Continuing Education Activity
Ankyloglossia, also known as tongue-tie, is a condition that impairs tongue movement due to a restrictive lingual frenulum. Multiple specialties within medicine and dentistry are involved in the evaluation and treatment of this condition. Ankyloglossia mainly impairs breastfeeding and has also been linked with speech disorders, malocclusion, and gingival recession. Management of ankyloglossia remains controversial. If surgical treatment is decided, frenotomy is the most common procedure. This activity reviews the available data regarding the etiology, epidemiology, and common clinical findings of ankyloglossia. It also describes the current evaluation and management strategies for patients with ankyloglossia; identifies the differential diagnoses, prognosis, and complications; and highlights the role of the interprofessional team in the management of ankyloglossia.
Objectives:
- Identify the signs and symptoms of ankyloglossia and assess the severity of the condition based on commonly used classification and grading systems.
- Apply evidence-based guidelines and practices for the diagnosis and management of ankyloglossia, considering the latest research and recommendations.
- Select suitable interventions for ankyloglossia management, such as referral for frenotomy, tongue exercises, or speech therapy, based on individual patient needs.
- Collaborate with other healthcare professionals, including lactation consultants, speech-language pathologists, and pediatricians, to provide comprehensive care for patients with ankyloglossia.
Introduction
Ankyloglossia, also known as tongue-tie, is a condition that concerns multiple specialties within medicine and dentistry. There is a lack of consensus regarding all aspects of the disease.[1] No definition, classification system, or diagnostic parameters has been generally accepted. Therefore, controversy exists concerning when to treat the condition, when it should be left untreated, and what intervention is best if managed. This activity reviews the available data regarding the etiology, epidemiology, and common clinical findings of ankyloglossia. It also describes the current evaluation and management strategies for patients with ankyloglossia and identifies the differential diagnoses, prognosis, and complications.
Definition
No standard definition of ankyloglossia has been agreed on. The International Affiliation of Tongue-Tie Professionals defines the lingual frenulum as a tissue remnant located in the midline between the tongue's ventral surface and the mouth's floor.[2] When the lingual frenulum limits the function of the tongue, it is called symptomatic tongue-tie or symptomatic ankyloglossia.[2]
In 2020, a group of otolaryngologists with expertise in managing tongue-tie formulated a clinical consensus statement. They agreed on a definition of tongue-tie as a "condition of limited tongue mobility caused by a restrictive lingual frenulum."[1] This panel of experts also acknowledged that professionals have been using the terms anterior and posterior ankyloglossia in recent years.[1]
