Introduction
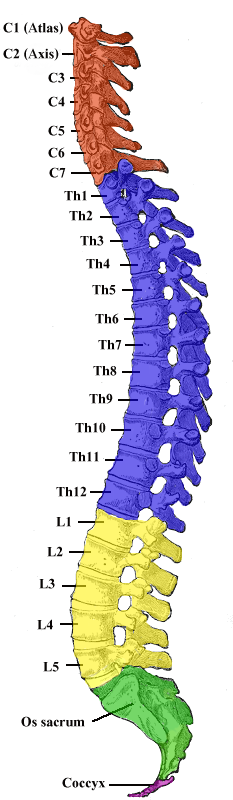
The spine, or vertebral column, is a segmental set of 33 bones and associated soft tissues in the subcranial portion of the axial skeleton. It is subdivided into 5 regions based on curvature and morphology: cervical, thoracic, lumbar, sacral, and coccygeal (see Image. Vertebral Column).
The cervical spine has 7 articulating vertebrae, whereas the thoracic has 12, and the lumbar has 5. Despite their similar morphology, these regions have variable flexibility, movement, and joint articulation, giving rise to the spine's S-shaped curvature.
Meanwhile, the sacrum and the coccyx are 2 sets of fused caudal vertebrae that convey no motion. The sacrum has 5 fused vertebrae, while the coccyx has 4.[1]
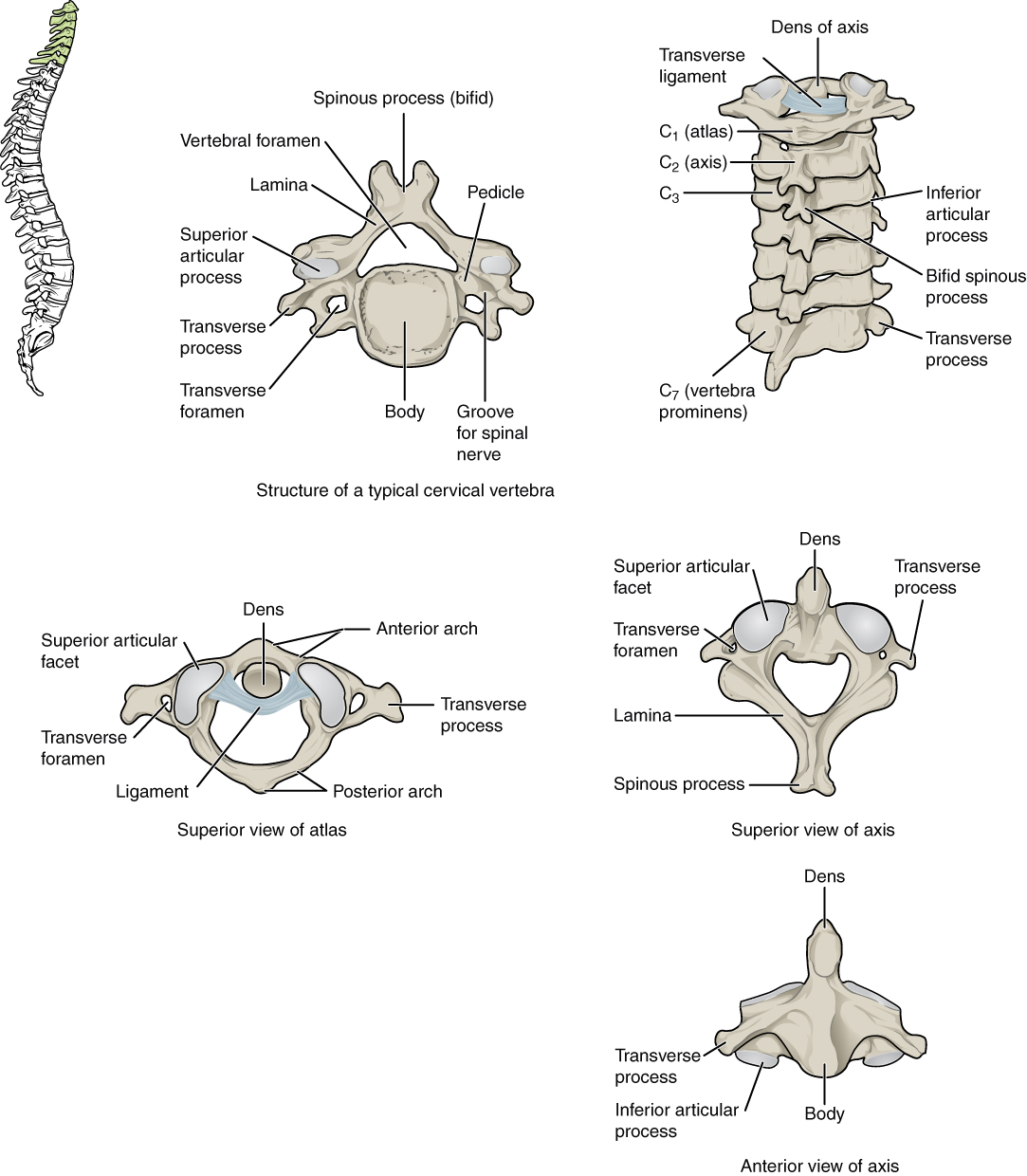
The cervical spine comprises 7 vertebrae (C1 to C7) and is divided into 2 major segments. The 2 most cephalad vertebrae, the atlas (C1) and the axis (C2), form the craniocervical junction (CCJ) together with the occiput. The 5 cervical vertebrae caudad, C3 to C7, comprise the subaxial spine and are referred to by number (see Image. Cervical Vertebrae). The cervical spine supports the weight of the cranium and head and neck motion.
Structure and Function
Typical vertebrae have hallmark anatomic structures that are conserved across the cervical, thoracic, and lumbar regions. Generally, each vertebra has a ventral vertebral body with mostly trabecular (cancellous) bone and a denser, mostly cortical dorsal vertebral arch.
The vertebral body is the main site of intervertebral articulation and load-bearing. Each vertebral body is linked to the next by an intervertebral disk.
