Continuing Education Activity
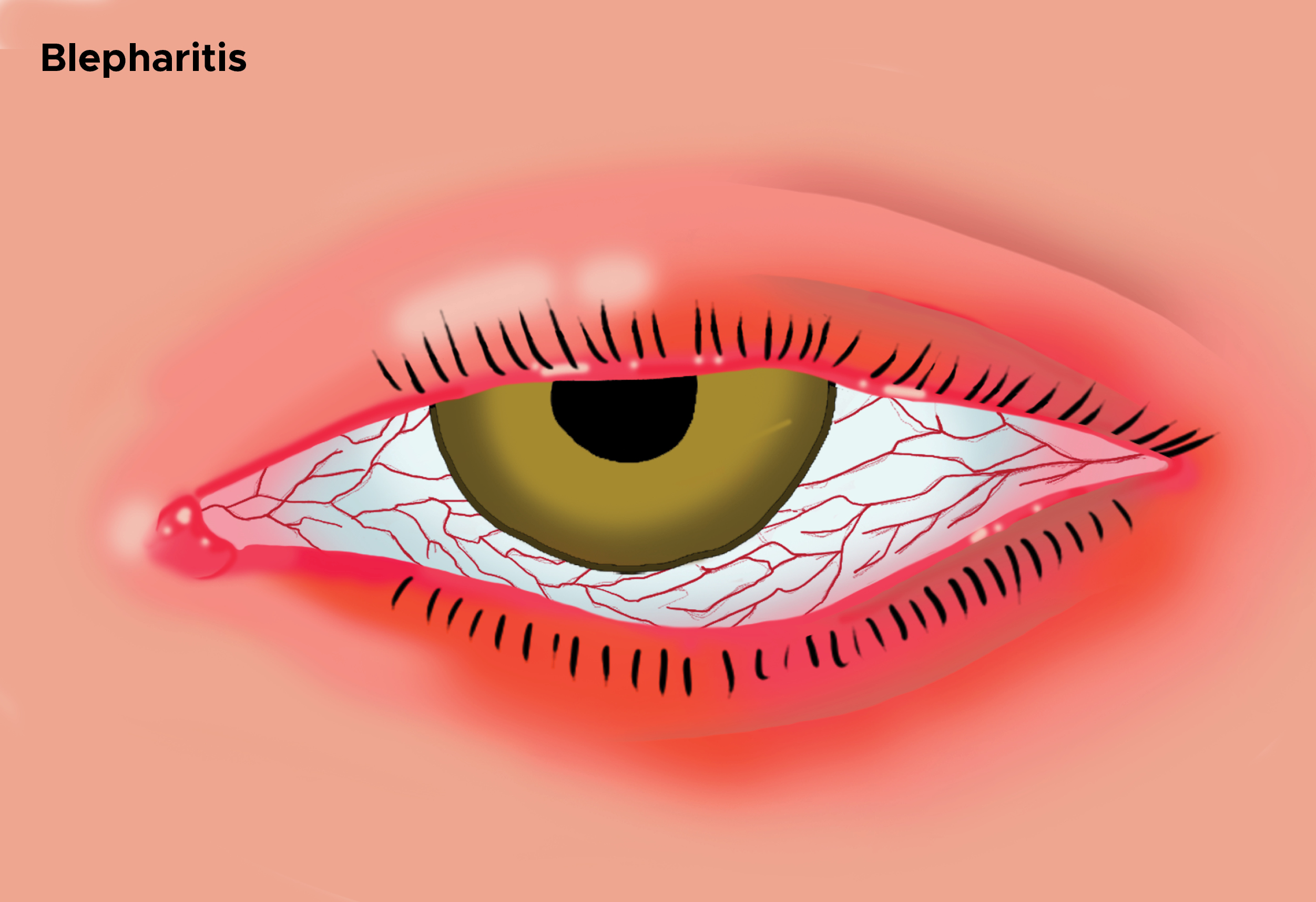
Blepharitis is an ophthalmologic condition where there is inflammation of the eyelid margins. The diagnosis is clinical and based on irritation of the lid margins with crusting and flaking of the lashes. This activity illustrates the evaluation and treatment of blepharitis and explains the role of the interprofessional team in managing patients with this condition.