Anterior ankyloglossia is classic ankyloglossia, where the frenulum attaches at or close to the tongue tip, limiting tongue mobility.[2] Notably, 'anterior ankyloglossia' and 'ankyloglossia' are interchangeable.[1] Diagnosis of posterior ankyloglossia remains a subject of controversy. Posterior ankyloglossia occurs when the frenulum attaches to the posterior aspect of the ventral surface of the tongue and restricts tongue mobility.[1] Some also use the term to refer to the submucosal tethering of the tongue.[1] Others consider posterior ankyloglossia normal frenulum attachment and attribute breastfeeding difficulties to other factors, like nipple anatomy, maternal milk production, and maternal experience.[2] Maxillary lip frenulum tethering has also been reported to affect breastfeeding.[2]
Classification and Assessment Tools
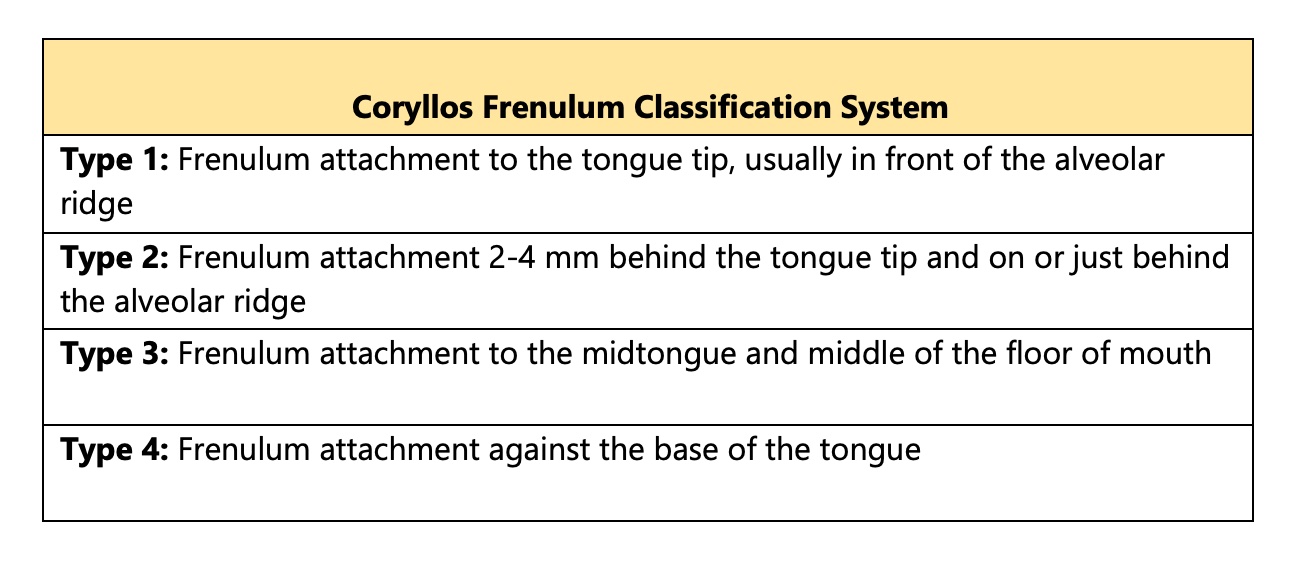
Various grading tools have been proposed. The Coryllos classification is useful to determine the type of frenulum, but it does not include the evaluation of function nor a criterion for ankyloglossia.[1] (See Table 1. Coryllos Lingual Frenulum Classification System).
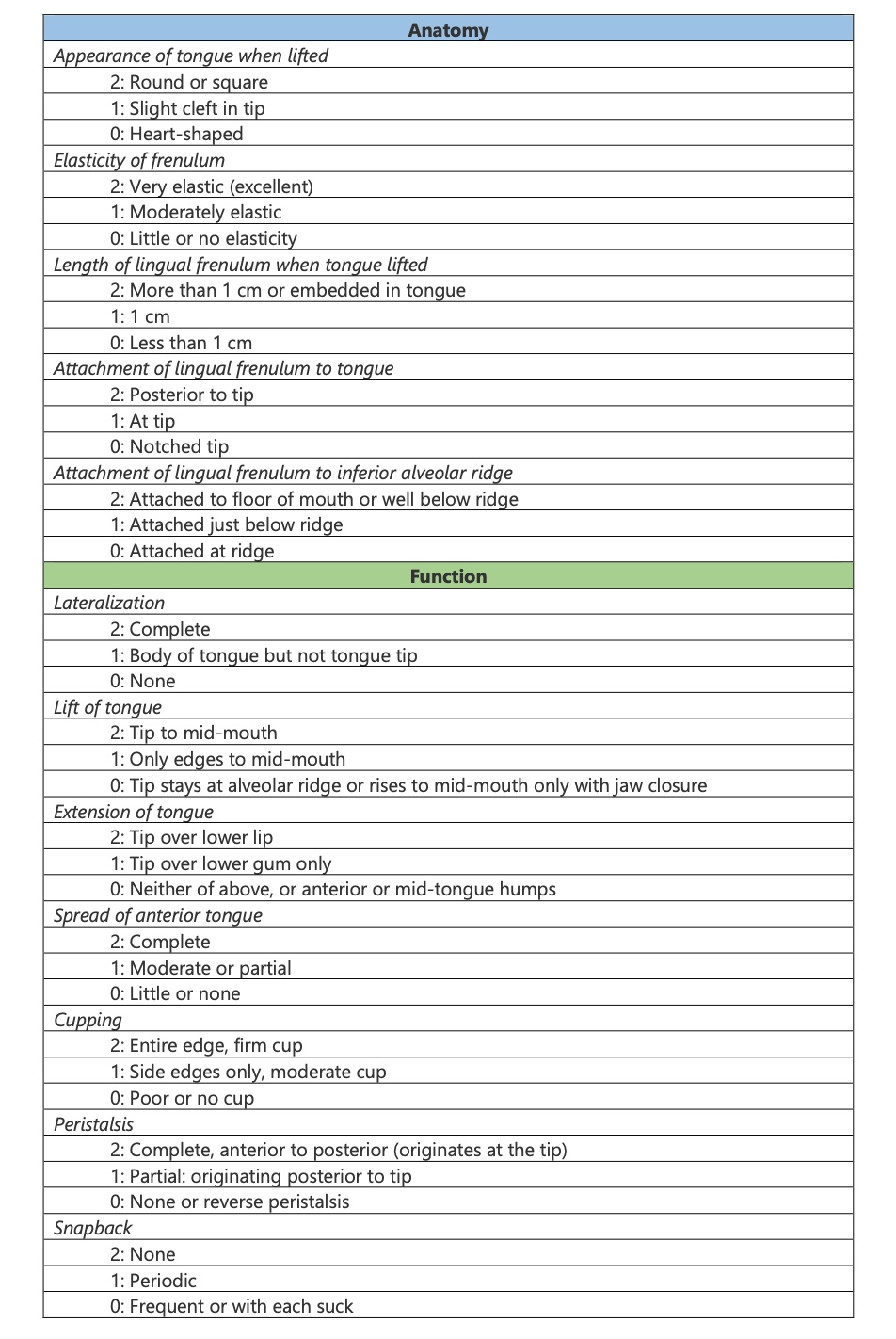
The Hazelbaker Assessment Tool for Lingual Frenulum Function (HATLFF) assesses frenulum anatomy and function and scores ankyloglossia.[1] [See Table 2. The Hazelbaker Assessment Tool for Lingual Frenulum Function (HATLFF)].[3] This tool uses 10 points for frenulum anatomy and 14 points for the function of the tongue. Surgery is not recommended if the function score is 14, regardless of the anatomy score. A function score of 11 is acceptable if the anatomy score is 10. A function score less than 11 means impaired function; frenotomy is recommended if management fails. Frenotomy is recommended when the anatomy score is less than 8.
Regardless of the evaluation tool used, it is essential to demonstrate restricted tongue movement and ascertain that the lingual frenulum exclusively causes this limitation.[1]
Etiology
The exact etiology of ankyloglossia remains unknown. An association between X-linked cleft palate syndrome has been reported.[4][5] Ankyloglossia has also been observed in rare syndromes, including Kindler, Opitz, and Van Der Woude.[6]
Despite this, tongue-tie is mainly seen in patients with no congenital pathologies or diseases.[6] There is evidence that tongue-tie could be transmitted genetically.[6] Furthermore, newborns from mothers who consume cocaine during pregnancy seem more predisposed to ankyloglossia.[7]
Epidemiology
The prevalence of tongue-tie ranges from 0.1% to 10.7%.[6] This is partly because of the lack of a single definition and the differences among investigators.[6] Also, an increase in the incidence of ankyloglossia was noticed in recent years, again mainly because of the several definitions of ankyloglossia being used by clinicians. This has led to overdiagnosing infants and children with tongue-tie and unnecessary surgery.[1][8]
Some less severe forms of tongue-tie may resolve spontaneously with time, explaining why its prevalence is higher in studies evaluating only newborns (1.72% to 10.7%) than in those investigating children, teenagers, and adults (0.1% to 2.08%).[6] Regarding sex, ankyloglossia seems more prevalent in males; no racial preference is observed.[6]
History and Physical
