of symptoms with continued progression with or without superimposed relapses.[27]
A small subset of patients experience a progressive worsening of disability from the disease's onset, known as the primary progressive course of multiple sclerosis. Clinical manifestations in this course commonly include myelopathy, cognitive symptoms, and visual impairments. Diffuse and chronic symptoms may arise from global brain atrophy and widespread cortical demyelination.
The physical examination aligns with evaluating the patient's illness history and includes the aspects mentioned below.
HEENT:
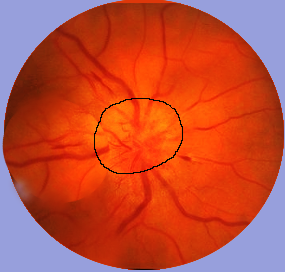
- Assessment for optic neuritis, which typically presents as subacute monocular central vision loss, along with pain upon eye movement (see Image. Optic Neuritis as an Indicator of Multiple Sclerosis)
- Observation of difficulty in adducting during lateral gaze, indicating internuclear ophthalmoplegia
- Other conditions, such as nystagmus, diplopia, hearing loss, and facial pain
Neuromuscular/neurological:
- Partial transverse myelitis is typically unilateral or bilateral and is characterized by sensory disturbances
- Brainstem symptoms often include diplopia, dysphagia, dysarthria, and ataxia
- The Lhermitte sign is often described as a shock-like sensation with neck flexion
- Hyperreflexia, tremors, muscle spasms, and weakness
Genitourinary:
- Urinary incontinence/retention with an assessment of residual bladder volume [28]
- Erectile dysfunction with consideration of a nocturnal penile tumescence stamp test if indicated
Isolated syndromes:
Isolated syndromes may present as:
- Radiographically isolated syndrome: MRI brain lesions that are characteristic of multiple sclerosis but are found in patients, usually incidentally, but they do not have any symptoms of multiple sclerosis.
- Clinically isolated syndrome: Isolated symptom that may not fulfill diagnostic criteria for multiple sclerosis but can lead to clinically definite multiple sclerosis.
If multiple sclerosis is suspected but the patient does not present with typical symptoms, the symptoms mentioned below should prompt further inquiry.[29]
- Sleep disorders, including obstructive sleep apnea, nocturia, insomnia, and restless legs
- Transient (paroxysmal) neurological events, which typically last for seconds and occur with frequencies ranging from hundreds of times per day to only occasionally, may include:
- Abnormal or unexplained sensation spreading across the body
- Brainstem symptoms such as blurred vision, diplopia, dysarthria, and vertigo
- Motor symptoms such as transient inhibition of motor function, tonic spasms, and ataxia
- Gustatory symptoms such as taste hallucination and altered taste
- Hypothermia or hyperthermia (very rarely)
- Pulfrich phenomenon (based on a mismatch of visual acuity between eyes)
- Objects moving in a straight line appear to be in an elliptical orbit
- May present with difficulty crossing roads, pouring liquids, playing ball sports, or feeling cars swerving in direction while driving.
- The sense of uselessness or loss of function in hand (known as "useless hand of Oppenheim")
- The Lhermitte phenomenon, occurring with less commonly observed triggers, such as limb movements, neck extension, or coughing [30]
Red Flags for Alternative Diagnoses
Red flags that should alert the clinician to the possibility of other diagnoses include the following:
- Hyperacute presentation (maximal deficit in minutes to hours)
- Progressive ataxia or cognitive dysfunction
- Family history of any other neurological disease
- Encephalopathy
- Short-lasting symptoms (minutes to hours)
- Rapidly progressive disease
- Failure to remit
- Leptomeningeal disease
- Progressive ataxia
- Cognitive dysfunction
- Complete or fluctuating ophthalmoplegia
- Headache and/or meningismus
- Multiple cranial neuropathies or hearing loss
- Symptoms of systemic disease such as night sweats, weight loss, and fever
- Nonspecific neurological examination findings and/or neurological symptoms not easily localized to the CNS (such as isolated fatigue)
Evaluation
Pathognomonic tests do not exist to diagnose multiple sclerosis. Diagnosis is established by considering the patient's history and physical examination, along with MRI findings, evoked potentials, and cerebrospinal fluid (CSF) or blood studies, while also excluding other causes of the patient's symptoms. Clinically, a diagnosis of multiple sclerosis is supported by evidence of one or more relapses, which can be confirmed through objective clinical evidence of one or more lesions or objective clinical evidence of one lesion with reliable historical evidence of a prior relapse.