The dorsal arch typically consists of a pair of pedicles arising from the dorsal vertebral body, which unite dorsally by their flat laminae. The spinous process arises as a dorsal projection from the midline fusion of the laminae. The pedicles, laminae, and dorsum of the vertebral body form the vertebral foramen, a complete osseous ring enclosing the spinal cord. The vertebral canal, which houses the spinal cord and its associated vascular structures, forms from connecting the vertebral foramina.
The transverse processes extend posterolaterally from the junctions of the laminae and pedicles. The 2 superior and 2 inferior articular processes also project from the junctions of the laminae and pedicles. In the cervical spine, the costal process becomes the anterior part of the transverse process, enclosing the vertebral artery foramen.[2]
Unique Features of the Cervical Spine
The cervical vertebral bodies are relatively smaller than their thoracic and lumbar counterparts due to the relatively lighter load at this spinal level. Consequently, the cervical spine is also more mobile, making it appropriate for supporting head and neck motion. However, the increased mobility and flexibility carry a higher spinal cord injury risk in this region.
Despite having most of the typical vertebral hallmarks, structural variability exists among the 7 cervical vertebrae. For instance, C2 to C6 have bifid spinous processes, but C7 has a larger, singular spinous process, and C1 has none. The C7 spinous process is called "vertebra prominens," which is palpable at the neck's base and similar to thoracic spinous processes. The C1 vertebra has a posterior tubercle instead of a spinous process.
The cervical vertebrae also have several anatomic variations. For example, all transverse processes have transverse foramina that, when connected, protect the vertebral arteries traveling at both sides of the neck. However, the C7 transverse foramina may be small or absent in some individuals.[3]
The Upper Cervical Spine – The Atlas (C1) and the Axis (C2)
The atypical cervical vertebrae C1 and C2 make up the upper cervical spine.
