Introduction
The levator palpebrae superioris is a triangular-shaped muscle located in each upper eyelid. The primary function is elevation and retraction of the upper eyelid. It has an abundant blood supply, mainly provided by the ophthalmic and supraorbital arteries (from the internal carotid), anastomosing with branches of the external carotid via angular and superficial temporal arteries through the superior peripheral arcade.[1][2] Lymphatic drainage travels laterally to the preauricular/parotid nodes before draining to the deep cervical lymph nodes.[3] The muscle receives innervation by the superior branch of the oculomotor nerve (cranial nerve III). Problems with the levator palpebrae superioris function or innervation will result in upper eyelid ptosis.[2][4]
Structure and Function
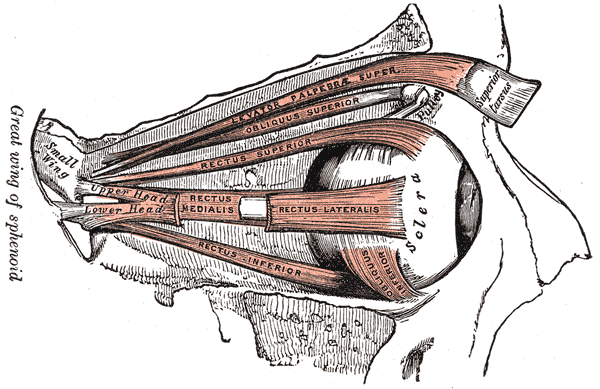
The function of the levator palpebrae superioris muscle is to raise the upper eyelid and to maintain the upper eyelid position. The levator palpebrae superioris muscle origin is the periosteum of the lesser wing of the sphenoid bone, superior to the optic foramen. The muscle travels anteriorly along the superior aspect of the orbit superior to the superior rectus muscle. The supraorbital artery and the frontal and lacrimal nerves are superior to the levator muscle in the orbit. Distally the muscle widens and becomes a tendon sheath known as the levator aponeurosis in the region of the Whitnall ligament, which is a transverse suspensory ligament. The Whitnall ligament appears to be part of the pulley system allowing the horizontal levator muscle to become the more vertical levator aponeurosis.
The Whitnall ligament also forms part of the complex Koornneef orbital septae, which provide support to the globe and orbital components and also serve as an accessory locomotor system. The levator aponeurosis has lateral and medial wings attaching to the respective canthal tendons. The lateral horn is more robust than the medial horn.
The levator aponeurosis has multiple insertions: anteriorly into the upper eyelid skin, inferiorly on the anterior surface of the upper tarsal plate, and with indirect extensions to the superior conjunctival fornix. Posterior to the levator aponeurosis is the superior tarsal muscle (Müller muscle), which is a smooth muscle that also attaches to the superior tarsal plate. The levator palpebrae superioris is not a smooth muscle but a skeletal muscle.[2][5]
Embryology
The levator palpebrae muscle derives from the mesenchyme of the second pharyngeal arch. It begins formation during the sixth week of gestation and develops from lateral and medial mesodermal extensions of the frontal nasal process. Initially, the levator palpebrae muscles begin development as a part of the superior mesodermal complex with the superior rectus muscle and the superior oblique muscles. During the eighth week of gestation, the superior mesodermal complex and lower mesodermal complex fuse, followed by the differentiation of the upper and lower lid structures, including the levator palpebrae muscles.[2][5][6]
Blood Supply and Lymphatics
The internal carotid artery provides most of the levator palpebrae superioris blood supply via branches of the ophthalmic artery. Four arterial systems direct blood to the levator palpebrae muscle: the lacrimal, supratrochlear, and supraorbital arteries and muscular branches of the ophthalmic artery.[7] These branches eventually connect to the superior peripheral arcade, providing blood supply to the superior aspect of the upper eyelid. The superior peripheral arcade connects medially and laterally with the superior marginal arcade, which provides the blood supply to the margin of the upper eyelid. These two arcades form a vast anastomosis with blood from branches of the internal and external carotid arteries.