Dissemination in space (DIS) and dissemination in time (DIT) are 2 key criteria for accurately diagnosing multiple sclerosis. DIS is assessed by integrating information from the patient's history and physical examination to determine the location of CNS involvement. MRI and evoked potentials also have vital roles in establishing DIS. DIT is established by charting the disease course with a thorough history and documenting the presence of multiple exacerbations over time. The 2010 McDonald criteria determined that new lesions can demonstrate DIT on a follow-up MRI compared to a baseline scan.[31]
DIS is established by observing at least a T2 lesion in 2 of the 4 following CNS sites—spinal cord, infratentorial, juxtacortical, and periventricular regions. Revisions in the 2017 McDonald criteria increased the sensitivity of diagnosis by introducing oligoclonal bands in the CSF analysis as a marker for establishing DIT. Symptomatic lesions were also included to establish DIT and DIS, and cortical lesions were used to demonstrate DIS.[32]
Evoked potentials help demonstrate slowed conduction indicative of subclinical involvement. These findings are often asymmetric. MRI, CSF, and blood studies are essential in ruling out other etiologies. When possible, all patients should undergo an MRI. Additionally, specific blood studies such as complete blood count (CBC), thyroid-stimulating hormone (TSH), vitamin B12 levels, erythrocyte sedimentation rate (ESR), and antinuclear antibody (ANA) testing should be performed as part of the diagnostic workup.
The main characteristics of multiple sclerosis lesions on brain MRI can be outlined as follows:
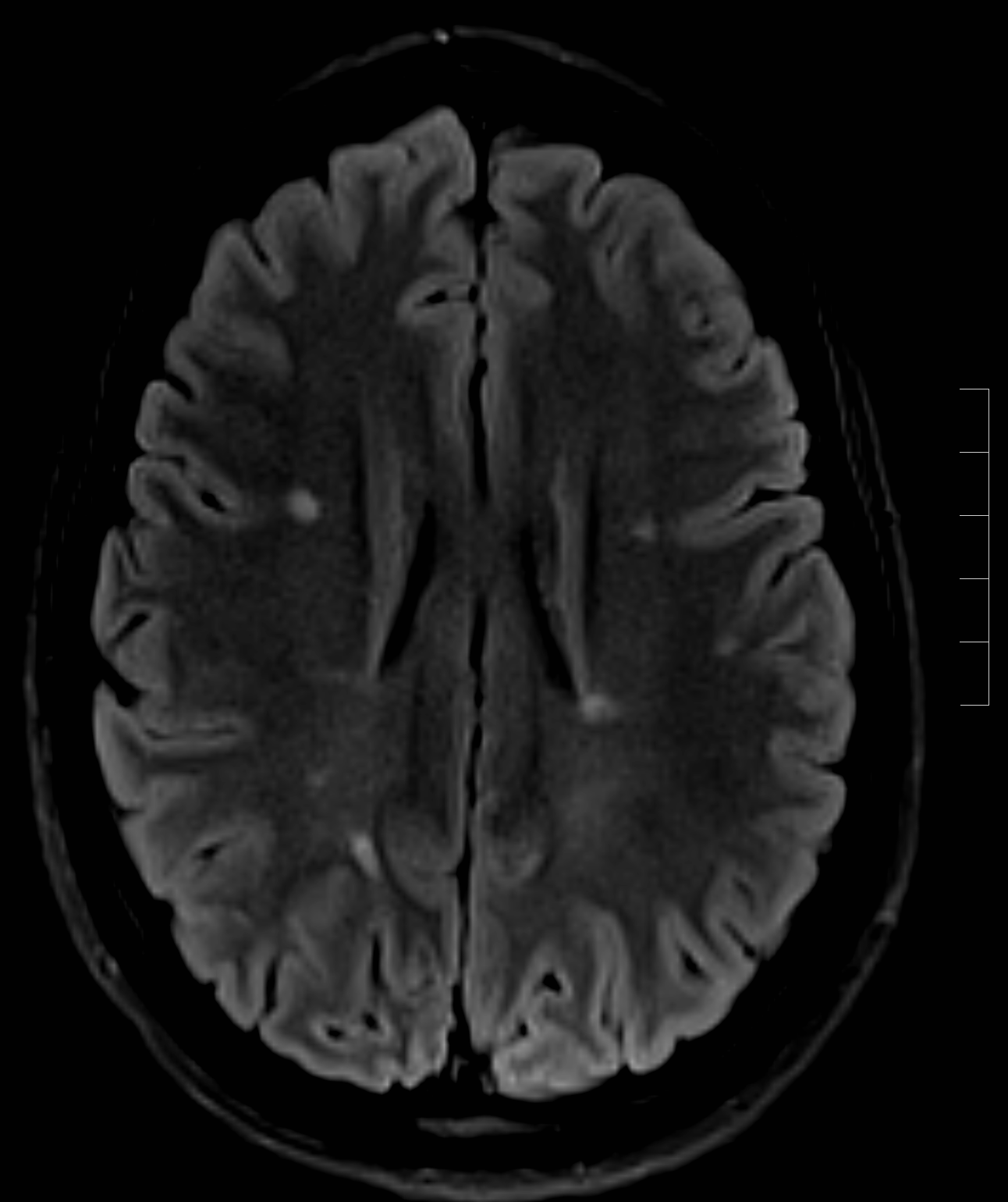
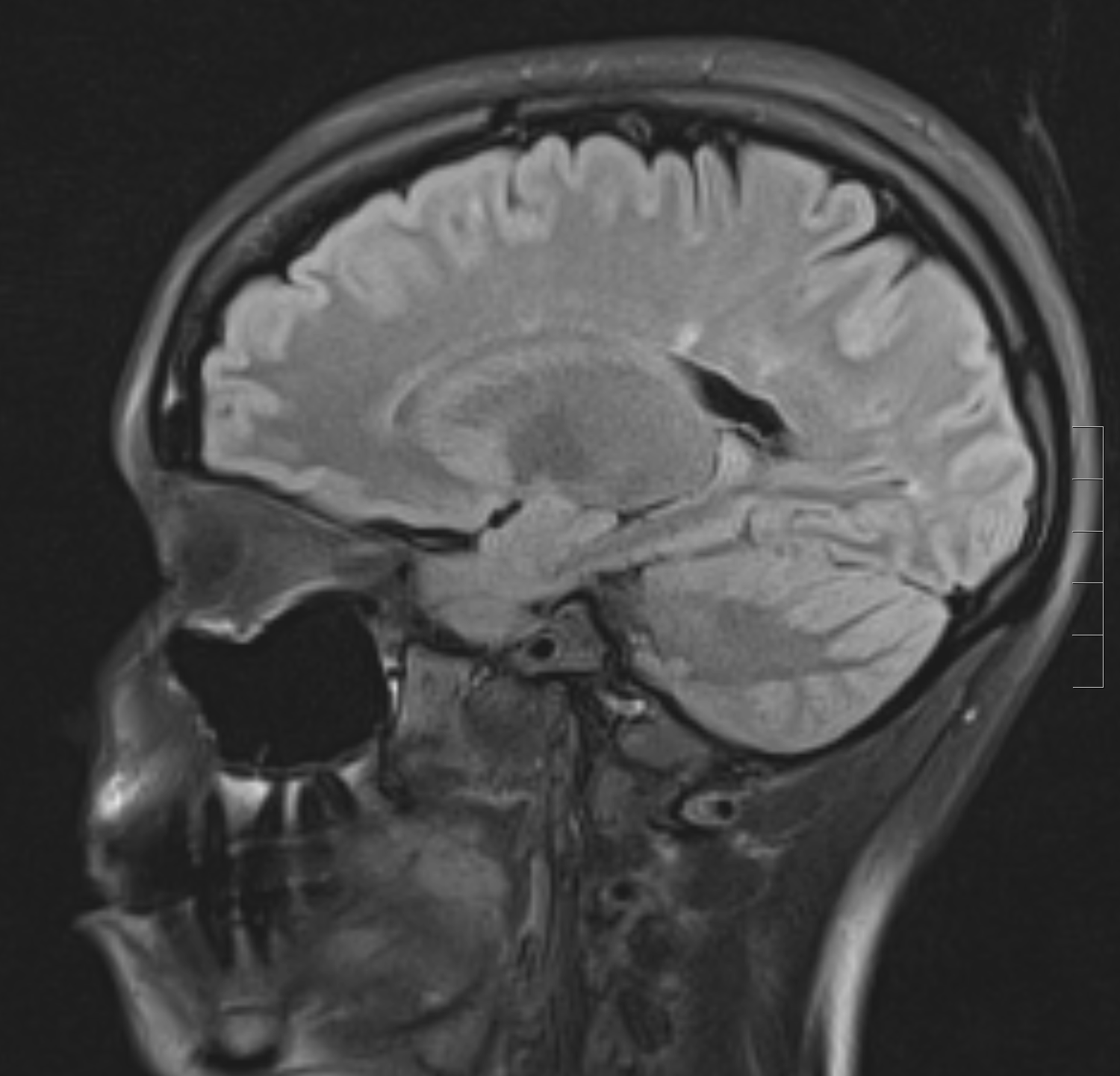
- Lesions are T2 hyperintense and T1 isointense or hypointense, also known as black holes (see Image. Sagittal FLAIR MRI Brain Image Demonstrating Linear Hyperintense Lesions).
- Lesions are typically oval or patchy.
- A high predilection for periventricular white matter.
- Lesions are oriented perpendicular to the ependymal surface, known as Dawson fingers (see Image. Sagittal FLAIR Sequence Demonstrating a Hyperintense Lesion on MRI).
- Active lesions often exhibit gadolinium enhancement, presenting as diffuse or rim enhancement.
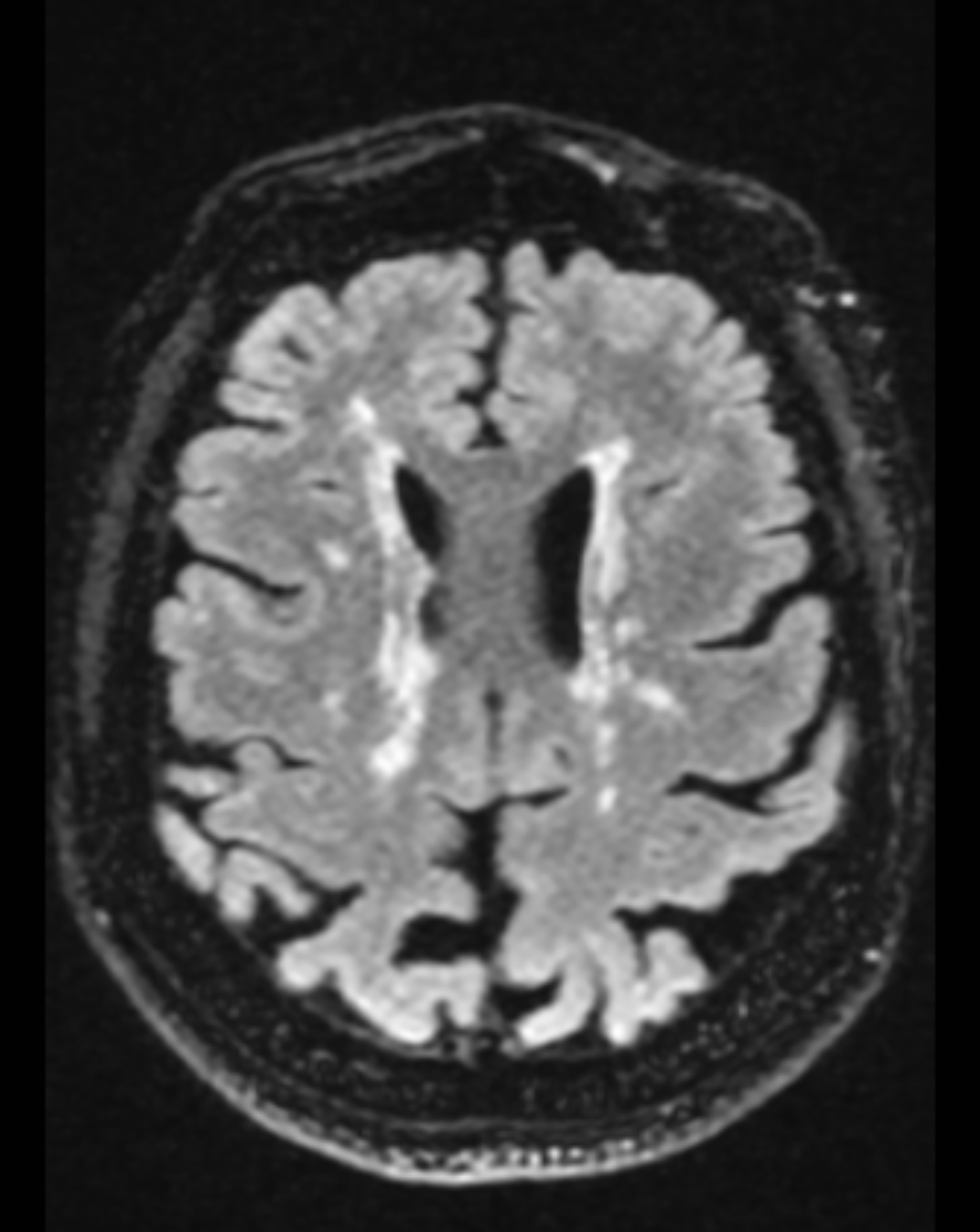
- Thinning of the corpus callosum and parenchymal atrophy (see Image. Axial FLAIR Sequence Demonstrating an Advanced Lesion Burden on MRI).
- The disappearance of a black hole is most likely due to the resolution of edema and remyelination.[33]