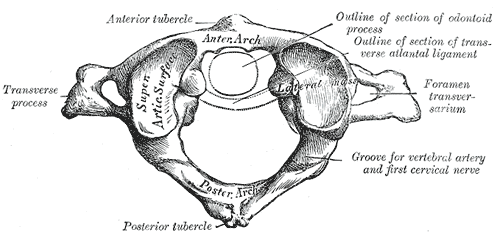
The C1 vertebra, aka the atlas, supports the skull at the atlanto-occipital joint (see Image. First Cervical Vertebra). Due to its unique role, C1 has features not shared with the rest of the spine. First, the vertebral body is absent, allowing the ring-shaped C1 to accommodate the spinal cord as it exits the foramen magnum. Second, C1's concave, medially oriented articular facets make it suitable for receiving the occipital condyles to form the atlanto-occipital joint. The atlanto-occipital joint transmits the head's weight to the spine, contributes greatly to the neck's flexion and extension, and limits the occiput's lateral displacement. Strong soft-tissue ligaments further stabilize the joint.[2][4]
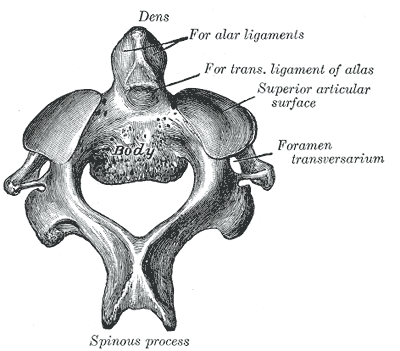
The C2 vertebra, aka the axis, is the primary weight-bearing bone of the upper cervical region(see Image. Second Cervical Vertebra). C2's hallmark feature is the odontoid process, aka dens, which is the bony projection extending cranially from its vertebral body. The odontoid process evolved from the body of C1 and serves as the principal attachment point for the soft tissues, stabilizing the atlantoaxial junction.
The atlantoaxial junction has 3 articulation points (see Image. Atlantoaxial Junction). The first is the midline atlanto-odontoid (atlanto-dental) joint, which permits the anterior arch of the atlas to pivot on the odontoid process. The other 2 are the atlantoaxial facet joints, which are lateral and involve C1's inferior facets and C2's superior facets. The atlantoaxial facet joints are fairly shallow, thus allowing significant motion. Compared to the atlanto-occipital joint, the atlantoaxial junction contributes more to the head and neck's rotatory motion than flexion or extension.[2][3][4][5]
The Subaxial Cervical Spine – C3 to C7
Compared to the upper cervical spine, all 5 subaxial cervical vertebrae share nearly identical morphological and functional features and have most of the typical vertebral structures. The C3 to C7 vertebrae possess uncinate processes, which are bony lateral vertebral body projections articulating at the Luschka joints to prevent vertebral listhesis.[3]
However, C7 has features not found in the other subaxial cervical vertebrae. As mentioned, the C7 transverse foramina are the smallest and sometimes absent. The vertebral arteries typically bypass the C7 transverse foramina and run cephalad starting from the C6 transverse foramina. C7 is also considered a transitional vertebra with a spinous process, inferior facets, and a larger vertebral body like the thoracic vertebrae.[6]
Embryology
The vertebral column originates from the somites, part of the paraxial mesoderm. More than 40 somite pairs develop craniocaudally alongside the notochord during the body axis elongation process. Local factors secreted by the notochord, neural tube, ectoderm, and visceral mesoderm induce the somites to undergo endothelial-to-mesenchymal transition (EMT) rapidly. The sclerotome, dermatome, and myotome appear after the transition. The mesenchymal sclerotome gives rise to the vertebral column, whereas the dermomyotome forms the muscles and overlying dermis.[7][8]
During the 4th week of embryogenesis, sclerotome cells develop around the notochord and the neural tube, signifying the initial formation of the true vertebral column and skull base. Column segmentation begins owing to the notochord's inductive influence. Cells that will give rise to the intervertebral discs' annulus fibrosus and nucleus pulposus coalesce between collections of sclerotome cells. The sclerotome aggregates form the vertebrae during the 6th week of embryogenesis.
