Introduction
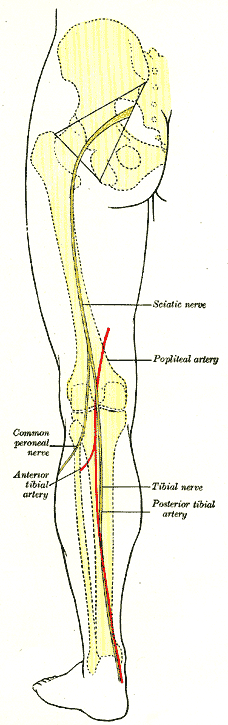
The posterior tibial nerve describes the distal end of the tibial nerve as it passes around the medial malleolus in the tarsal tunnel. Anatomically, the structure is a continuation its parent tibial nerve in a specific region of the distal extremity and does not represent a branch of the tibial nerve or a distinct structure. Accordingly, some texts will refer to it as the tibial nerve. Moreover, there is no anterior tibial nerve at the level of the foot or ankle. However, many authors and texts refer to the structure as the posterior tibial nerve due to its clinical significance. The tibial nerve is both a motor and sensory nerve is the largest distal extension of the sciatic nerve and is a branch of the lumbosacral plexus carrying spinal roots L4, L5, S1, S2, and S3. In the distal thigh, the tibial nerve splits from the sciatic nerve, passes through the popliteal fossa, runs under the arch of the soleus and continues distally on its undersurface to finally descend posterior to the medial malleolus, where it earns the distinction of the posterior tibial nerve, and into the foot as the medial and lateral plantar branches. The posterior tibial nerve is susceptible to entrapment in tarsal tunnel syndrome and can be manipulated with anesthesia to provide nerve blockade.[1]
Structure and Function
The posterior tibial nerve is a mixed motor and sensory nerve and courses around the medial malleolus and below the flexor retinacula in the tarsal tunnel. Distal to the medial malleolus, it divides into its terminal branches: lateral plantar, medial plantar, and calcaneal. These branches provide sensory innervation to the plantar foot: the main calcaneal branch supplies the medial plantar heel while the medial and lateral plantar nerves innervate the remainder of the sole of the foot. Proximally, the articular branch of its origin, the tibial nerve, carries sensory information from the knee joint and the sural nerve branch, which runs distal with the small saphenous vein and anastomoses with a peroneal nerve branch, terminates as the lateral dorsal cutaneous nerve of the foot with this distal portion being a part of the posterior tibial nerve. Motor innervation by the posterior tibial nerve gets directed to the intrinsic plantar musculature. Specifically, the medial branch innervates the first lumbrical, flexor hallucis brevis, flexor digitorum brevis, and abductor hallucis, while the lateral branch supplies the plantar muscles of the foot. The posterior tibial nerve is not responsible for any reflexes.[2][3]
Embryology
The lumbosacral plexus, and consequently the tibial and posterior tibial nerves, are of ectodermal origin while the muscles, blood vessels, and bones of the limbs they supply are of mesodermal derivation. The sacral plexus consists of the sacral spinal nerves S1 through S4 and their respective anterior rami along with branches from spinal roots L4 and L5. The anterior rami of L1 through L4 nerve roots along with contributions from T12 collect to form the lumbar plexus. The and femoral nerves arise from the lumbar plexus while the sciatic nerve arises from the sacral plexus and carries fibers from L4 to S3.