Spinal cord lesions typically exhibit the following MRI characteristics:
- Typically located in the cervical or thoracic cord, often in the dorsolateral region.
- Little or no cord swelling observed.
- Lesions are focal, with clearly circumscribed and delineation on T2-weighted sequences.
- Size ranges from 3 mm to less than 2 vertebral segments in length.
- Unequivocal hyperintensity on T2-weighted sequences visible in 2 planes (eg, sagittal and axial)
The classic abnormal CSF findings in multiple sclerosis typically include elevated protein and myelin basic protein levels, occasional leukocytes (mainly mononuclear cells), and increased levels of total immunoglobulin G (IgG), free kappa light chains, and oligoclonal bands.[34]
When clinical, imaging, or laboratory features are atypical of multiple sclerosis, patients are tested for aquaporin-4 (AQP4) IgG serum autoantibody and the myelin oligodendrocyte glycoprotein IgG autoantibody (MOG-IgG).
Table. Diagnostic Tests for Multiple Sclerosis
| Tests |
Percentage of Patients with Abnormal Test Results |
| Brain MRI |
70% - 95% |
| Somatosensory evoked potentials |
50% |
| Visual evoked responses |
50% - 90% |
| Brainstem auditory evoked responses |
20% - 55% |
| Cerebrospinal fluid IgG index |
75% |
| Cerebrospinal fluid oligoclonal banding |
85% - 95% |
Table reference is [34].
Treatment / Management
Glatiramer acetate, dimethyl fumarate, fingolimod, interferon-beta preparations, natalizumab, and mitoxantrone are some of the primary disease-modifying therapies. Immediate treatment initiation upon diagnosis is crucial for multiple sclerosis. Short-term goals focus on decreasing MRI lesion activity, while long-term goals aim to prevent secondary progressive multiple sclerosis. Post-treatment challenges include ensuring patient compliance and monitoring for drug toxicity.
In the realm of treatment and management for multiple sclerosis, several disease-modifying therapies, as mentioned below, offer various mechanisms to address the underlying pathology.
Glatiramer acetate: This is a synthetic polypeptide mixture that may act as a ligand for major histocompatibility complex molecules, limiting their activation and promoting regulatory cell induction. This drug may also have neuroprotective and repair mechanisms.[35] Glatiramer acetate is administered subcutaneously and is generally well-tolerated; however, this drug is ineffective for progressive forms of multiple sclerosis.