Each vertebra initially has 3 ossification centers. However, 2 more ossification centers will develop during the first year of life and contribute to vertebral growth plate formation.[5][7][8] The ossification centers of the odontoid process are significant since they are often mistaken for pediatric fractures. The junction between the dens and C2's vertebral body fuses around 6 years of age. Meanwhile, the secondary odontoid ossification centers appear around age 3 but do not fuse to the cranial aspect of the dens until age 12.[5]
Blood Supply and Lymphatics
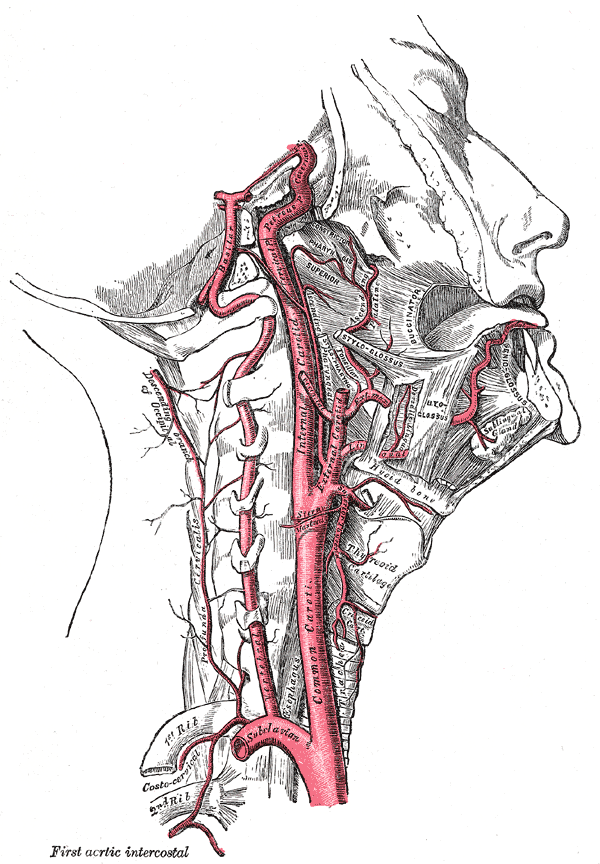
The vertebral arteries course cranially to the base of the skull distal to their bifurcation from the subclavian arteries (see Image. Internal Carotid and Vertebral Arteries). They progress past the C7 vertebrae anteriorly before entering the C6 transverse foramina. After exiting the C2 transverse foramina, the vertebral arteries bend laterally to enter the C1 transverse foramina, revert medially over the C1 arch, then enter the skull base. The main tributaries of the vertebral arteries, the cervical radicular arteries, supply blood to the cervical vertebral bodies.[9]
The carotid arteries also course through the cervical spine region. The right common carotid artery diverges from the brachiocephalic artery, while the left common carotid arises directly from the aortic arch. The common carotids then bifurcate into the internal and external carotids at the C3 vertebral level. The internal carotids do not perfuse any cervical spine structures despite their cervical location.[9]
Nerves
The cervical spine functions as the spinal cord's bony protection as it exits the cranium. Despite there being only 7 cervical vertebrae, there are 8 pairs of cervical nerves, termed C1 to C8. The first 7 cervical nerves exit the spine cranially to their associated vertebrae, while the 8th cervical nerve exits caudally to C7 (see Image. Cervical Nerves).
Direct innervation of the spinal column is highly complex. The sympathetic trunk, sympathetic rami communicantes, and perineural vascular plexus of the vertebral arteries lie in the cervical spine's ventral compartment. Meanwhile, the posterior aspect of the cervical spine receives innervation from the medial branch of the posterior primary rami. Coursing through the intervertebral foramen with the vertebral arteries are the vertebral nerves, which supply additional sympathetic innervation.[10]
Muscles
The cervical vertebrae serve as the origins and insertion points for the muscles supporting head and neck movement (see Image. Neck Muscles).
The erector spinae are deep back muscles traversing posteriorly along the entire spine. These muscles insert on the spinous and transverse processes of the cervical and upper thoracic vertebrae. The erector spinae provide postural support and assist in flexing and extending the vertebral column.
The posterior neck muscles and the suboccipital triangle are associated with the cervical vertebrae and enable the neck's extension, rotation, and lateral bending. The anterior neck's deep muscles also originate at various cervical landmarks before attaching to the cranium or 1st and 2nd ribs. The anterior neck muscles contribute to neck flexion, rotation, lateral bending, and stabilization of the skull.[4]
Physiologic Variants
The vertebrae initially arise from 3 primary ossification centers during embryogenesis: one in the centrum of the vertebral body and one in either vertebral arch. However, 5 ossification centers develop during the 1st year of life: one at either transverse process, one at the spinous process margin, and one each at the superior and inferior portions of the vertebral body. Bones ossifying from these 5 areas contribute to growth plate formation. Consequently, the growth plate's absence or asymmetry can contribute to cervical vertebral congenital defects.[8]
Surgical Considerations
The cervical spine is adjacent to vital head and neck structures. Most surgical procedures involving the cervical spine are performed via an anterior or posterior midline approach.