Blood Supply and Lymphatics
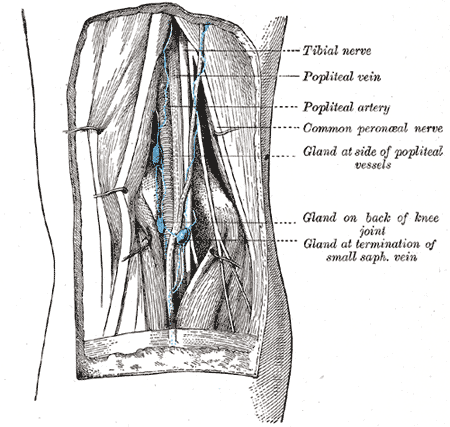
The posterior tibial artery descends around the medial malleolus adjacent to the posterior tibial nerve and continues to track with the medial plantar nerve branch on the medial side of the foot. The artery runs just posterior to the flexor digitorum longus tendon in the lower leg near the ankle. Clinically, a common place to assess blood flow to the foot is through palpation of the posterior tibial artery posterior to the medial malleolus. Dividing into superficial and deep, the lymphatics of the lower extremity parallel the venous distribution. The inguinal lymph nodes receive drainage from the great saphenous vein while the popliteal nodes receive lymphatic drainage from the lesser saphenous vein.[4] The posterior tibial artery, vasa vasorum from which supply the posterior tibial nerve at the level of the medial malleolus, is subject to coronary artery disease causing limited blood flow and thus ischemia to the nerve.[5]
Nerves
Other nerves originating from the sacral plexus with the sciatic nerve include the pudendal, posterior femoral cutaneous, tibial, common fibular, inferior gluteal, superior gluteal. The tibial nerve, a branch of the sciatic nerve, can be referred to as the posterior tibial nerve distally as it courses around the medial malleolus.[6]
Muscles
The tibial nerve delivers motor innervation to the deep muscles of the posterior leg. Muscles innervated include the gastrocnemius, popliteus, soleus, tibialis posterior, flexor digitorum longus, flexor hallucis longus, abductor hallucis, flexor digitorum brevis, flexor hallucis brevis, foot lumbricals, quadratus plantae, flexor digiti minimi, adductor hallucis, foot interossei, abductor digiti minimi. The posterior tibial nerve as a distinct entity provides motor innervation to the intrinsic muscles of the plantar foot.
Physiologic Variants
Though most commonly displaying bifurcation within the tarsal tunnel, the posterior tibial nerve can display trifurcation at this anatomic landmark. Coursing laterally after it branches from the posterior tibial nerve, this rare variant then branches deep to the quadratus plantae muscle.[7]
Surgical Considerations
Initial treatment of tarsal tunnel syndrome is non-operative. These measures include immobilization and night splinting for between 6 to 12 weeks, ant-inflammatory medications and shoe wear modification. If these measures fail, patients may merit consideration for surgical intervention. Pre-operative workup may include radiographs and/or MRI studies to evaluate for tarsal coalition or space-occupying lesions, respectively. Some authors contend that surgical options be limited to those with space-occupying lesions[8]. Patients with pre-operatively identified space-occupying lesions have reportedly improved outcomes, but the release of the tarsal tunnel can be performed in other settings.
Some authors have proposed ultrasound-guided release of the tarsal tunnel.[9]
If a patient opts for an open approach, an incision is made beginning plantar to the navicular tuberosity and extending proximally between the medial malleolus and the calcaneal tuberosity. After careful dissection through superficial veins, the flexor retinaculum is encountered. The midportion of the flexor retinaculum is excised carefully to liberate the underlying structures.[10] If a space-occupying lesion is present, it also requires excision. The abductor hallucis muscle can be incised or reflected iplantardirection to access the distal branches of the posterior tibial nerve as they curve plantarly. Care is taken to ensure the posterior tibial nerve and its branches are completely free of tethers or points of compression. Occasionally, the medial calcaneal branches penetrate the retinaculum placing these branches at risk when the retinaculum undergos excision.
Additionally, the posterior tibial nerve is susceptible to injury with fracture of and during subsequent fixation of medial malleolus fractures along with the tibialis posterior tendon, flexor digitorum longus longus tendon, the posterior tibial artery, and the flexor hallucis longus tendon.[11]
Clinical Significance
Tarsal tunnel syndrome, also called posterior tibial nerve neuralgia or tibial nerve dysfunction refers to an entrapment neuropathy of the posterior tibial nerve within the structures of the tarsal tunnel which is located inferior and posterior to the medial malleolus. The contents of the tarsal tunnel are the tendons of the posterior tibialis, flexor digitorum longus, flexor hallucis longus muscles along with the posterior tibial artery, vein, and nerve (L4-S3). The etiology of this syndrome subdivides into either extrinsic causes including post-surgical scarring, valgus or varus hind-foot, diabetes, lower extremity edema, poorly fitting shoes, trauma, or intrinsic causes. The clinical manifestations occur due to compression of the posterior tibial nerve or its distal branches (the lateral or medial plantar nerve), and the diagnosis is clinical. Pain is typically noted directly over the tarsal tunnel and radiates to the plantar foot’s arch. It is not uncommon for pain to present as shooting or sharp with accompanying plantar numbness and/or paresthesia along the course of the posterior tibial nerve or pain with eversion or dorsiflexion. Management is variable depending on etiology and can be operative or nonoperative.[12]
A posterior tibial nerve block is completed using the posterior tibial artery as a landmark. The needle passes toward the posterior tibial artery behind the medial malleolus, adjacent to the Achilles tendon.