Continuing Education Activity
The Triple Arthrodesis is a versatile procedure useful in many pedal conditions. The term "triple" arthrodesis refers to a fusion procedure of three joints of the hindfoot and midfoot, the subtalar joint (talus and calcaneus), the talonavicular joint, and the calcaneocuboid joint. Due to the procedure's predictability, it is often used as a definitive treatment for many pedal deformities and offers patients the ability for pain-free, propulsive gait. It is not without its disadvantages; however, the loss of range of motion afterward may make other procedures a more prudent choice. In this activity, we will discuss the indications, anatomy, and the procedure itself.
Objectives:
- Identify the anatomical structures, indications, and contraindications of the triple arthrodesis.
- Describe the equipment, personnel, preparation, and technique in regards to the triple arthrodesis.
- Review the potential complications and clinical significance of the triple arthrodesis.
- Summarize interprofessional team strategies for improving care coordination and communication to advance the triple arthrodesis and improve outcomes.
Introduction
The triple arthrodesis is a versatile procedure useful in many pedal conditions and gait disturbances. The term "triple" arthrodesis refers to a fusion procedure of three joints of the hindfoot; the subtalar joint (talus and calcaneus), the talonavicular joint, and the calcaneocuboid joint. Due to the procedure's predictability, it is often used as a definitive treatment for many pedal deformities and offers patients the ability for pain-free, propulsive gait. In one study following patients who underwent a triple arthrodesis, 95% of patients were satisfied with the outcome after 44 years.[1] It is not without its disadvantages; however, the loss of range of motion afterward may make other procedures a more prudent choice.
Anatomy and Physiology
The most common approach to a triple arthrodesis is a double incision, one lateral incision, and one medial. As such, many structures are encountered during dissection and fixation. The most common structures encountered are discussed here. Laterally, nerves encountered are the sural and intermediate dorsal cutaneous nerve. Vascular structures encountered on the lateral incision include the artery of the tarsal sinus and venous connections supplying the extensor digitorum brevis.[2] Muscle and tendons encountered laterally are the peroneal tendons, extensor digitorum brevis muscle belly, and the peroneus tertius tendon. Medially the posterior tibial tendon is commonly encountered on its distal insertion. Depending on the technique, the deltoid artery and the artery of the tarsal canal may be encountered medially, as well as the great saphenous vein and its tributaries.[2]
There has been a discussion of a single medial incision approach with sparing of the calcaneocuboid joint for hindfoot arthrodesis (called a "medial double").[3] The advantages of this include avoiding lateral structures, avoiding non-union of the calcaneocuboid joint, decreased OR time, and decreased operating costs.[4][5] The disadvantages of this approach may be increased dissection, damaging the vasculature supplying the talar body.[2]
Indications
The triple arthrodesis is considered a definitive procedure for many pedal deformities and gait disturbances. Conditions it may be performed in include [6]:
- End-stage flatfoot deformities due to loss of soft tissue structures or joint adaptive changes of surrounding joints and pain
- Degenerative or Posttraumatic Arthritis due to pain
- Cavus foot deformities due to joint adaptive changes of surrounding joints and pain
- Charcot arthropathy after coalescence with risk for ulceration, or an apropulsive gait.
- Tarsal coalitions due to pain or degeneration of the ankle joint/surrounding joints
- Residual clubfoot deformities causing pain, joint degenerative disease or an apropulsive gait
- Certain neurological conditions resulting in neuromuscular imbalances and an apropulsive gait[7][1][8]:
- Charcot-Marie-Tooth
- Poliomyelitis
- Friedreich ataxia
- Spina bifida
- Cerebral palsy
Many conditions may be treated using other motion-preserving procedures, so the decision to perform the triple arthrodesis is always dependant on patient condition, disease progression, and surgeon preference.
Contraindications
Absolute contraindications to the triple arthrodesis include the presence of an active infection, acute Charcot arthropathy, arterial insufficiency, and others. Acute Charcot arthropathy can be determined via physical exam with possible bounding pedal pulses, increased lower extremity temperature, localized edema, and loss of protective sensation. Additionally, a positive history of neuropathy, radiographs showing disorganized osteolysis and lab markers such as increased ESR increase the likelihood of this diagnosis. Relative contraindications include uncontrolled comorbidities, presence of ankle arthritis, lack of trial of conservative therapy, and others. As with any procedure, careful patient selection and management of post-operative goals must take place to achieve an optimal outcome.