Objectives:
- Describe the etiology of blepharitis.
- Identify the typical presentation of itching, burning and crusting of eyelids in patients with blepharitis.
- Outline the use of warm compresses and eyelid hygiene in the management of blepharitis.
- Summarize the importance of collaboration and communication among the interprofessional team members to enhance delivery of care for patients affected by blepharitis.
Introduction
Blepharitis is an ophthalmologic condition characterized by an inflammation of the eyelid margins. It can be acute or chronic with chronic being the more common form. It can further be defined by the location of the problem, anterior versus posterior. It usually presents with recurrent symptoms that may vary over time and involve both eyes. Blepharitis is a clinical diagnosis based on irritation of the lid margins with flaking and crusting of the lashes. The main treatment for blepharitis is good eyelid hygiene and elimination of triggers that exacerbate symptoms. Topical antibiotics may be prescribed. Patients refractory to these measures require referral to an ophthalmologist. The goal of treatment is to alleviate symptoms. Because most blepharitis is chronic, patients need to maintain a good hygiene regimen to prevent recurrences. While there is no definitive cure, the prognosis for blepharitis is good. Blepharitis is a more symptomatic condition than a true health threat.[1][2][3][4]
Etiology
Causes of blepharitis differ depending on whether it is an acute or chronic process and in the case of chronic the location of the problem. Acute blepharitis may be ulcerative or nonulcerative. An infection causes ulcerative blepharitis. This is usually bacterial and most commonly staphylococcal. A viral etiology such as infection with Herpes simplex and Varicella zoster is also possible. Nonulcerative is usually an allergic reaction such as atopic or seasonal. Its location best classifies the chronic form of blepharitis. In anterior blepharitis, an infection, usually staphylococcal, or seborrheic disease process is involved. Individuals frequently have seborrheic dermatitis of the face and scalp. Also, anterior blepharitis may be associated with rosacea. Meibomian gland dysfunction causes posterior blepharitis. The glands over-secrete an oily substance becoming clogged and engorged. Commonly, this is associated with acne rosacea, and hormonal causes are suspected. Both anterior (Demodex folliculorum) and posterior (Demodex brevis) blepharitis may be caused by a Demodex mite. Their role is not well-established since asymptomatic individuals have also been found to harbor the mites at approximately the same prevalence.[5][6][7]
Epidemiology
Blepharitis is not specific to any group of people. It affects people of all ages, ethnicities, and gender. It is more common in individuals older than the age of 50. The total number of cases in the US at any one time is not known. In a 2009 US survey, 37% of patients seen by an ophthalmologist and 47% of patients seen by an optometrist had signs of blepharitis. A recent study carried out over a ten year period (2004 through 2013) in South Korea determined the overall incidence to be 1.1 per 100 person-years. This increased with time and was higher in female patients. The overall prevalence for patients over 40 years of age was 8.8%.
Pathophysiology
The exact pathophysiology of blepharitis is not known. The cause is most likely multifactorial. Causative factors include a combination of chronic low-grade bacterial infections of the ocular surface, inflammatory skin conditions such as atopy and seborrhea, and parasitic infestations with Demodex mites.
History and Physical
Patients with blepharitis typically describe itching, burning, and crusting of the eyelids. They may experience tearing, blurred vision and foreign body sensation. In general, symptoms tend to be worse in the morning with crusting of the lashes being most prominent upon waking. The symptoms tend to affect both eyes and can be intermittent. The physical exam is best performed using a slit lamp. In anterior blepharitis, slit lamp exam reveals erythema and edema of the eyelid margin. Telangiectasia may be present on the outer portion of the eyelid. Scaling can be seen at the base of the eyelashes forming "collarettes." Also, loss of lashes (madarosis), depigmentation of lashes (poliosis), and misdirection of lashes (trichiasis) may be seen. In posterior blepharitis, the meibomian glands are dilated, obstructed, and may be capped with oil. Secretions from these glands may appear thick, and scarring of the lid may be present in the area around the glands. In all types of blepharitis, the tear film may show signs of rapid evaporation. This is best evaluated measuring the tear break-up time. A slit lamp exam is performed, and fluorescein dye is placed in the eye. The patient is asked to blink fully then maintain an open eye for 10 seconds. The tear film is examined for breaks or dry spots under cobalt blue light. There is general agreement that a tear break-up time less than 10 seconds is considered abnormal.
