Continuing Education Activity
An interscalene nerve block anesthetizes most of the territory innervated by the brachial plexus, sparing the inferior trunk. This block is generally performed on patients undergoing shoulder, upper arm or elbow surgery. It is not recommended for hand surgery as the inferior trunk may be spared. This activity reviews the indications, contraindications, and technique involved in performing an interscalene nerve block and highlights the role of the interprofessional team in the care of patients undergoing this procedure.
Objectives:
Describe the parts of the upper extremity that are anesthetized during interscalene nerve blocks.
Outline the steps involved in performing an interscalene nerve block.
Identify risks associated with interscalene nerve blocks.
Explain a structured, interprofessional team approach to provide effective care to and appropriate surveillance of patients undergoing interscalene nerve blocks.
Introduction
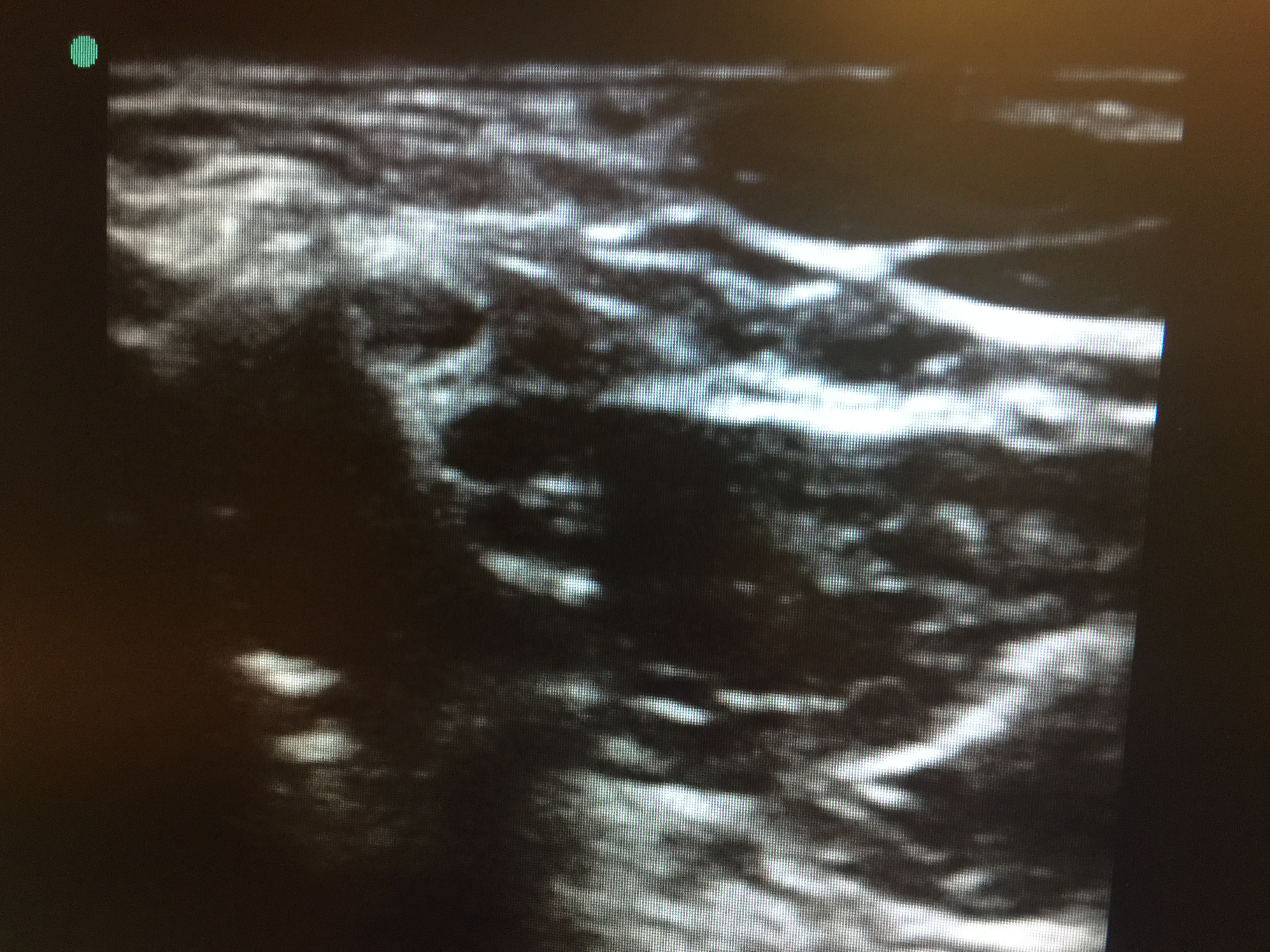
The brachial plexus is a nerve network that supplies the upper extremity. It is formed by C5-T1. It exits the cervical spine and travels between the anterior and middle scalene muscles and then travels distally around the axillary artery. The space between the scalene muscles is called the interscalene groove. This space is palpable behind the lateral head of the sternocleidomastoid muscle and adjacent to the C6 lateral tubercle, also known as Chaissaignac's tubercle. Under ultrasound visualization, the brachial plexus can be typically seen as 2 or 3 hollow circles ("stoplight") that correspond with the superior, middle, and inferior trunks (see Image. Interscalene Nerve "Stoplight" Sign). The inferior trunk can sometimes be difficult to visualize as the muscle gets thicker. Once visualized, injection of a long-acting local anesthetic can block nerve impulses and cause upper extremity numbness and weakness. Structures immediately distal to the nerve block placement consistently block nerve impulses and causes sensory and movement loss.