Symptoms of ankyloglossia usually manifest as breastfeeding difficulties and clinical findings in the mother and infant. Breastfeeding complications in the infant may appear as poor latching, constant loss of latch, irritability while breastfeeding, and poor weight gain.[2] The mother usually reports pain while breastfeeding, inadequate milk secretion, or incomplete emptying due to an insufficient infant suck.[2] Examination findings in the mother may include nipple infection, ulceration, or bleeding.[2] This can result in early abandonment of breastfeeding due to frustration, anxiety, and feeling of failure.[2]
The lingual frenulum can be attached to different areas of the tongue and alveolus.[2] A short or thick lingual frenulum may also affect the function of the tongue.[2] The examination must demonstrate tongue mobility restriction; usually, the tongue cannot be protruded beyond the vermillion border.[2] The tongue may also show a heart-shaped deformity and dimpling.[2]
Restricted tongue mobility may affect the pronunciation of consonants and the sounds “s, z, t, d, j, l, ch, zh, th, dg,” and “r.”[9][10][11] Nevertheless, a difference in pronunciation is not necessarily considered a speech disorder.[6] The link between speech disorders and ankyloglossia remains unclear.[12] Ankyloglossia and speech articulation difficulties are common among newborns and children, but an absolute connection between them could not yet be established.[12] There is a need for widely accepted grading systems and better-designed clinical studies.[12]
Mechanical complications have also been reported in adults with ankyloglossia, including difficulties with licking the lips, kissing, eating ice cream, and doing tricks with the tongue.[13] Discomfort under the tongue and tongue cuts from teeth have also been described.[13]
Ankyloglossia is linked to the development of malocclusion, particularly Class III malocclusion. Ankyloglossia's hypothesized association with mandibular prognathism and underdevelopment of the maxilla stems from the notion that the tongue's low position in affected patients exerts forward and downward pressure.[6] However, the evidence that tongue-tie contributes to malocclusion is limited, and this belief may be only based on speculation.[6]
Evaluation
Several factors, including ankyloglossia, can cause breastfeeding problems, but not all infants with tongue-tie necessarily have breastfeeding difficulties.[14] Results from randomized control trials demonstrate that many infants with different severities of ankyloglossia feed well without surgical treatment.[15][16] Since ankyloglossia is easily diagnosed on clinical examination is more commonly believed to be the cause of breastfeeding problems.[1]
Examining an infant with breastfeeding difficulties should not be limited to the lingual frenulum but should be widened to evaluate for other head and neck etiologies.[1] A lactation history from the mother must also be obtained.[1]
The infant must be assessed for an abnormal palate, maxilla, or mandible development; neurologic or cardiovascular disorders; and obstruction in the upper airways that could complicate feeding.[1] It is crucial to gather information regarding various lactation factors, such as the mother's breastfeeding experience, frequency and duration of breastfeeding, and the utilization of formula or pumping devices.[17] In addition to the aforementioned lactation aspects, it is essential to consider maternal factors such as typical discomfort during the initial weeks of breastfeeding, inadequate positioning and support while nursing, nipple anatomy, milk supply, and the possibility of breast infection.[1]