Evaluation
Blepharitis is a clinical diagnosis. No specific diagnostic testing beyond the history and physical exam is required. Individuals who fail treatment for chronic blepharitis should undergo biopsy of the lid to exclude carcinoma especially in cases of eyelash loss.
Treatment / Management
Eyelid hygiene remains the mainstay of treatment and is effective in treating most cases of blepharitis. Warm, wet compresses are applied to the eye for 5 to 10 minutes to soften eyelid debris, oils, and also to dilate meibomian glands. Immediately following this, the eyelid margins should be washed gently with a cotton applicator soaked in diluted baby shampoo to remove scale and debris. Care should be taken not to use too much soap since it can result in dry eyes. Individuals with posterior blepharitis, benefit from a gentle massage of the eyelid margins to express oils from the meibomian glands. A cotton applicator or finger is used to massage the lid margins in small circular patterns. During symptomatic exacerbations of blepharitis, eyelid hygiene needs to be performed two to four times daily. In patients with chronic blepharitis, a lid-hygiene regimen needs to be maintained daily for life, or irritating symptoms will recur. In addition, eye makeup needs to be limited and all triggers removed. Underlying conditions should be treated.[8][9][10][11]
Topical antibiotics should be used in all cases of acute blepharitis and cases of anterior blepharitis. They have been found to be useful in symptomatic relief and eradicating bacteria from the lid margin. Topical antibiotic creams like bacitracin or erythromycin can be applied to the lid margin for 2 to 8 weeks. Oral tetracyclines and macrolide antibiotics may be used to treat posterior blepharitis not responsive to eyelid hygiene or associated with rosacea. These oral antibiotics are used for their anti-inflammatory and lipid regulating properties.
Short courses of topical steroids are beneficial in patients with ocular inflammation. Recent trials have shown that antibiotics and corticosteroids can produce significant improvements in symptoms. These often are prescribed as a combination topical treatment in patients who have failed eyelid hygiene treatment.
In patients who are felt to have significant Demodex infestations, tea tree oil eyelid and shampoo scrubs have been shown to be beneficial when used for a minimum of 6 weeks.
Recent new therapies have become available for the treatment of blepharitis. Thermal pulsation therapy (LipiFlow device) applies heat to both the anterior and posterior surfaces. Pulsations gently remove debris and crustings from the meibomian glands. MiBoFlo is a thermal therapy applied to the outside of the eyelids. BlephEx is a rotating light burr used to remove debris from meibomian gland orifices. This allows better flow of oils and improved response to heat therapies. The Maskin probe is a stainless steel probe applied to an anesthetized meibomian gland orifice. A light electrical current is applied to the gland to facilitate oil secretion. While some small trials have shown promise, further clinical trials are needed to establish the efficacy of these treatments.
Differential Diagnosis
- Contact lens complications
- Epidemic keratoconjunctivitis
Pearls and Other Issues
While rarely sight-threatening, blepharitis can result in eyelid scarring, excessive tearing, hordeolum and chalazion formation, and chronic conjunctivitis.The development of keratitis and corneal ulcers can result in vision loss.
Blepharitis is a chronic condition characterized by exacerbations and remissions. While symptoms may be improved, there is rarely a cure.
Enhancing Healthcare Team Outcomes
Blepharitis is managed by an interprofessional team that consists of a nurse practitioner, primary care provider, ophthalmologist and the internist. Blepharitis is characterized by an inflammation of the eyelid margins, which can be acute or chronic. The main treatment for blepharitis is good eyelid hygiene and elimination of triggers that exacerbate symptoms. Topical antibiotics may be prescribed. Patients refractory to these measures require referral to an ophthalmologist. The goal of treatment is to alleviate symptoms. Because most blepharitis is chronic, patients need to maintain a good hygiene regimen to prevent recurrences. While there is no definitive cure, the prognosis for blepharitis is good. Blepharitis is a more symptomatic condition than a true health threat. Most patients do respond to treatment but the condition is characterized by exacerbations and remissions. [12](Level V)