Anterior Surgical Approach
The anterior approach exposes the C2 to T1 vertebral levels and is indicated for anterior cervical diskectomy and fusion, corpectomy and fusion, cervical disk replacement, tumor resection, fracture, and infection. Surgeon preference dictates the side of access. A left-sided approach is often preferred, where the recurrent laryngeal nerve has a less variable course and poses a lower iatrogenic injury risk. Recurrent laryngeal nerve injury results in vocal cord paralysis and hoarseness. However, the clinical value of this approach remains controversial.
Superficial dissection transects the platysma muscle at the desired level. The sternocleidomastoid muscle is then identified and retracted laterally to protect the carotid sheath and expose strap musculature at the medial aspect. Superficial dissection must be performed carefully to avoid injuring the structures inside the carotid sheath.
Deep dissection retracts the trachea and esophagus medially, allowing access to the longus colli muscles. The longus colli muscles are then divided longitudinally and retracted laterally, exposing the anterior longitudinal ligament that overlies the vertebral bodies and disks. Careful retractor placement and dissection help avoid injury to the trachea, esophagus, and stellate ganglion, which are typically lateral to the longus colli muscles at the C6 level.
The stellate ganglion is a sympathetic structure. Injuries can lead to Horner syndrome, characterized by ptosis, anhydrosis, miosis, enophthalmos, and loss of ciliospinal reflex ipsilateral to the lesion.
A postoperative lateral cervical spine x-ray is obtained to assess soft tissue swelling. The soft tissue shadow anterior to the cervical spine should be less than 10 mm at the C1 level, less than 5 mm at C3, and less than 15 to 20 mm at C6.[2]
Posterior Surgical Approach
The posterior approach divides the paraspinal muscles dorsally at the midline. Adequate hemostasis and proper retractor placement ensure minimal blood loss. Access to the cervical spine's posterior elements is necessary during procedures like laminectomy, laminoplasty, foraminotomy, and posterior cervical instrumentation.
Upper cervical spine fractures are also most frequently accessed posteriorly. The unique anatomy of this spinal segment warrants careful consideration during surgical intervention. For example, pedicle screws may be safely used on C2 and C7 but not C3 to C6 because of their small size and proximity to the vertebral arteries. Lateral mass screw placement with radiographic navigation is an alternative, having a lower risk of injuring the vertebral arteries.
Posterior arch dissection during C1 lateral mass screw placement should not be exposed more than 1.5 cm away from the midline to minimize the risk of vertebral artery injury. To avoid the vertebral artery, the screw should be angled 10 to 15 degrees medially.[2]
Trans-articular screw placement at the C1-C2 level also risks vertebral artery injury as the screw must pass C2's pars interarticularis. C2 pedicle screw placement carries less vertebral artery injury risk but confers some risk to the internal carotid artery, depending on screw length.