Interferon-beta preparations: These preparations act through multiple mechanisms, including modulation of T- and B-cell function, cytokine expression alteration, potential role in blood-brain barrier recovery, and reduction in matrix metalloproteinase expression. The administration is subcutaneously or intramuscularly, and they may cause flu-like symptoms and possibly briefly worsen patients' neurological symptoms.
Natalizumab: This drug is an intravenously (IV) administered humanized monoclonal antibody that blocks leukocyte adhesion to vascular endothelial cells, thereby inhibiting leukocyte migration into the CNS. Although generally well tolerated, natalizumab may cause mild headaches, and flushing may occur during IV administration.
Mitoxantrone: This is an IV-administered chemotherapeutic agent used to treat multiple sclerosis due to its effects on DNA repair and RNA synthesis. A possible effect on cellular and humoral immunity may represent the therapy mechanism for multiple sclerosis.[36] However, its use is limited due to the various adverse effects that have been documented, including amenorrhea and alopecia.
Fingolimod: This is an orally administered drug with immunomodulatory effects, possibly relating to the inhibition of T-cell migration. However, possible adverse effects include lymphopenia, bradycardia, and hepatotoxicity, thereby necessitating careful monitoring.
Patients with secondary progressive, progressive-relapsing, and primary progressive multiple sclerosis primarily experience neurodegenerative processes. Due to this, disease-modifying therapies show varying effectiveness, ranging from possible benefits to limited impact on disease progression. Typically, younger patients with a shorter duration of progression tend to benefit more from these therapies.
Guiding Principles for Acute Relapse Management
Several principles guide the treatment of acute relapses in multiple sclerosis, including:
- Addressing possible underlying processes that could have triggered a relapse, such as an infection or metabolic derangement
- Providing symptomatic treatment based on specific neurological symptoms
- Administering a short course of corticosteroids to assist in recovery
- Implementing rehabilitation programs involving physical and occupational therapy for comprehensive management
Women of childbearing age should avoid certain medications due to their potential risks, as listed below.
- Teratogens: Teriflunomide, cladribine, siponimod, fingolimod, and ozanimod
- Drugs associated with a higher risk of rebound symptoms upon discontinuation: Fingolimod, siponimod, natalizumab, and ozanimod
Treatment of Acute Exacerbation of Multiple Sclerosis
Neurological symptoms may include increased disability, impairments in strength, cerebellar function, vision, or significant sensory disturbances.
- IV or oral steroids may be prescribed by a physician, as described below, depending on a patient's conditions and symptoms.
- IV methylprednisolone: This can be administered as a 3- to 7-day course at 500 to 1000 mg daily, optionally followed by a short prednisone taper.[37]
- Oral prednisone: This can be administered at a dosage of 1250 mg/d of prednisone, with/without a short taper, and is an alternative to 3 to 7 days of oral methylprednisolone administered at 1000 mg/d.
- Plasma exchange (PLEX) is recommended if a poor glucocorticoid response occurs.[38]
- PLEX is administered daily or every other day for a total of 3 to 7 treatments.
Differential Diagnosis
The differential diagnosis of multiple sclerosis is extensive and can be categorized into 7 categories, as listed below.
- Other demyelinating or inflammatory CNS syndromes:
- Optic neuritis
- Marburg disease
- Acute disseminated encephalomyelitis
- Devic neuromyelitis optical
- Susac syndrome [39]
- Primary cerebral vasculitis and partial transverse myelitis
- Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS), a rare form of encephalomyelitis typically affecting the spinal cord, cerebellum, and brainstem [40]
- General inflammatory and autoimmune syndromes:
- Systemic lupus erythematosus
- Wegener granulomatosis
- Sarcoidosis
- Antiphospholipid antibody syndrome
- Behcet syndrome
- Sjögren syndrome
- Infectious etiologies:
- Lyme disease
- Syphilis
- HIV
- Herpes viruses
- Vascular etiologies
- Migraine headaches
- Dural arteriovenous fistula
- Small vessel ischemia
- Ischemic optic neuropathy (arteritic and nonarteritic)
- Vascular malformations and emboli
- Metabolic causes:
- Vitamin deficiencies
- Thyroid disease
- Hereditary ataxias
- Adult-onset leukodystrophy, such as adult-onset adrenoleukodystrophy
- Uncommon genetic etiologies:
- Mitochondrial cytopathy
- Fabry disease
- Alexander disease
- Hereditary spastic paraplegia
- Neoplastic causes include primary CNS malignancies, such as gliomas and meningiomas, or metastasis
Prognosis
The prognosis and severity of multiple sclerosis vary widely among patients,[41] and the disease often exhibits mild symptoms early, which worsens over time.