A regional anesthesia specialist usually performs an interscalene block. It is commonly performed in the preoperative suite or postanesthesia care unit with the patient mildly sedated. The interscalene block covers most of the brachial plexus, sparing the ulnar (C8-T1) nerve. It is a great block for distal clavicle, shoulder, and proximal humerus procedures. Under sterile conditions, the interscalene space is identified either by palpation or ultrasound visualization. A nerve stimulator can also be used as an adjunct to confirm placement. The nerve stimulator causes muscle contractions in the deltoid muscle, arm, or forearm when the corresponding nerve is stimulated. A volume of local anesthetic is injected, typically between 15-25mL. Commonly used local anesthetics include bupivacaine and ropivacaine. Once the local anesthetic is placed, the patient can expect pain relief and limb heaviness for the duration of local anesthetic action.
Side Effects
Side effects and complications of an interscalene block can be divided into 2 parts.
Needle and Local Anesthetic Placement
A misguided needle placement can result in pneumothorax, nerve damage, epidural or intrathecal placement, and spinal cord trauma. Ultrasound use can decrease this risk. Patients with pulmonary comorbidities can also complain of shortness of breath post-block placement due to the blockage of the phrenic nerve. The phrenic nerve traverses anterior to the brachial plexus and can be affected when the volume of local anesthetic travels more proximally. The volume of local anesthetic can also spread posteriorly and affect the cervical plexus, which results in Horner syndrome (ptosis, miosis, and anhidrosis).
Local Anesthetics
Monitoring for local anesthetic toxicity during block placement is required. Commonly used local anesthetics have a maximum dose allowed, and knowledge of these values by the provider is important. Allergic reactions to amide local anesthetic are uncommon; however, ester local anesthetics have para-aminobenzoic acid (PABA), a known allergen.[1]
Anatomy and Physiology
The brachial plexus is a nerve network comprised of the anterior rami from the lower 4 cervical spinal nerves and first upper thoracic spinal nerve (C5, C6, C7, C8, T1). The spinal nerves of the brachial plexus then continue to form the roots, trunks, divisions, cords, and branches. As the 5 roots give rise to the 3 trunks (superior, middle, and inferior), they emerge between the anterior and middle scalene muscles. Each trunk then divides anteriorly and posteriorly behind the clavicle at the apex of the axilla forming a total of 6 divisions. The 6 divisions then combine to make 3 cords (lateral, median, and posterior), which then split into 5 terminal nerve branches (musculocutaneous, axillary, radial, median, and ulnar nerves). [2]
Indications
This block is generally performed on patients undergoing shoulder, upper arm or elbow surgery. It is not recommended for hand surgery as the inferior trunk may be spared. [3]
Contraindications
This block is contraindicated in patients with respiratory insufficiency due to the high likelihood of ipsilateral phrenic nerve block and diaphragmatic hemiparesis. This can lead to a 25% reduction in pulmonary function. Additionally, the recurrent laryngeal nerve may be blocked, which could cause complete airway obstruction with anyone who has an existing vocal cord palsy.