Some healthcare providers, including otolaryngologists and dentists who diagnose ankyloglossia, may occasionally possess limited knowledge about breastfeeding techniques and practices.[1] Inadequate breast positioning is, in most cases, the cause of breastfeeding difficulty; therefore, it is necessary to consult with a lactation expert who will provide lactation advice and support.[1]
Treatment / Management
Even though there is significant evidence that breastfeeding difficulty in infants with ankyloglossia can be improved by frenotomy, some do not benefit from the procedure.[1][15][18][19][20][21][22] Parents must be informed about this possibility before the infant undergoes surgery.[1] Caregivers must also be informed of conservative treatment options, including observation, lactation, and speech pathology consultation.[1]
Frenotomy is usually recommended in infants diagnosed with ankyloglossia experiencing breastfeeding difficulties after other conservative treatments have failed. Early release of the lingual frenulum will decrease the possibility that the mother abandons breastfeeding.[23] Notably, there is limited evidence to support that frenotomy is associated with positive outcomes in other issues besides breastfeeding.[24]
Relative contraindications to frenotomy in infants include neuromuscular disorder, hypotonia, retrognathia, and micrognathia, as a lingual frenotomy may aggravate glossoptosis, obstruct the airways, and complicate swallowing.[1]
It is essential to distinguish between 'frenotomy,' 'frenuloplasty,' and 'frenectomy,' as these terms are sometimes used interchangeably.[1] Frenotomy, also known as frenulotomy, is the incision of the lingual frenulum and is the procedure performed in infants.[1] Frenuloplasty involves cutting the lingual frenulum and repositioning the tissue; frenectomy refers to removing the lingual frenulum.[1]
Frenotomy involves holding the tongue up to tighten the frenulum, then cutting through the fascia-like tissue along a line parallel and close to the tongue. The cut is made in a single motion in less than a second. The infant is restrained by swaddling or in a Papoose board, with an assistant holding the child's head for better support. In a study of 200 infants undergoing frenotomy without analgesia, researchers found that 18% cried during and 60% after the procedure. In a study by Griffiths et al[25], the mean crying time for frenotomy was 15 seconds. Some physicians choose to give sucrose before the procedure to minimize and help with the pain. Placing topical anesthesia is not beneficial, and local anesthesia is contraindicated in infants.[1]
Risks and complications of frenotomy are uncommon but have been described. Rare complications include bleeding, airway obstruction, damage to surrounding structures, scarring, and oral aversion.[1] Bleeding is the most common and is usually resolved with local pressure. A family history of bleeding disorders should be assessed before the procedure, and in older patients, a history of bleeding should be elicited.