Factors that suggest a worse prognosis include:
- Male gender
- Progressive course
- Primarily pyramidal or cerebellar symptoms
- More frequent relapses
- Minimal recovery between relapses
- Multifocal onset
- High early relapse rate
- Large lesion load and brain atrophy on MRI
Factors that suggest a favorable diagnosis include:
- Female gender
- Relapsing course
- Mild relapses
- Good recovery between exacerbations
- Primarily sensory symptoms
- The long interval between the first and second relapses
- Low lesion load on MRI
- Presentation of optic neuritis
- Full recovery from exacerbations
Complications
Long-term disability in multiple sclerosis results from incomplete recovery after each relapse, leading to an accumulation of symptoms over time.
- Impaired mobility is observed in most long-term multiple sclerosis patients due to various factors. The reduction in mobility is multifactorial and possibly related to defective motor control and vestibular symptoms.
- Brain stem lesions involving the oculomotor pathways can cause chronic diplopia, which may be managed with prisms or surgery.
- Chronic vertigo, another common issue, is a possible source of morbidity and may respond to medications such as meclizine, ondansetron, or diazepam.
- Chronic dysphagia due to bulbar dysfunction can lead to chronic aspiration.
- Cerebellar tremors can potentially significantly affect a person's disability. While wrist weights may help manage tremors, potential superimposed weakness can preclude their use.
- Urinary tract infections, considered long-term complications, can occur due to bladder dysfunction, which often necessitates consultation with urology specialists.
- Constipation is the most frequent gastrointestinal complication, and this issue can be managed with patient education, increased fiber intake, and bulk-forming agents.
- Erectile dysfunction is treated with oral phosphodiesterase-5 inhibitors if present.
- Cognitive impairment, mood disorders, and generalized fatigue are considered long-term sources of morbidity, and they are managed in various ways, often involving subspecialty care.
Consultations
Multiple sclerosis is a complex neurological disorder that leads to various neurological and non-neurological symptoms, disabilities, and complaints. A comprehensive team approach involves specialists from:
- Neurology and neuro-ophthalmology
- Psychiatry and cognitive psychology
- Pain management
- Nursing and physician assistants
- Speech therapy
- Occupational therapy
- Social work
- Physical medicine and rehabilitation
- Urology (in the setting of genitourinary complications)
- Gastroenterology (in the setting of gastrointestinal complications)
Deterrence and Patient Education
Diagnosing multiple sclerosis can be challenging for patients, and clinicians play a crucial role in providing supportive counseling regarding the diagnosis. Predicting the disease course is complex, so clinicians must educate patients about the varied possibilities in disease progression. In addition, it is important to emphasize that many patients respond well to treatment and to explain the role of effective medications. Patients should also be directed to reputable online sources such as the Multiple Sclerosis International Federation and the National Multiple Sclerosis Society to learn more about their condition. Educating patients about the nature of relapses and long-term complications is also vital.
Patients should be informed to contact their treating clinician promptly if they experience new neurological symptoms lasting more than 24 hours, as this may require corticosteroid administration. In addition, it is crucial to emphasize smoking cessation, take vitamin D supplementation, maintain a balanced diet, and adhere to lifestyle modifications. Patients should also receive counseling on the significance of adhering to disease-modifying therapy, considering the adverse effect profile of these medications.
Enhancing Healthcare Team Outcomes
Multiple sclerosis is a complex disease process presenting with sensory, visual, weakness, coordination, and spasticity issues. Other health concerns include bladder and bowel dysfunction, depression, cognitive impairment, fatigue, sexual dysfunction, sleep disturbances, and vertigo. Due to its multisystem impact and reduced life expectancy, optimal management of multiple sclerosis necessitates an interprofessional healthcare team, including neurologists, pain specialists, therapists, nurse specialists, ophthalmologists, mental health nurses, gastroenterologists, urologists, nurses, and pharmacists, who can treat patients with multiple sclerosis.