Equipment
To perform the block the health care professional will need:
- Skin prep, for example, chlorhexidine, betadine, alcohol
- Two-inch, 22-gauge, short-beveled, insulated, stimulating needle
- A 3-mL syringe plus 25-gauge needle with local anesthetic for skin infiltration
- One 20- to 30-mL syringe with local anesthetic
- Marking pen
- Sterile gloves
- Peripheral nerve stimulator
- Ultrasound machine
Personnel
The interscalene block requires 2 people. One person will have control of the ultrasound probe and needle, and another person will manage the nerve stimulator as well as the syringe with a local anesthetic.
Preparation
Patient Positioning
The patient can be supine, sitting, semi-sitting, or semi-lateral decubitus. It is most often done with the patient sitting at a 30-degree angle, and a pillow or blanket is placed beneath the patient's chest with the patient looking away from the side of the block. The key things to keep in mind when positioning the patient are:
- The patient should be able to lie comfortably and still in the same position.
- The area on the neck should be adequately exposed.
- There should be enough space between the patient and bed for the ultrasound probe and needle to fit properly if an in-plane posterolateral approach is desired.
Technique or Treatment
Performing Block With Ultrasound[4]
With the patient properly positioned, the skin is disinfected, and the transducer is placed over the neck until the appropriate landmarks and structures are identified. There are 2 commonly accepted techniques for finding the proper image. Firstly, the transducer is placed at the level of the cricoid cartilage medial to the sternocleidomastoid muscle, and the carotid artery is identified. The transducer is then slid laterally until the brachial plexus in between the anterior and middle scalene muscles are identified. The second method is to place the transducer just above the clavicle and identifying the subclavian artery with brachial plexus (the image for a supraclavicular block). The transducer is then moved cephalad towards the patient's neck while keeping the brachial plexus nerves in view until the "stop-light" image is seen. The needle is then inserted in-plane to the transducer entering lateral to medial. If preferred the needle can be inserted medial to lateral as well. Once the needle reaches the interscalene groove, after careful aspiration, the local anesthetic is injected. If a nerve stimulator is used, the patient should exhibit a motor response of the shoulder and arm.
Performing Block Without Ultrasound
Prior to cleaning the skin the proper landmarks are identified and marked with a marking pen. The 3 major landmarks required for the block are the clavicle, the clavicular head of the sternocleidomastoid and the external jugular vein. Another helpful landmark is the cricoid cartilage. After identifying these landmarks, the skin is prepped, and with sterile gloves, the anterior and middle scalene muscle can be palpated. This is located just posterior the clavicular head of the sternocleidomastoid around the level of the cricoid cartilage. The external jugular vein usually crosses the interscalene groove. The skin is then anesthetized with 3-mL local anesthetic subcutaneously, and the needle is then inserted just posterior to the external jugular vein approximately 3 to 4 cm above the clavicle and advanced at an angle perpendicular to the skin plane. With the nerve stimulator connected the needle is advanced until stimulation of the brachial plexus is seen. This occurs in most patients around 1 to 2 cm in depth. The local anesthetic is then injected with intermittent aspirations to avoid intravascular injections.
Complications
Possible complications of the interscalene nerve block include:
- Infection
- Bleeding/Hematoma
- Puncture of vascular structure
- Epidural or subarachnoid injection
- Local anesthetic toxicity
- Permanent nerve injury
- Total spinal anesthesia
- Horner syndrome[5]
- Hemiparalysis of the diaphragm[6]
- Pneumothorax
Clinical Significance
The interscalene block allows for coverage of the lateral two-thirds of the clavicle, shoulder, and proximal humerus. When attempting a blockade of areas in the arm and forearm, it is important to keep in mind that the inferior trunk (C8-T1) is often inadequately blocked and additional blockade of the ulnar distribution may be required. It traditionally has not been reliable for surgery on the hand. The interscalene nerve block is commonly used alone or in conjunction with other forms of anesthesia for pain control during surgery or in the perioperative period.
Enhancing Healthcare Team Outcomes
The interscalne block is a frequently performed procedure by the anethesia nurse, anesthesiologist nurse and the pain specialist. Howver, all those who perform this block must be fully aware of the potential complications and have resuscitative equipment in the room. The patient must be monitored by a dedicated nurse during the procedure. When done well, the interscalene block does allow for surgery on the arm without the need for general anesthesia.[7][8][9]