Equipment
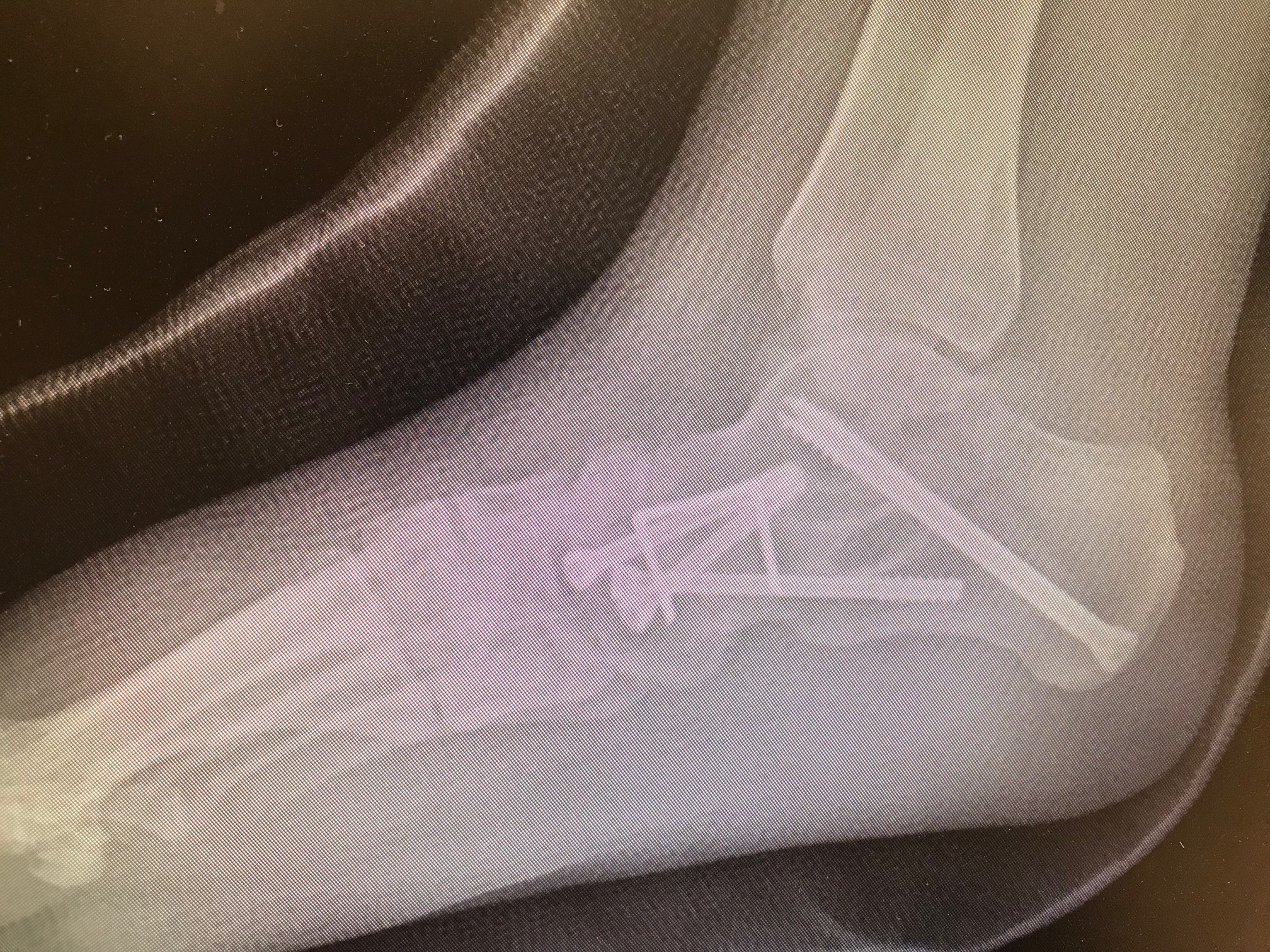
Equipment for the triple arthrodesis includes standard hardware for most arthrodesis procedures of the rearfoot and ankle. Screws from 6.5 mm to 8mm screws may serve for fixation of the subtalar joint, 4.5 mm screws may be used to fixate the midtarsal joints. Specialty equipment from many manufacturers exists, include plates and staples for the midtarsal joint. A thigh tourniquet is used for hemostasis during the procedure, and intraoperative fluoroscopy is recommended for confirmation of joint positioning and proper fixation. A distraction device such as a lamina spreader or Hintermann distractor may be useful.