In cases involving upper cervical spine fusion, surgeons must inform the patient about the risk of potential mobility reduction when rotating, flexing, or extending the cervical spine.[2]
Clinical Significance
Neck pain presents a significant socioeconomic burden. Studies estimate the prevalence of neck pain in the adult population to be between 10% and 30%, making it one of the leading causes of disability globally. Neck pain is often classified based on duration (acute, subacute, or chronic) and etiology (eg, mechanical, neuropathic, rheumatologic). Frequent neck pain is defined as having at least 3 neck pain episodes in a year.[3][11]
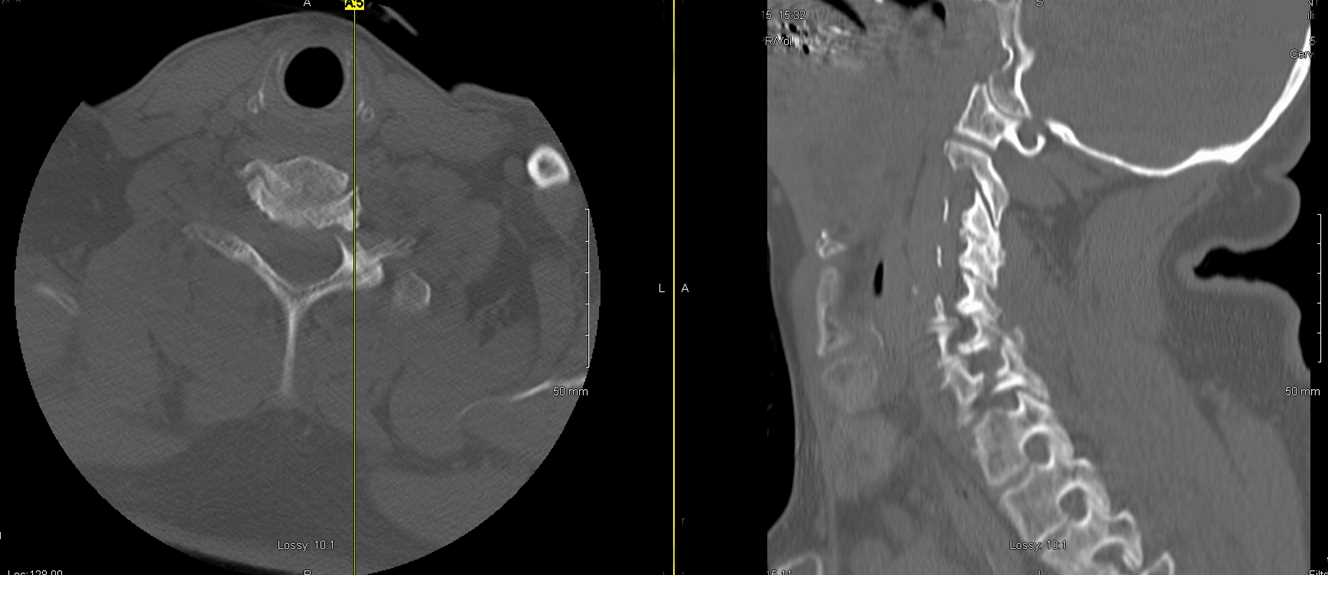
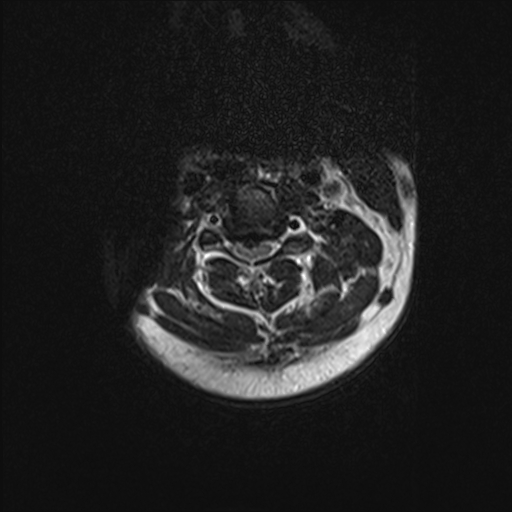
Acute neck pain often arises from trauma or sports injury. Fractures and dislocations are common and, in severe cases, may be fatal. Cross-table radiography and computed tomography (CT) scans are invaluable tools for assessing cervical fractures and other bone abnormalities (see Image. CT Scan of C6-C7 Fracture). In contrast, magnetic resonance imaging (MRI) is preferred for spinal cord or soft tissue evaluation (see Image. Cervical Spine MRI). Given the high neurological stakes, missed or incorrect diagnoses can have serious long-term costs. Regardless of location, the specific characteristics of cervical spine injury dictate the management.[11][12]
Subacute and chronic neck pain have diverse causes. Cervical facet arthritis is a common cause of mechanical neck pain. Neuropathic neck pain frequently has peripheral origins such as nerve root compression, intervertebral disk herniation, and spinal stenosis. A comprehensive history and physical examination can help differentiate between mechanical and neuropathic etiologies. Diagnostic imaging and further workup are necessary in some cases.[11]