The internal carotid artery supplies the majority of the blood to the superior peripheral arcade via the branches previously stated. The external carotid artery provides additional blood to the superior peripheral arcade medially via the angular artery (a branch of the facial artery) and laterally via the superficial temporal artery. This complex anastomosis maintains a rich blood supply to the lateral palpebrae superioris.[1][2]
The venous drainage of the muscles of the orbit is via the superior and inferior ophthalmic veins. The superior ophthalmic vein will eventually drain into the cavernous sinus, and the inferior ophthalmic vein will drain into the pterygoid venous plexus.[1][2]
It was previously thought that the lymphatic drainage of the medial upper eyelid drained medially along the angular artery, and the lateral upper eyelid lymph drained laterally to the preauricular and parotid nodes. There is a recent change regarding eyelid lymphatic drainage based on lymphoscintigraphy in human subjects. The upper eyelid lymphatics, including the levator palpebrae superioris muscles, are believed to drain entirely laterally to the preauricular/parotid lymph nodes, then to the deep cervical lymph nodes (level II). From here, lymph drainage follows conventional drainage patterns.[3]
Nerves
Like most muscles of the orbital cavity, the levator palpebrae superioris receives innervation from the third cranial nerve, the oculomotor nerve. The nerve originates from a single caudal subnucleus within the oculomotor nucleus in the midbrain. The nerve exits the brainstem between the superior and posterior cerebellar arteries. Next, it traverses the cavernous sinus laterally before exiting the cranium through the superior orbital fissure, where it divides into the superior and inferior branches. The superior branch crosses over the optic nerve and supplies direct innervation to the levator palpebrae superioris and the superior rectus muscles.[2] Due to the innervation originating from a single subnucleus, a single lesion can result in bilateral ptosis.[4]
Muscles
The levator palpebrae superioris has strong associations with the superior rectus muscle, superior tarsal muscle (Müller muscle), and orbicularis oculi. The superior branch of the oculomotor nerve dually innervates the superior rectus muscle and levator palpebrae superioris muscles, allowing synchronous elevation of the upper eyelid during upward gaze.[5]
The location of the superior tarsal muscle is posterior to the levator aponeurosis extending from the inferior aspect of the levator palpebrae superioris to the superior aspect of the tarsal plate. It is sympathetically innervated and assists with eyelid retraction.[8]
The levator palpebrae superioris is the major antagonistic muscle of the orbicularis oculi, whose primary function is eyelid closure.[9][10]
Physiologic Variants
The levator palpebrae superioris typically has one muscle belly. However, bipartite variances occur, and occasionally a bipartite muscle belly may be absent, resulting in an off-center unipartite levator palpebrae superioris. Also, accessory muscle slips may form. One accessory muscle slip variation is known as the "levator-trochlear muscle." Accessory muscle slips often receive their innervation from the oculomotor nerve.[11]
Regarding lymphatic drainage, occasionally, lymph would drain into an accessory or secondary preauricular/parotid lymph node or bypass this node and traverse directly to the deep cervical node.[3]
Surgical Considerations
The levator palpebrae superioris is often the directed target for correcting various causes of ptosis.[7] There are two main approaches to the levator palpebrae superioris when correcting ptosis: the anterior approach and the posterior approach. In the anterior approach, in the presence of levator aponeurosis dehiscence, the levator aponeurosis is re-inserted onto the tarsal plate. In congenital ptosis with a function of more than 4 mm, a more aggressive shortening of the levator aponeurosis and muscle is the procedure of choice.
In the posterior approach, the levator palpebrae superioris may similarly be advanced after making an incision at the top of the tarsal plate, or a Müllerectomy procedure may be carried out, in which conjunctiva and the Müller muscle are resected: histopathology has shown that this technique also removes some levator aponeurosis.
Weights (commonly gold and platinum) may also be surgically attached to upper eyelids to increase the weight of an upper eyelid and counter the action of the levator palpebrae superioris muscle. This surgery is useful in correcting excessive upper eyelid retraction and lagophthalmos (inability to close eyelids).[12]
Clinical Significance
Myogenic or neurogenic problems with the levator palpebrae superioris may occur, resulting in ptosis (drooping of the eyelid).
Myogenic ptosis may occur due to a failure of differentiation between the levator palpebrae superioris from the superior rectus muscle. During surgical correction, a thickened fibrous tissue is often identified instead of two differentiated muscles.[5] Also, various myopathies and eyelid trauma with subsequent scarring may cause myogenic ptosis. Additionally, ptosis may result from long-term hard contact lens use, which tends to result in disinsertion of the aponeurosis of the levator palpebrae superioris muscle.
Neurogenic ptosis due to inadequate levator palpebrae superioris innervation may occur from an oculomotor (cranial nerve III) nerve palsy, trauma, Guillain–Barré syndrome, and chronic inflammatory demyelinating polyneuropathy.[13][14][15]
Congenital ptosis may occur with dystrophy of the muscular component of the levator muscle, which shows fatty infiltration with poor levator function.