Personnel
The procedure may be performed by a single surgeon, although a team approach ensures optimal patient outcomes. Perioperative nursing team, anesthesia team, and a radiology technician are also required. Post-procedure evaluation by physical therapy can assist in achieving patient long term pain relief and functional goals.
Preparation
A full biomechanical evaluation is crucial to optimal success. The ankle joint must be evaluated to see if an adequate range of motion exists to support an arthrodesis of the midfoot. The entire lower extremity must also be assessed to plan for proper intra-op and post-op positioning of the foot. This process involves a gait analysis with both the knee, ankle, and foot position evaluated.
Typically, the foot upon weight-bearing and in the progression of gait abducts approximately 10 to 15 degrees. If the knee is rectus with the foot abducted 15 degrees, it may be advisable to abduct the foot in its final position to 30 degrees; this would be 15 degrees abduction from the line of gait. However, if the knee is laterally positioned 15 degrees during the base of gait, it may be advised to position the foot in a rectus position.
Pre-operative radiographs include a weight-bearing dorsoplantar, medial oblique, and lateral view. These views can help assess overall joint quality, joint positioning needing to be corrected to obtain a rectus foot, and potential wedging or required grafting during the procedure. A calcaneal axial view may also be obtained to assess the degree of correction in regards to calcaneal valgus or varus. If questioning the integrity of the subtalar joint, one can get a CT scan to evaluate.[4] Alternatively, in-office weight-bearing CT scans are gaining in popularity to assess. Other imaging modalities that are obtainable include an MRI for evaluation of soft tissue structures, including the posterior tibial tendon, DEXA scan in the assessment of osteoporosis, or scanogram in the evaluation of limb length deformities. The decision for performing the surgery has its basis on both the patient's complaint of pain, overall disease progression, gait analysis, and radiographs.
Adequate patient counseling must take place before the procedure. With the fusion of the joints of the rearfoot, the patient will have difficulty walking on uneven surfaces, possible difficulty going downstairs, and a change in gait pattern. Patients must know that the post-procedure recovery may take six months to a year until fully recovered.
Technique or Treatment
The patient is positioned supine with a thigh tourniquet. General anesthesia is recommended.
The procedure begins laterally, careful to avoid the sural and intermediate dorsal cutaneous nerve, starting at the distal tip of the fibula and carried until the base of the fourth and fifth metatarsal. The incision is continued deep, until the arrival of the fascia overlying the extensor digitorum brevis muscle. A communicating branch of the sural nerve to the intermediate cutaneous branch can be encountered at this point and may have to be sacrificed to proceed. The extensor digitorum brevis then gets reflected off of its origination on the sinus tarsi. Peroneal tendons may be retracted plantarly.
The sinus tarsi may then be identified and excavated. Fibrofatty tissue in the sinus tarsi (Hoke's tonsil) must be removed for adequate exposure of the subtalar joint. All subtalar joint attachments must be released, including the interosseous ligament, to expose the anterior and middle facets.
Following the former incision distally, the calcaneal cuboid joint will be identified, and its dorsal ligaments must be released.
Following this, the medial incision will be placed between the medial gutter of the ankle and extended to the inferior aspect of the navicular. The great saphenous vein is often in this area and retractable superiorly. The capsular tissue of the talonavicular joint can be incised in line with the incision, leaving the attachment of the posterior tibial tendon intact. A cobb elevator is often useful in exposing the entire aspect of the joint.
Resection of the talonavicular joint can be performed using a variety of methods. Curettes or osteotomes may be used for cartilage resection and exposure of subchondral bone, maintaining the original contour of the joint. Adequate resection of cartilage and fenestration of the bone is crucial to ensure satisfactory osseous union.