Differential Diagnosis
Breastfeeding difficulties can be caused by many other factors besides ankyloglossia.[1] In neonates experiencing problems with breastfeeding, it is crucial to rule out the following pathologies:
- Craniofacial pathologies, like retrognathia and cleft palate
- Nasal obstruction, like in piriform aperture stenosis and choanal atresia
- Airway obstruction, like bilateral vocal fold paralysis and laryngomalacia
- Laryngopharyngeal reflux
Patient morbidity and outcomes may worsen if these conditions are not identified and treated before deciding to perform a frenotomy.[1]
Prognosis
The natural history of ankyloglossia remains unknown. For those infants experiencing breastfeeding difficulties, a frenotomy is an acceptable option since it is a low-risk procedure likely to be beneficial for such patients.[2]
Complications
As previously mentioned, infants with ankyloglossia mainly experience breastfeeding difficulties, including poor latching, irritability while breastfeeding, and failure to thrive. Complications for the mother are pain while breastfeeding, deficient milk secretion, nipple ulceration, infection, or bleeding.[2]
Older children and adults with ankyloglossia may undergo mechanical limitations, like difficulty eating ice cream, licking their lips, and doing tongue "tricks."[13] Restricted tongue mobility may complicate the pronunciation of certain letters; however, the link between ankyloglossia and speech disorders remains controversial.[12] Furthermore, the role of tongue-tie in mandibular development, malocclusion, and gingival recession is still unclear.[2]
Deterrence and Patient Education
- Ankyloglossia must be diagnosed when there is a limitation in tongue mobility that can be isolated to the lingual frenulum.
- Not all tongue-ties require surgical management.
- When a newborn presents with breastfeeding difficulties, other causes must be ruled out.
- Inadequate position during breastfeeding is the most common cause of breastfeeding difficulties.
- First-time mothers and other patients experiencing breastfeeding challenges should be encouraged to seek guidance and support from a lactation expert to ensure appropriate assistance.
- Patients must be well informed about the risks and complications of frenotomy, particularly since the procedure may not resolve the breastfeeding problem.
Enhancing Healthcare Team Outcomes
The management of ankyloglossia concerns multiple specialties within medicine and dentistry. Ankyloglossia may be encountered by primary care clinicians, pediatricians, otolaryngologists, nurse practitioners, lactation nurses, speech consultants, and dentists.
The treatment of ankyloglossia has many controversies, which can be very confusing for parents who seek different opinions. The best approach for any healthcare worker encountering this issue is to weigh the benefits for the patient. Observation is the best treatment option if the condition is not causing any problems during the neonatal period. Once other potential causes of feeding difficulties have been excluded, a frenotomy can be presented as a possible treatment option. Frenotomy should only be performed by a trained and qualified healthcare provider.
When patients present with articulation problems, the decision-making process becomes more complex, and it is advisable to recommend evaluation and therapy with a speech pathologist. Overall, most patients benefit from observation. However, frenotomy is generally considered a low-risk procedure that can be performed in an outpatient clinic without anesthesia. It has the potential to improve breastfeeding difficulties and provide relief to the typically frustrated mother.[Level 2]