Once the talonavicular joint is prepped, resection then continues at the calcaneocuboid joint. Once again, curettes or osteotomes are options, or a sagittal saw can be employed. If transverse plane deformity of the foot exists, a wedge of the calcaneus can be taken for correction.
Finally, the subtalar joint gets prepped for arthrodesis. The posterior facet can be prepped using curettage, osteotome, or a rotary burr to ensure adequate subchondral bone exposure. If the middle facet has been exposed, it too can be resected using this method. If a bone graft is employed for wedging, it can be placed for deformity correction.[4]
After prepping all joints, the talonavicular joint can undergo manual manipulation and then fixated temporarily using Kirschner wires or Steinmann pins. Following this, the subtalar joint and calcaneocuboid can be temporarily fixated using the same methods.
Ensuring the foot is in the optimal position for fusion, the subtalar joint is then permanently fixated. For fixation, screws can be used from a posterior and lateral angle on the calcaneus extending to the dorsal medial aspect of the talus. The talonavicular joint can then be fixated using screws from a distal and inferior aspect of the navicular into the head of the talus. The calcaneocuboid joint can finally be fixated utilizing a variety of hardware options.
The final position of the foot should be the following: heel in neutral to slight eversion, midtarsal joint in slight valgus.
Incisions are then irrigated and closed using anatomically layered closure. Skin closure can be through many methods. A drain may be used to prevent hematoma formation. Patients are typically placed in a splint and are non-weight bearing following the procedure.[9]
Complications
Complications after a triple arthrodesis include:
- Wound dehiscence, possibly due to aggressive tissue handling techniques or arterial insult; this is manageable via aggressive post-operative wound care.
- Pseudo or non-union of arthrodesis sites may occur, possibly due to improper joint resection or lack of rigid internal fixation. Further immobilization post-operative, bone stimulators, or a repeat procedure may be performed to correct.
- The most common joint for non-union in a triple arthrodesis is the talonavicular joint.[10]
- Hardware failure, possibly due to improper patient immobilization after surgery or due to non-union. If asymptomatic, no further management may be needed; however, a repeat procedure may necessary.
- Infection managed by antimicrobial therapy
- Vascular disruption to the talus due to arterial insult during dissection.[2] Although rare, this may result in osteonecrosis of the talus resulting in the need for ankle fusion, talectomy, or bone grafting.
- Early osteoarthritis of the ankle joint due to the improper final position of the arthrodesis sites.[11] If progressing and in the presence of pain, an ankle fusion may be necessary.
Clinical Significance
Triple arthrodesis is useful in many pedal conditions and gait disturbances. Due to the procedure's predictability, it is often used as a definitive treatment for many pedal deformities and offers patients the ability for pain-free, propulsive gait. In one study following patients who underwent a triple arthrodesis, 95% of patients were satisfied with the outcome.[1] It is not without its disadvantages; however, the loss of range of motion afterward may make other procedures a more prudent choice. Many patients with end-stage pedal deformities may be candidates for this procedure.
Enhancing Healthcare Team Outcomes
Due to the prolonged nature of recovery after a triple arthrodesis, an interprofessional approach enhances patient outcomes. In the immediate post-operative stage, identification of infection through the use of laboratory personal and tests can be crucial for avoiding complications. Physical therapy and occupational therapy are both modalities that can be employed to ensure a patient remains safe as they are non-weight bearing on their extremity. Identification of patients better served at a skilled nursing facility can enhance patient safety.
Nursing, Allied Health, and Interprofessional Team Interventions
Post-operatively, patients should be receiving information regarding activity restrictions. If patients are not comfortable using crutches or other devices, a physical therapy consult is in order. Post-operative care should emphasize to the patient the need for icing, elevation, and other pain modalities. The patient and family members should have involvement to ensure compliance.[12]
Nursing, Allied Health, and Interprofessional Team Monitoring
The patient's airway and vital signs require monitoring in the post-operative state. Circulation to the affected extremity and sensory monitoring should take place in the immediate post-operative state, along with pain monitoring. A general assessment of the patient should take place before patient discharge.[12]